Anesth Pain Med.
2022 Jan;17(1):52-56. 10.17085/apm.21071.
The use of sugammadex in an infant with prolonged neuromuscular blockade - A case report -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- KMID: 2526527
- DOI: http://doi.org/10.17085/apm.21071
Abstract
- Background
Residual neuromuscular blockade (RNMB) is a frequent event after general anesthesia, which can lead to serious complications, such as upper airway obstruction. Sugammadex is useful in reversing RNMB. However, its use in infants has not yet been approved by the Food and Drug Administration. Therefore, anesthesiologists can be hesitant use it, even in situations where no other choice is available. Case: A two-month-old baby presented to the hospital for umbilical polypectomy. At the end of the surgery, neostigmine was administered. Even after waiting for 30 min and injecting an additional dose of neostigmine, neuromuscular blockade was not adequately reversed. Eventually, sugammadex was administered, and spontaneous breathing returned.
Conclusions
If there were no particular causes of delayed return to spontaneous breathing in infants, RNMB should be considered and reversal with sugammadex would be useful.
Keyword
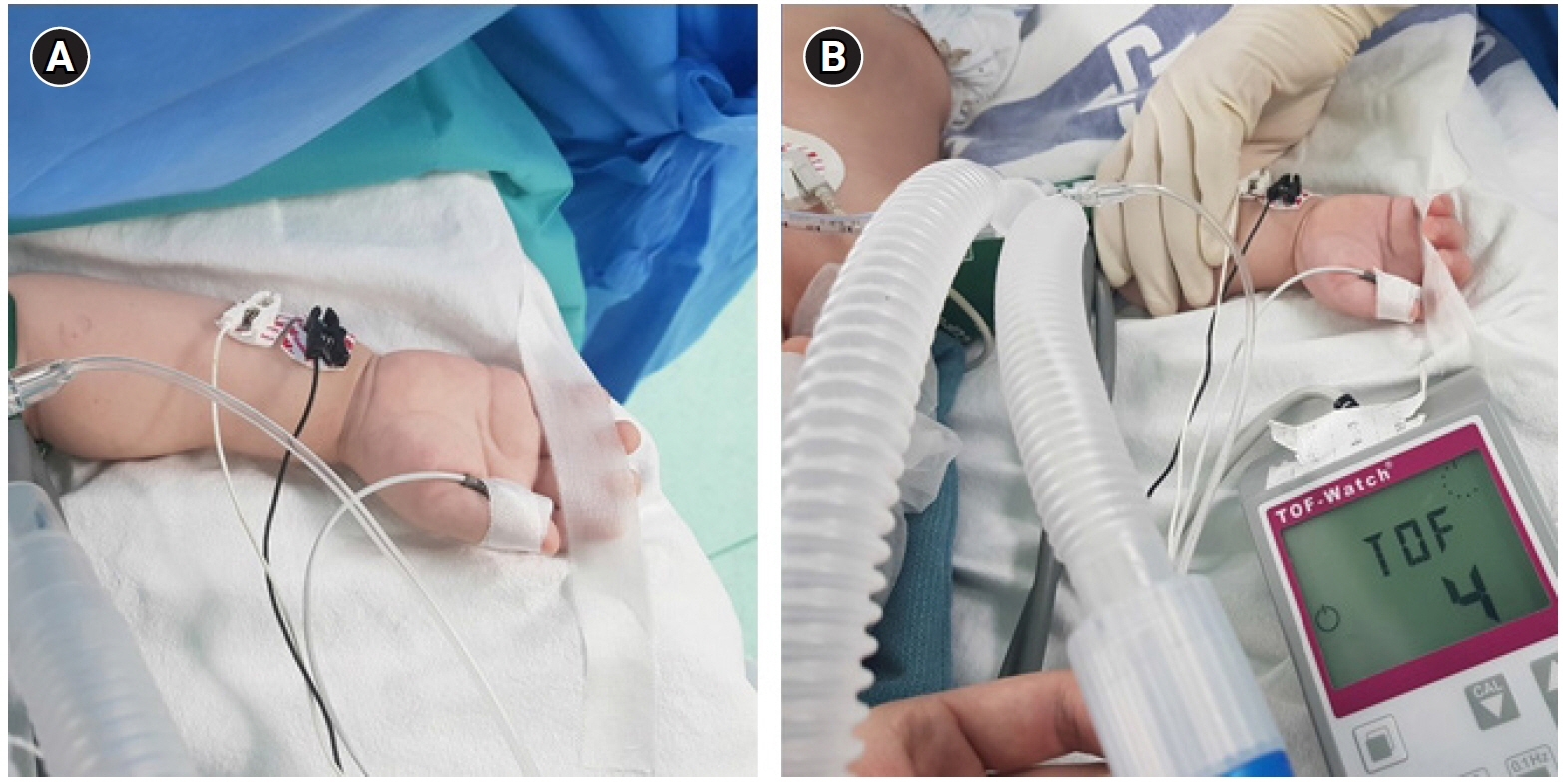
Figure
Reference
-
1. Meretoja OA. Neuromuscular block and current treatment strategies for its reversal in children. Paediatr Anaesth. 2010; 20:591–604.2. Viby-Mogensen J, Jørgensen BC, Ording H. Residual curarization in the recovery room. Anesthesiology. 1979; 50:539–41.3. Viby-Mogensen J. Postoperative residual curarization and evidence-based anaesthesia. Br J Anaesth. 2000; 84:301–3.4. Gropper MA, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Cohen NH, Leslie K. Miller's anesthesia. 9th ed. Philadelphia, Elsevier;2020. p. 832–64.5. Jones RK, Caldwell JE, Brull SJ, Soto RG. Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology. 2008; 109:816–24.6. Tobias JD. Current evidence for the use of sugammadex in children. Paediatr Anaesth. 2017; 27:781.7. Won YJ, Lim BG, Lee DK, Kim H, Kong MH, Lee IO. Sugammadex for reversal of rocuronium-induced neuromuscular blockade in pediatric patients: a systematic review and meta-analysis. Medicine (Baltimore). 2016; 95:e4678.8. Ozmete O, Bali C, Cok OY, Turk HE, Ozyilkan NB, Civi S, et al. Sugammadex given for rocuronium-induced neuromuscular blockade in infants: a retrospectıve study. J Clin Anesth. 2016; 35:497–501.9. Kim JE, Chun HR. Rocuronium-induced neuromuscular block and sugammadex in pediatric patient with duchenne muscular dystrophy: a case report. Medicine (Baltimore). 2017; 96:e6456.10. Sung TY, Kang T, Cho C, Kwon HU, Kang PS, Jee YS. Experience with reversal of a neuromuscular block with sugammadex in a child with Prader-Willi syndrome - a case report -. Anesth Pain Med. 2017; 12:335–8.11. Franz AM, Chiem J, Martin LD, Rampersad S, Phillips J, Grigg EB. Case series of 331 cases of sugammadex compared to neostigmine in patients under 2 years of age. Paediatr Anaesth. 2019; 29:591–6.12. Cascella M, Bimonte S, Di Napoli R. Delayed emergence from anesthesia: what we know and how we act. Local Reg Anesth. 2020; 13:195–206.13. Anderson BJ. Pharmacology in the very young: anaesthetic implications. Eur J Anaesthesiol. 2012; 29:261–70.