J Rheum Dis.
2022 Apr;29(2):123-128. 10.4078/jrd.2022.29.2.123.
A Case of Macrophage Activation Syndrome During the Treatment of Adult-onset Still’s Disease With Tocilizumab
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Soonchunhyang University College of Medicine, Cheonan, Korea
- 3Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2527552
- DOI: http://doi.org/10.4078/jrd.2022.29.2.123
Abstract
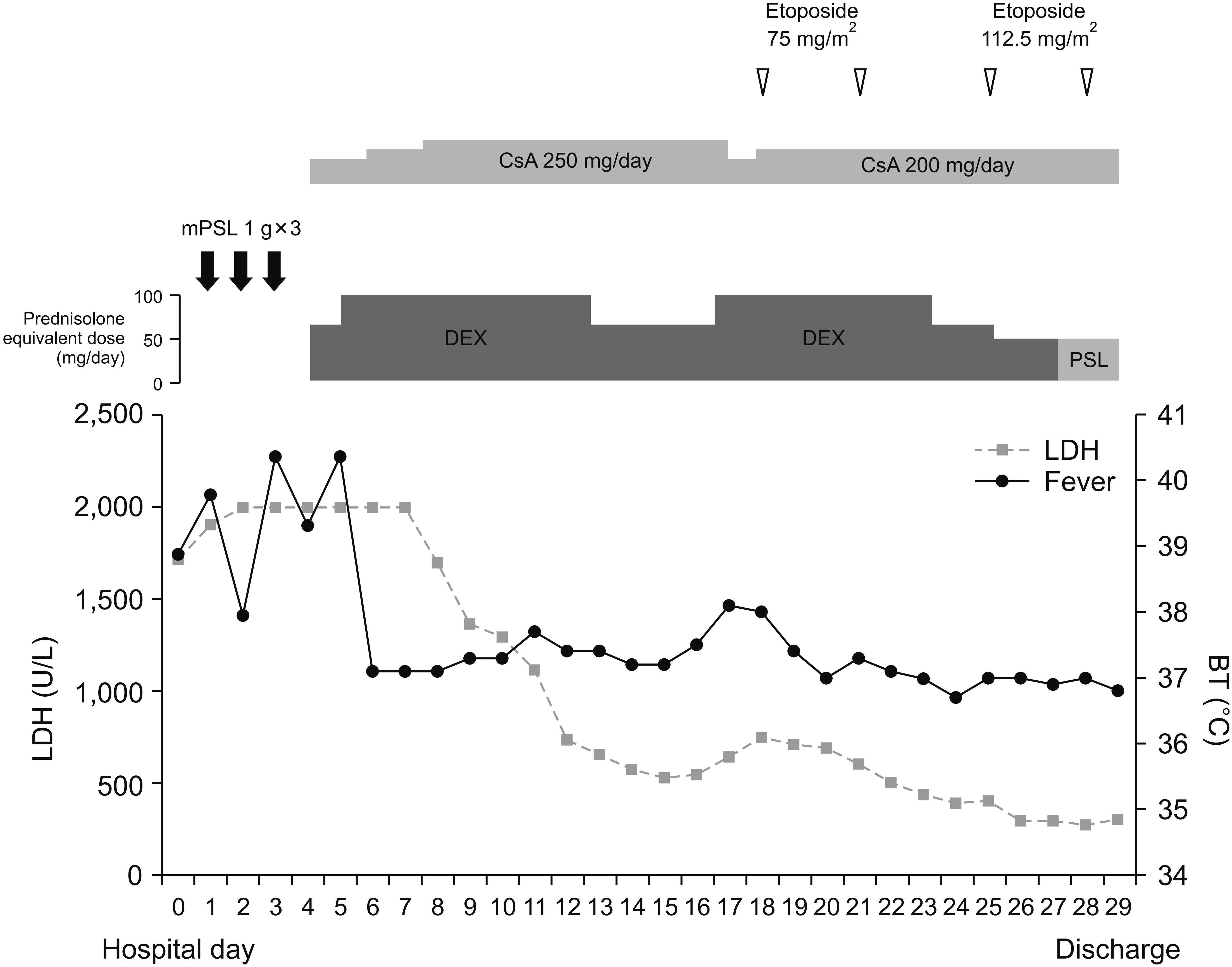
- Macrophage activation syndrome (MAS) is a fatal complication of adult-onset Still’s disease (AOSD). Although anti-cytokine agents have been recommended for refractory AOSD or complicated with MAS, MAS cases have been rarely reported during anticytokine treatment. Herein, we describe the first AOSD case complicated with MAS during the treatment with tocilizumab in Korea. Two years after tocilizumab maintenance therapy, high fever and hypertransaminasemia recurred. MAS was diagnosed based on hyperferritinemia, elevated soluble IL-2 receptor levels, and the presence of hemophagocytic histiocytes in the bone marrow. However, she had normal white blood cell counts and acute phase reactant levels. High-dose glucocorticoid and anakinra therapies were not effective, but her disease improved with etoposide. This case shows that tocilizumab may not prevent MAS development and can modify clinical features making it challenging to diagnose. Cytotoxic therapy such as etoposide may be required in MAS cases that develop during anti-cytokine therapy.
Keyword
Figure
Reference
-
1. Jamilloux Y, Gerfaud-Valentin M, Martinon F, Belot A, Henry T, Sève P. 2015; Pathogenesis of adult-onset Still's disease: new insights from the juvenile counterpart. Immunol Res. 61:53–62. DOI: 10.1007/s12026-014-8561-9. PMID: 25388963.
Article2. Banse C, Vittecoq O, Benhamou Y, Gauthier-Prieur M, Lequerré T, Lévesque H. 2013; Reactive macrophage activation syndrome possibly triggered by canakinumab in a patient with adult-onset Still's disease. Joint Bone Spine. 80:653–5. DOI: 10.1016/j.jbspin.2013.04.011. PMID: 23751410.
Article3. Shimizu M, Nakagishi Y, Kasai K, Yamasaki Y, Miyoshi M, Takei S, et al. 2012; Tocilizumab masks the clinical symptoms of systemic juvenile idiopathic arthritis-associated macrophage activation syndrome: the diagnostic significance of interleukin-18 and interleukin-6. Cytokine. 58:287–94. DOI: 10.1016/j.cyto.2012.02.006. PMID: 22398373.
Article4. Yokota S, Itoh Y, Morio T, Sumitomo N, Daimaru K, Minota S. 2015; Macrophage activation syndrome in patients with systemic juvenile idiopathic arthritis under treatment with tocilizumab. J Rheumatol. 42:712–22. DOI: 10.3899/jrheum.140288. PMID: 25684767.
Article5. Schulert GS, Minoia F, Bohnsack J, Cron RQ, Hashad S, KonÉ-Paut I, et al. 2018; Effect of biologic therapy on clinical and laboratory features of macrophage activation syndrome associated with systemic juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 70:409–19. DOI: 10.1002/acr.23277. PMID: 28499329.
Article6. Shimizu M, Mizuta M, Okamoto N, Yasumi T, Iwata N, Umebayashi H, et al. 2020; Tocilizumab modifies clinical and laboratory features of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 18:2. DOI: 10.1186/s12969-020-0399-1. PMID: 31924225. PMCID: PMC6954608.
Article7. Irabu H, Shimizu M, Kaneko S, Inoue N, Mizuta M, Nakagishi Y, et al. 2020; Comparison of serum biomarkers for the diagnosis of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis during tocilizumab therapy. Pediatr Res. 88:934–9. DOI: 10.1038/s41390-020-0843-4. PMID: 32184444.
Article8. Yamabe T, Ohmura SI, Uehara K, Naniwa T. 2021; Apr. 6. Macrophage activation syndrome in patients with adult-onset Still's disease under tocilizumab treatment: a single-center observational study. Mod Rheumatol. [Epub]. DOI: 10.1080/14397595.2021.1899565.
Article9. Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, et al. 1992; Preliminary criteria for classification of adult Still's disease. J Rheumatol. 19:424–30.10. Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. 2007; HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 48:124–31. DOI: 10.1002/pbc.21039. PMID: 16937360.
Article11. Martini A, Ravelli A, Avcin T, Beresford MW, Burgos-Vargas R, Cuttica R, et al. 2019; Toward new classification criteria for juvenile idiopathic arthritis: first steps, Pediatric Rheumatology International Trials Organization international consensus. J Rheumatol. 46:190–7. DOI: 10.3899/jrheum.180168. PMID: 30275259.
Article12. Ravelli A, Minoia F, Davì S, Horne A, Bovis F, Pistorio A, et al. 2016; 2016 classification criteria for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology Inter-national Trials Organisation collaborative initiative. Arthritis Rheumatol. 68:566–76. DOI: 10.1002/art.39332. PMID: 26314788.13. Wang R, Li T, Ye S, Tan W, Zhao C, Li Y, et al. 2020; Macrophage activation syndrome associated with adult-onset Still's disease: a multicenter retrospective analysis. Clin Rheumatol. 39:2379–86. DOI: 10.1007/s10067-020-04949-0. PMID: 32130578.
Article14. Iemoli E, Piconi S, Fusi A, Borgonovo L, Borelli M, Trabattoni D. 2010; Immunological effects of omalizumab in chronic urticaria: a case report. J Investig Allergol Clin Immunol. 20:252–4.15. La Rosée P, Horne A, Hines M, von Bahr Greenwood T, Machowicz R, Berliner N, et al. 2019; Recommendations for the management of hemophagocytic lymphohistiocytosis in adults. Blood. 133:2465–77. DOI: 10.1182/blood.2018894618. PMID: 30992265.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tocilizumab-induced Transaminitis in a Seropositive Rheumatoid Arthritis Patient with Macrophage Activation Syndrome
- Refractory Macrophage Activation Syndrome in a Patient with Systemic Lupus Erythematosus Treated with Tocilizumab
- Macrophage Activation Syndrome Presented in a Case of Neonatal Lupus
- Macrophage Activation Syndrome as the Extreme Form of Kawasaki Disease
- A Case of Macrophage Activation Syndrome Developed in Female Adolescent with Systemic Lupus Erythematosus