J Korean Med Sci.
2022 Mar;37(11):e89. 10.3346/jkms.2022.37.e89.
Effect of Maternal Anxiety on Parenting Stress of Fathers of Children With ADHD
- Affiliations
-
- 1Department of Psychiatry, Soonchunhyang University Seoul Hospital, College of Medicine, Seoul, Korea
- 2Department of Nursing, Masan University, Masan, Korea
- KMID: 2527449
- DOI: http://doi.org/10.3346/jkms.2022.37.e89
Abstract
- Background
Hyperactivity, inattention, and impulsivity of children with attention deficit hyperactivity disorder (ADHD) increase parenting stress and familial conflict. Among parentrelated factors, maternal mental health has been studied in-depth, but studies on paternal factors in this context are scarce. This cross-sectional study was conducted of children with ADHD and their parents in South Korea. We investigated the relationships between ADHD symptom severity of children and the mental health of their mothers and fathers.
Methods
The study included 70 children with ADHD and their 140 married heterosexual parents (70 fathers and 70 mothers). Children completed the Child Depression Inventory and State-Anxiety Inventory for children, and their parents completed the Korean ADHD rating scale-IV, Adult ADHD self-report scale, State-Anxiety Inventory, Patient Health Questionnaire-9, and Parental Stress Scale.
Results
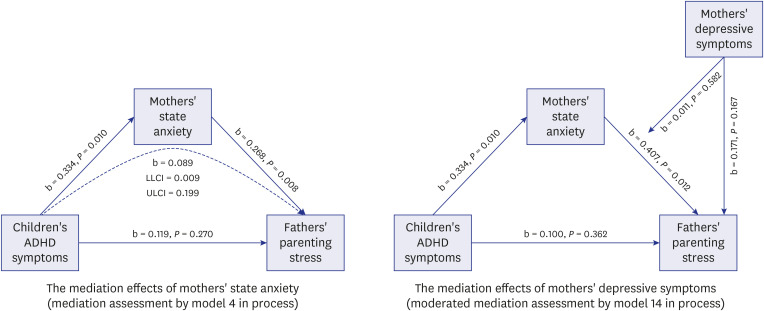
There was a significant positive correlation between children’s ADHD symptoms and maternal anxiety symptom severity, whereby more severe ADHD symptoms were associated with more severe maternal anxiety symptoms. There was also a significant positive correlation between maternal anxiety symptom severity and paternal parenting stress severity, whereby more severe maternal anxiety was associated with more severe paternal parenting stress. A mediation model showed that paternal parenting stress severity was not directly related to children’s ADHD symptoms, but the severity of maternal anxiety mediated this relationship.
Conclusion
The present study found the importance of mental health in mothers of children with ADHD and the interrelatedness of mental health within families. Future assessments and treatment of children with ADHD should include both the children and their parents.
Keyword
Figure
Reference
-
1. Patterson GR. Coercion as a basis for early age of onset for arrest. McCord J, editor. Coercion and Punishment in Long-term Perspectives. Cambridge, UK: Cambridge University Press;1995. p. 81–105.2. Storebø OJ, Ramstad E, Krogh HB, Nilausen TD, Skoog M, Holmskov M, et al. Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD). Cochrane Database Syst Rev. 2015; 2015(11):CD009885.3. Edwards G, Barkley RA, Laneri M, Fletcher K, Metevia L. Parent-adolescent conflict in teenagers with ADHD and ODD. J Abnorm Child Psychol. 2001; 29(6):557–572. PMID: 11761288.4. Fletcher KE, Fischer M, Barkley RA, Smallish L. A sequential analysis of the mother-adolescent interactions of ADHD, ADHD/ODD, and normal teenagers during neutral and conflict discussions. J Abnorm Child Psychol. 1996; 24(3):271–297. PMID: 8836802.5. Graziano PA, McNamara JP, Geffken GR, Reid A. Severity of children’s ADHD symptoms and parenting stress: a multiple mediation model of self-regulation. J Abnorm Child Psychol. 2011; 39(7):1073–1083. PMID: 21629991.6. Theule J, Wiener J, Tannock R, Jenkins JM. Parenting stress in families of children with ADHD: a meta-analysis. J Emot Behav Disord. 2013; 21(1):3–17.7. Wiener J, Biondic D, Grimbos T, Herbert M. Parenting stress of parents of adolescents with attention-deficit hyperactivity disorder. J Abnorm Child Psychol. 2016; 44(3):561–574. PMID: 26183609.8. Baker DB. Parenting stress and ADHD: a comparison of mothers and fathers. J Emot Behav Disord. 1994; 2(1):46–50.9. Mash EJ, Johnston C. A comparison of the mother-child interactions of younger and older hyperactive and normal children. Child Dev. 1982; 53(5):1371–1381. PMID: 7140436.10. Neff PE. Fathering an ADHD child: an examination of paternal well-being and social support. Sociol Inq. 2010; 80(4):531–553. PMID: 20879176.11. Liu L, Wang M. Parenting stress and harsh discipline in China: the moderating roles of marital satisfaction and parent gender. Child Abuse Negl. 2015; 43:73–82. PMID: 25676108.12. Wirth A, Reinelt T, Gawrilow C, Schwenck C, Freitag CM, Rauch WA. Examining the relationship between children’s ADHD symptomatology and inadequate parenting: the role of household chaos. J Atten Disord. 2019; 23(5):451–462. PMID: 29254391.13. Leitch S, Sciberras E, Post B, Gerner B, Rinehart N, Nicholson JM, et al. Experience of stress in parents of children with ADHD: a qualitative study. Int J Qual Stud Health Well-being. 2019; 14(1):1690091. PMID: 31713473.14. McDermut JF, Haaga DA, Bilek LA. Cognitive bias and irrational beliefs in major depression and dysphoria. Cognit Ther Res. 1997; 21(4):459–476.15. Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: implications for research, practice, and DSM-V. J Am Acad Child Adolesc Psychiatry. 1997; 36(8):1065–1079. PMID: 9256586.16. The MTA Cooperative Group. Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: the Multimodal Treatment Study of children with Attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999; 56(12):1088–1096. PMID: 10591284.17. Faraone SV, Biederman J, Friedman D. Validity of DSM-IV subtypes of attention-deficit/hyperactivity disorder: a family study perspective. J Am Acad Child Adolesc Psychiatry. 2000; 39(3):300–307. PMID: 10714049.18. Park JL, Hudec KL, Johnston C. Parental ADHD symptoms and parenting behaviors: a meta-analytic review. Clin Psychol Rev. 2017; 56:25–39. PMID: 28601690.19. Gordon CT, Hinshaw SP. Parenting stress as a mediator between childhood ADHD and early adult female outcomes. J Clin Child Adolesc Psychol. 2017; 46(4):588–599. PMID: 26042524.20. Miranda A, Tárraga R, Fernández MI, Colomer C, Pastor G. Parenting stress in families of children with autism spectrum disorder and ADHD. Except Child. 2015; 82(1):81–95.21. Chi TC, Hinshaw SP. Mother-child relationships of children with ADHD: the role of maternal depressive symptoms and depression-related distortions. J Abnorm Child Psychol. 2002; 30(4):387–400. PMID: 12109489.22. Craig F, Operto FF, De Giacomo A, Margari L, Frolli A, Conson M, et al. Parenting stress among parents of children with neurodevelopmental disorders. Psychiatry Res. 2016; 242:121–129. PMID: 27280521.23. Ma JL, Lai KY. Paternal and maternal experiences in caring for Chinese children with attention deficit hyperactivity disorder in Hong Kong. Asian Soc Work Pol Rev. 2016; 10(2):185–199.24. Mirzaaghas R, Kohani Y, Baniasadi H, Tara F. Maternal Anxiety and Attention Deficit Hyperactivity Disorder (ADHD) in Children. J Midwifery Reprod Health. 2014; 2(4):233–237.25. Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. J Clin Child Psychol. 2001; 30(4):503–513. PMID: 11708238.26. Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD). Child Psychiatry Hum Dev. 2010; 41(2):168–192. PMID: 19768532.27. McCleary L. Parenting adolescents with attention deficit hyperactivity disorder: analysis of the literature for social work practice. Health Soc Work. 2002; 27(4):285–292. PMID: 12494720.28. Schermerhorn AC, D’Onofrio BM, Slutske WS, Emery RE, Turkheimer E, Harden KP, et al. Offspring ADHD as a risk factor for parental marital problems: controls for genetic and environmental confounds. Twin Res Hum Genet. 2012; 15(6):700–713. PMID: 22958575.29. Chung KM, Ebesutani C, Bang HM, Kim J, Chorpita BF, Weisz JR, et al. Parenting stress and child behavior problems among clinic-referred youth: cross-cultural differences across the US and Korea. Child Psychiatry Hum Dev. 2013; 44(3):460–468. PMID: 23073610.30. Rescorla L, Achenbach T, Ivanova MY, Dumenci L, Almqvist F, Niels NB, et al. Behavioral and emotional problems reported by parents of children ages 6 to 16 in 31 societies. J Emot Behav Disord. 2007; 15(3):130–142.31. Kim HO, Hoppe-Graff S. Mothers roles in traditional and modern korean families: The consequences for parental practices and adolescent socialization. Asia Pac Educ Rev. 2001; 2(1):85–93.32. Ra HM, Lee HY. Analysis of research trends on parenting involvement of fathers with early childhood children in Korea. J Fisheries Marine Sci Educ. 2012; 24(2):246–262.33. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, D.C., USA: American Psychiatric Association;2013.34. Pappas D. ADHD Rating Scale-IV: checklists, norms, and clinical interpretation. J Psychoed Assess. 2006; 24(2):172–178.35. Jang SJ, Suh DS, Byun HJ. Normative study of the K-ARS (Korean ADHD Rating Scale) for parents. J Korean Acad Child Adolesc Psychiatry. 2007; 18:38–48.36. Kovacs M. The children’s depression inventory: a self-rated depression scale for school-aged youngsters. [master’s thesis]. Pittsburgh, PA, USA: University of Pittsburgh;1983.37. Costa NM, Weems CF, Pellerin K, Dalton R. Parenting stress and childhood psychopathology: An examination of specificity to internalizing and externalizing symptoms. J Psychopathol Behav Assess. 2006; 28(2):113–122.38. Larson K, Russ SA, Kahn RS, Halfon N. Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics. 2011; 127(3):462–470. PMID: 21300675.39. Cho SC, Lee YS. Development of the Korean form of the Kovacs’ Children’s Depression Inventory. J Korean Neuropsychiatr Assoc. 1990; 29:943–956.40. Kim JH, Lee EH, Joung YS. The WHO Adult ADHD Self-Report Scale: reliability and validity of the Korean version. Psychiatry Investig. 2013; 10(1):41–46.41. Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005; 35(2):245–256. PMID: 15841682.42. Adler LA, Spencer T, Faraone SV, Kessler RC, Howes MJ, Biederman J, et al. Validity of pilot Adult ADHD Self- Report Scale (ASRS) to rate adult ADHD symptoms. Ann Clin Psychiatry. 2006; 18(3):145–148. PMID: 16923651.43. Heo S, Kim JH, Joung YS, Lee WI, Kim JJ, Sohn SH, et al. Clinical utility of the Korean version of the WHO Adult Attention-Deficit/Hyperactivity Disorder Self-Report Scale screener. Psychiatry Investig. 2018; 15(3):325–329.44. Spielberger CD, Gorsuch R, Lushene R. Manual for the State-Trait Inventory. Palo Alto, CA, USA: Consulting Psychologists Press;1970.45. Spielberger CD, Edwards CD, Lushene RE, Montuori J, Platzek D. Preliminary Manual for the State-Trait Anxiety Inventory for Children. Palo Alto, CA, USA: Consulting Psychologists Press;1973.46. Cho SC, Choi JS. Development of the Korean form of the state-trait anxiety inventory for children. Seoul J Psychiatry. 1989; 14:150–157.47. Han DW, Lee CH, Tak JK. Standardization of Spielberger’s manual for the state-trait anxiety inventory. Proc Korean Psychol Assoc. 1993; (1):505–512.48. Spitzer RL, Kroenke K, Williams JB. Primary Care Evaluation of Mental Disorders. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999; 282(18):1737–1744. PMID: 10568646.49. Choi HS, Choi JH, Park KH, Joo KJ, Ga H, Ko HJ, et al. Standardization of the Korean version of Patient Health Questionnaire-9 as a screening instrument for major depressive disorder. J Korean Acad Fam Med. 2007; 28:114–119.50. Berry JO, Jones WH. The Parental Stress Scale: initial psychometric evidence. J Soc Pers Relat. 1995; 12(3):463–472.51. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008; 40(3):879–891. PMID: 18697684.52. Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002; 7(4):422–445. PMID: 12530702.53. Bianchi SM, Casper LM, King RB, editors. Work, Family, Health, and Well-Being. Mahwah, NJ, USA: Routledge;2006.54. Hosley CA, Montemayor R. Fathers and adolescents. In Lamb ME, editor. The Role of the Father in Child Development. 3rd ed. New York, NY, USA: Wiley;1997. p. 163–178.55. Parke RD. Father involvement: a developmental psychological perspective. Marriage Fam Rev. 2000; 29(2-3):43–58.56. Elam KK, Chassin L, Eisenberg N, Spinrad TL. Marital stress and children’s externalizing behavior as predictors of mothers’ and fathers’ parenting. Dev Psychopathol. 2017; 29(4):1305–1318. PMID: 28065187.57. Grych JH, Raynor SR, Fosco GM. Family processes that shape the impact of interparental conflict on adolescents. Dev Psychopathol. 2004; 16(3):649–665. PMID: 15605630.58. Essex MJ, Klein MH, Cho E, Kraemer HC. Exposure to maternal depression and marital conflict: gender differences in children’s later mental health symptoms. J Am Acad Child Adolesc Psychiatry. 2003; 42(6):728–737. PMID: 12921481.59. Costin J, Lichte C, Hill-Smith A, Vance A, Luk E. Parent group treatments for children with oppositional defiant disorder. AeJAMH. 2004; 3(1):36–43.60. DeWolfe NA, Byrne JM, Bawden HN. Early clinical assessment of attention. Clin Neuropsychol. 1999; 13(4):458–473. PMID: 10806460.61. DuPaul GJ, McGoey KE, Eckert TL, VanBrakle J. Preschool children with attention-deficit/hyperactivity disorder: impairments in behavioral, social, and school functioning. J Am Acad Child Adolesc Psychiatry. 2001; 40(5):508–515. PMID: 11349694.62. Cunningham CE, Benness BB, Siegel LS. Family functioning, time allocation, and parental depression in the families of normal and ADDH children. J Clin Child Psychol. 1988; 17(2):169–177.63. Krulik T, Turner-Henson A, Kanematsu Y, al-Ma’aitah R, Swan J, Holaday B. Parenting stress and mothers of young children with chronic illness: a cross-cultural study. J Pediatr Nurs. 1999; 14(2):130–140. PMID: 10337125.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between Parental Attention Deficit Hyperactivity Disorder Characteristics, Executive Function and Parental Emotional Distress
- Parenting Stress and Efficacy of the Mothers of Children with Internet Addiction and Attention-Deficit Hyperactivity Disorder
- The Relationship between Object Relations and Parenting Behavior of Mothers of ADHD Children
- Effects of Maternal Sociodemographic Characteristics and Parenting Stress on a Child's Self-Concept: Parenting Style as a Mediating Factor
- Analysis of Relationships between Parenting Stress, Maternal Depression, and Behavioral Problems in Children at Risk for Attention Deficit Hyperactive Disorder