Anesth Pain Med.
2022 Jan;17(1):112-119. 10.17085/apm.21050.
Management of renin-angiotensin-aldosterone inhibitors and other antihypertensives and their clinical effects on pre-anesthesia blood pressure
- Affiliations
-
- 1Department of Anesthesiology, Ankara City Hospital, Health Sciences University, Ankara, Turkey
- 2Department of Statistics, Hacettepe University, Ankara, Turkey
- KMID: 2526536
- DOI: http://doi.org/10.17085/apm.21050
Abstract
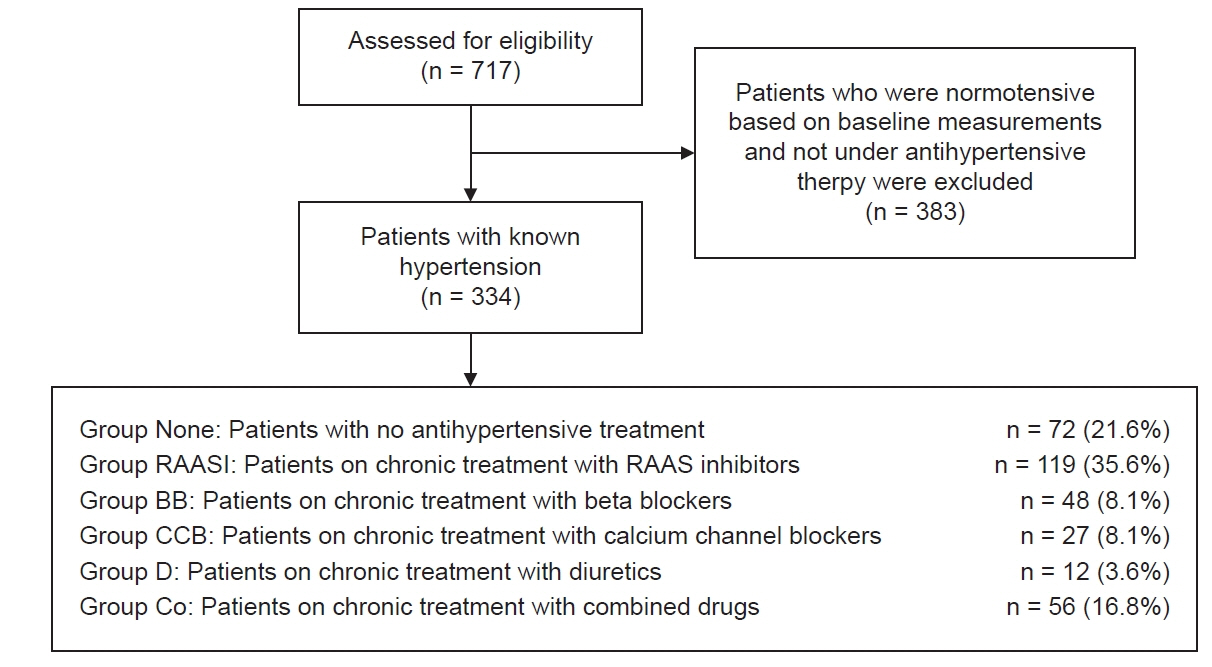
- Background
Blood pressure fluctuations appear more significant in patients with poorly controlled hypertension and are known to be associated with adverse perioperative morbidity. In the present study, we aimed to determine the effects of antihypertensive drug treatment strategies on preanesthetic operating room blood pressure measurements. Methods: A total of 717 patients participated in our study; 383 patients who were normotensive based on baseline measurements and not under antihypertensive therapy were excluded from the analysis. The remaining 334 patients were divided into six groups according to the antihypertensive drug treatment. These six groups were examined in terms of preoperative baseline and pre-anesthesia blood pressure measurements. Results: As a result of the study, it was observed that 24% of patients had high blood pressure precluding surgery, and patients using renin-angiotensin-aldosterone system inhibitors (RAASI) had higher pre-anesthesia systolic blood pressure than patients using other antihypertensive drugs. Patients who received beta-blockers were also observed to have the lowest pre-anesthesia systolic blood pressure, diastolic blood pressure, and mean blood pressure, compared to others. Conclusions: Recently, whether RAASI should be continued preoperatively remains controversial. Our study shows that RAASI cannot provide optimal pre-anesthesia blood pressure and lead to an increase in the number of postponed surgeries, probably due to withdrawal of medication before the operation. Therefore, the preoperative discontinuation of RAASI should be reevaluated in future studies.
Keyword
Figure
Reference
-
1. Crowther M, van der Spuy K, Roodt F, Nejthardt MB, Davids JG, Roos J, et al. The relationship between pre-operative hypertension and intra-operative haemodynamic changes known to be associated with postoperative morbidity. Anaesthesia. 2018; 73:812–8.2. Aronow WS. Management of hypertension in patients undergoing surgery. Ann Transl Med. 2017; 5:227.3. Wong D, Tsai PNW, Ip KY, Irwin MG. New antihypertensive medications and clinical implications. Best Pract Res Clin Anaesthesiol. 2018; 32:223–35.4. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. ESC Scientific Document Group. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–104.5. Dix P, Howell S. Survey of cancellation rate of hypertensive patients undergoing anaesthesia and elective surgery. Br J Anaesth. 2001; 86:789–93.6. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018; 71:e13–115.7. Wolfsthal SD. Is blood pressure control necessary before surgery? Med Clin North Am. 1993; 77:349–63.8. Bouri S, Shun-Shin MJ, Cole GD, Mayet J, Francis DP. Meta-analysis of secure randomised controlled trials of β-blockade to prevent perioperative death in non-cardiac surgery. Heart. 2014; 100:456–64.9. Blessberger H, Kammler J, Domanovits H, Schlager O, Wildner B, Azar D, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev. 2018; 3:CD004476.10. Karachalios GN, Charalabopoulos A, Papalimneou V, Kiortsis D, Dimicco P, Kostoula OK, et al. Withdrawal syndrome following cessation of antihypertensive drug therapy. Int J Clin Pract. 2005; 59:562–70.11. Kristensen SD, Knuuti J, Saraste A, Anker S, Bøtker HE, Hert SD, et al. Authors/Task Force Members. 2014 ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management: the Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014; 35:2383–431.12. Zou Z, Yuan HB, Yang B, Xu F, Chen XY, Liu GJ, et al. Perioperative angiotensin-converting enzyme inhibitors or angiotensin II type 1 receptor blockers for preventing mortality and morbidity in adults. Cochrane Database Syst Rev. 2016; 2016:CD009210.13. Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012; 30:449–56.14. Balci E, Demir A, Bahcecitapar M, Karadeniz U. Diagnosed in operating room with hypertension: a widespread but unseen affliction. Blood Press Monit. 2020; 25:136–41.15. Turan A, You J, Shiba A, Kurz A, Saager L, Sessler DI. Angiotensin converting enzyme inhibitors are not associated with respiratory complications or mortality after noncardiac surgery. Anesth Analg. 2012; 114:552–60.16. Roshanov PS, Rochwerg B, Patel A, Salehian O, Duceppe E, Belley-Côté EP, et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery: an analysis of the vascular events in noncardiac surgery patients cohort evaluation prospective cohort. Anesthesiology. 2017; 126:16–27.17. Kheterpal S, Khodaparast O, Shanks A, O'Reilly M, Tremper KK. Chronic angiotensin-converting enzyme inhibitor or angiotensin receptor blocker therapy combined with diuretic therapy is associated with increased episodes of hypotension in noncardiac surgery. J Cardiothorac Vasc Anesth. 2008; 22:180–6.18. Miceli A, Capoun R, Fino C, Narayan P, Bryan AJ, Angelini GD, et al. Effects of angiotensin-converting enzyme inhibitor therapy on clinical outcome in patients undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2009; 54:1778–84.19. Railton CJ, Wolpin J, Lam-McCulloch J, Belo SE. Renin-angiotensin blockade is associated with increased mortality after vascular surgery. Can J Anaesth. 2010; 57:736–44.20. Rosenman DJ, McDonald FS, Ebbert JO, Erwin PJ, LaBella M, Montori VM. Clinical consequences of withholding versus administering renin-angiotensin-aldosterone system antagonists in the preoperative period. J Hosp Med. 2008; 3:319–25.21. Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014; 130:2215–45.22. Howell SJ. Preoperative hypertension. Curr Anesthesiol Rep. 2018; 8:25–31.23. Kwon S, Thompson R, Florence M, Maier R, McIntyre L, Rogers T, et al. Surgical Care and Outcomes Assessment Program (SCOAP) Collaborative. β-blocker continuation after noncardiac surgery: a report from the surgical care and outcomes assessment program. Arch Surg. 2012; 147:467–73.24. Hartle A, McCormack T, Carlisle J, Anderson S, Pichel A, Beckett N, et al. The measurement of adult blood pressure and management of hypertension before elective surgery: joint guidelines from the Association of Anaesthetists of Great Britain and Ireland and the British Hypertension Society. Anaesthesia. 2016; 71:326–37.25. Charlson ME, MacKenzie CR, Gold JP, Ales KL, Topkins M, Shires GT. Preoperative characteristics predicting intraoperative hypotension and hypertension among hypertensives and diabetics undergoing noncardiac surgery. Ann Surg. 1990; 212:66–81.26. Kihara S, Brimacombe J, Yaguchi Y, Watanabe S, Taguchi N, Komatsuzaki T. Hemodynamic responses among three tracheal intubation devices in normotensive and hypertensive patients. Anesth Analg. 2003; 96:890–5.27. Venkatesan S, Myles PR, Manning HJ, Mozid AM, Andersson C, Jørgensen ME, et al. Cohort study of preoperative blood pressure and risk of 30-day mortality after elective non-cardiac surgery. Br J Anaesth. 2017; 119:65–77.28. Vázquez-Narváez KG, Ulibarri-Vidales M. The patient with hypertension and new guidelines for therapy. Curr Opin Anaesthesiol. 2019; 32:421–6.29. Bilo G, Grillo A, Guida V, Parati G. Morning blood pressure surge: pathophysiology, clinical relevance and therapeutic aspects. Integr Blood Press Control. 2018; 11:47–56.30. Bowles NP, Thosar SS, Herzig MX, Shea SA. Chronotherapy for hypertension. Curr Hypertens Rep. 2018; 20:97. Erratum in: Curr Hypertens Rep 2018;21:1.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New drugs for treatment of hypertension
- Use of Angiotensin Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: A Closer Look at Hyperkalemia
- Overview of the Renin-Angiotensin System
- Intra-operative refractory hypotension in patient chronically treated with renin-angiotensin system antagonists: A case report
- The Relationship between Aldosterone to Renin Ratio and RI Value of the Uterine Artery in the Preeclamptic Patient vs. Normal Pregnancy