J Dent Rehabil Appl Sci.
2021 Jun;37(2):88-94. 10.14368/jdras.2021.37.2.88.
Anti-inflammatory effect of non-thermal atmospheric pressure plasma for periodontitis treatment: in vitro pilot study
- Affiliations
-
- 1Department of Periodontology, School of Dentistry and Dental Research Institute, Pusan National University, Yangsan, Republic of Korea
- 2Department of Oral Medicine, School of Dentistry and Dental Research Institute, Pusan National University, Yangsan, Republic of Korea
- 3Dental Clinic Center, Pusan National University Hospital, Busan, Republic of Korea
- KMID: 2525982
- DOI: http://doi.org/10.14368/jdras.2021.37.2.88
Abstract
- Purpose
The purpose of this study was to evaluate the anti-inflammatory effects of non-thermal atmospheric pressure plasma (NTP) on human gingival fibroblasts (HGFs) for clinical application of periodontal treatment.
Materials and Methods
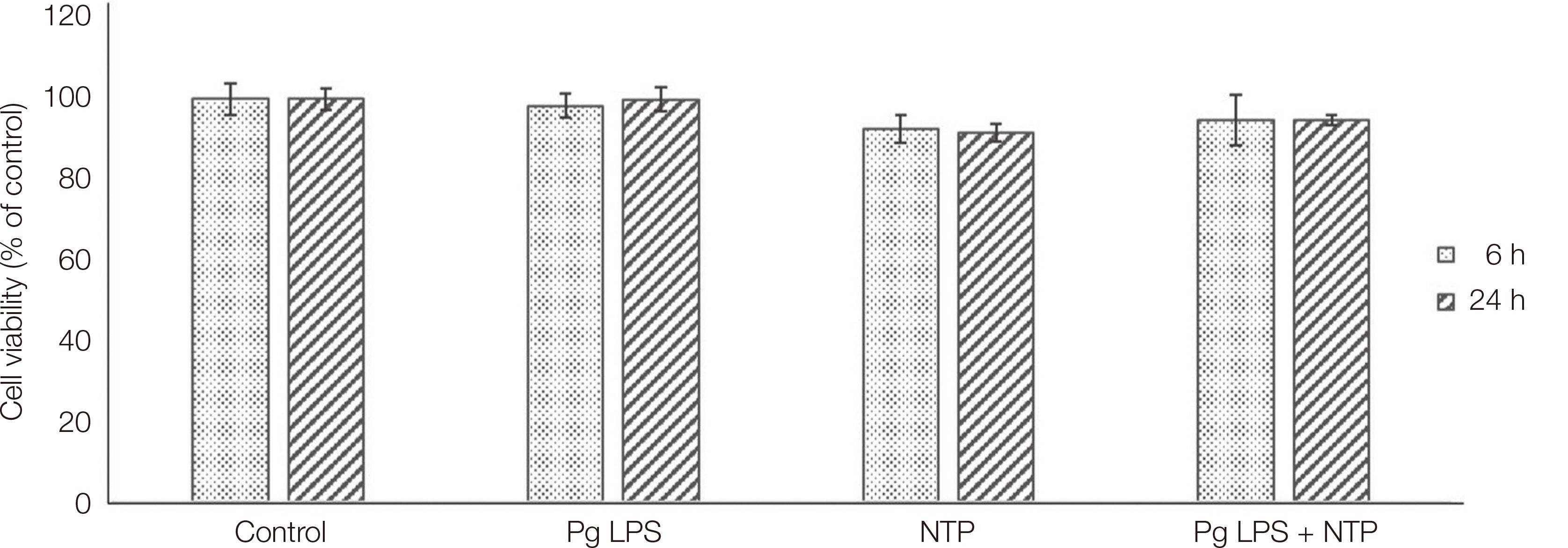
HGFs were treated with Porphyromonas gingivalis (Pg) lipopolysaccharide (LPS). Customized NTP device was developed for periodontal in vitro study. Cell viability was evaluated with cell counting kit-8. The levels of inflammatory cytokines, including interleukin (IL)-8 and 6, were determined by enzyme-linked immunosorbent assay.
Results
When NTP was applied, the cell viability did not change significantly, and there was no difference for 6 h and 24h. When Pg LPS was treated to HGFs, the secretion of IL-8 and IL-6 was increased compared to the control group. But when the NTP was applied, the secretion of them was significantly decreased.
Conclusion
NTP did not affect cell viability of HGFs. And it inhibited the LPS-induced production of IL-8 and IL-6.
Keyword
Figure
Reference
-
References
1. Park SR, Hong JW, Lee HJ, Kim GC. 2013; Plasma Medicine; How can Nonthermal Atmospheric Plasma be Applied to Medicine? J Life Sc. 23:838–46. DOI: 10.5352/JLS.2013.23.6.838.2. Kim CH. 2010; New conversing technology; plasma medicine. Korean J Otorhinolaryngol-Head Neck Surg. 53:593–602. DOI: 10.3342/kjorl-hns.2010.53.10.593.3. VON Woedtke T, Schmidt A, Bekeschus S, Wende K, Weltmann KD. 2019; Plasma Medicine: A Field of Applied Redox Biology. In Vivo. 33:1011–26. DOI: 10.21873/invivo.11570. PMID: 31280189. PMCID: PMC6689367.4. Kim YM, Lee HY, Lee HJ, Kim JB, Kim S, Joo JY, Kim GC. 2018; Retention Improvement in Fluoride Application with Cold Atmospheric Plasma. J Dent Res. 97:179–83. DOI: 10.1177/0022034517733958. PMID: 28945493. PMCID: PMC6429569.5. Nam SH, Lee HJ, Hong JW, Kim GC. 2015; Efficacy of nonthermal atmospheric pressure plasma for tooth bleaching. ScientificWorldJournal. 2015:581731. DOI: 10.1155/2015/581731. PMID: 25685843. PMCID: PMC4320848.6. Armand A, Khani M, Asnaashari M, AliAhmadi A, Shokri B. 2019; Comparison study of root canal disinfection by cold plasma jet and photodynamic therapy. Photodiagnosis Photodyn Ther. 26:327–33. DOI: 10.1016/j.pdpdt.2019.04.023. PMID: 31026615.7. Pan J, Sun K, Liang Y, Sun P, Yang X, Wang J, Zhang J, Zhu W, Fang J, Becker KH. 2013; Cold plasma therapy of a tooth root canal infected with enterococcus faecalis biofilms in vitro. J Endod. 39:105–10. DOI: 10.1016/j.joen.2012.08.017. PMID: 23228267.8. Lee CM, Jeong YI, Kook MS, Kim BH. 2020; Combinatorial Effect of Cold Atmosphere Plasma (CAP) and the Anticancer Drug Cisplatin on Oral Squamous Cell Cancer Therapy. Int J Mol Sci. 21:7646. DOI: 10.3390/ijms21207646. PMID: 33076565. PMCID: PMC7588898.9. Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D. 2002; A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol. 29 Suppl 3:92–102. DOI: 10.1034/j.1600-051X.29.s3.5.x. PMID: 12787211.10. Bartold PM, Van Dyke TE. 2017; Host modulation: controlling the inflammation to control the infection. Periodontol 2000. 75:317–29. DOI: 10.1111/prd.12169. PMID: 28758299.11. Schueller K, Hans J, Pfeiffer S, Walker J, Ley JP, Somoza V. 2020; Identification of Interleukin-8-Reducing Lead Compounds Based on SAR Studies on Dihydrochalcone-Related Compounds in Human Gingival Fibroblasts (HGF-1 cells) In Vitro. Molecules. 25:1382. DOI: 10.3390/molecules25061382. PMID: 32197426. PMCID: PMC7144391.12. Eaton KA, Kaiser JB, Davies RM. 1985; The removal of root surface deposits. J Clin Periodontol. 12:141–52. DOI: 10.1111/j.1600-051X.1985.tb01373.x. PMID: 3882769.13. Cobb CM. 2017; Lasers and the treatment of periodontitis: the essence and the noise. Periodontol 2000. 75:205–95. DOI: 10.1111/prd.12137. PMID: 28758295.14. Park EJ, Kwon EY, Kim HJ, Lee JY, Choi J, Joo JY. 2018; Clinical and microbiological effects of the supplementary use of an erythritol powder air-polishing device in non-surgical periodontal therapy: a randomized clinical trial. J Periodontal Implant Sci. 48:295–304. DOI: 10.5051/jpis.2018.48.5.295. PMID: 30405937. PMCID: PMC6207796.15. Mahasneh A, Darby M, Tolle SL, Hynes W, Laroussi M, Karakas E. 2011; Inactivation of Porphyromonas gingivalis by low-temperature atmospheric pressure plasma. Plasma Med. 1:191–204. DOI: 10.1615/PlasmaMed.2012002854.16. Shimada Y, Komatsu Y, Ikezawa-Suzuki I, Tai H, Sugita N, Yoshie H. 2010; The effect of periodontal treatment on serum leptin, interleukin-6, and Creactive protein. J Periodontol. 81:1118–23. DOI: 10.1902/jop.2010.090741. PMID: 20370420.17. Lagdive SS, Marawar PP, Byakod G, Lagdive SB. 2013; Evaluation and comparison of interleukin-8 (IL-8) level in gingival crevicular fluid in health and severity of periodontal disease: a clinico-biochemical study. Indian J Dent Res. 24:188–92. DOI: 10.4103/0970-9290.116675. PMID: 23965444.18. Begley CG, Ellis LM. 2012; Drug development: Raise standards for preclinical cancer research. Nature. 28:531–3. DOI: 10.1038/483531a. PMID: 22460880.19. Wei M, Zhang R, Zhang F, Zhang Y, Li G, Miao R, Shao S. 2019; An Evaluation Approach of Cell Viability Based on Cell Detachment Assay in a Single-Channel Integrated Microfluidic Chip. ACS Sens. 4:2654–61. DOI: 10.1021/acssensors.9b01061. PMID: 31502455.20. Hegde R, Awan KH. 2019; Effects of periodontal disease on systemic health. Dis Mon. 65:185–92. DOI: 10.1016/j.disamonth.2018.09.011. PMID: 30384973.21. Takashiba S, Naruishi K, Murayama Y. 2003; Perspective of cytokine regulation for periodontal treatment: Fibroblast biology. J Periodontol. 74:103–10. DOI: 10.1902/jop.2003.74.1.103. PMID: 12593604.22. Finoti LS, Nepomuceno R, Pigossi SC, Corbi SC, Secolin R, Scarel-Caminaga RM. 2017; Association between interleukin-8 levels and chronic periodontal disease: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 96:e6932. DOI: 10.1097/MD.0000000000006932. PMID: 28562542. PMCID: PMC5459707.23. Naruishi K, Nagata T. 2018; Biological effects of interleukin-6 on Gingival Fibroblasts: Cytokine regulation in periodontitis. J Cell Physiol. 233:6393–400. DOI: 10.1002/jcp.26521. PMID: 29574949.24. Shindo S, Hosokawa Y, Hosokawa I, Shiba H. 2019; Interleukin (IL)-35 Suppresses IL-6 and IL-8 Production in IL-17A-Stimulated Human Periodontal Ligament Cells. Inflammation. 42:835–40. DOI: 10.1007/s10753-018-0938-9. PMID: 30484005.25. Xiong G, Ji W, Wang F, Zhang F, Xue R, Cheng M, Sun Y, Wang X, Zhang T. 2019; Quercetin Inhibits Inflammatory Response Induced by LPS from Porphyromonas gingivalis in Human Gingival Fibroblasts via Suppressing NF-κB Signaling Pathway. Biomed Res Int. 2019:6282635. DOI: 10.1155/2019/6282635. PMID: 31531360. PMCID: PMC6720363.26. Muniz FW, Nogueira SB, Mendes FL, Rösing CK, Moreira MM, de Andrade GM, de Sousa Carvalho R. 2015; The impact of antioxidant agents complimentary to periodontal therapy on oxidative stress and periodontal outcomes: A systematic review. Arch Oral Biol. 60:1203–14. DOI: 10.1016/j.archoralbio.2015.05.007. PMID: 26067357.27. Kleineidam B, Nokhbehsaim M, Deschner J, Wahl G. 2019; Effect of cold plasma on periodontal wound healingan in vitro study. Clin Oral Investig. 23:1941–50. DOI: 10.1007/s00784-018-2643-3. PMID: 30232626.28. Zhang Y, Xiong Y, Xie P, Ao X, Zheng Z, Dong X, Li H, Yu Q, Zhu Z, Chen M, Chen W. 2018; Non-thermal plasma reduces periodontitis-induced alveolar bone loss in rats. Biochem Biophys Res Commun. 503:2040–6. DOI: 10.1016/j.bbrc.2018.07.154. PMID: 30086885.29. Soares DJ, Walker J, Pignitter M, Walker JM, Imboeck JM, Ehrnhoefer-Ressler MM, Brasil IM, Somoza V. 2014; Pitanga (Eugenia uniflora L.) fruit juice and two major constituents thereof exhibit antiinflammatory properties in human gingival and oral gum epithelial cells. Food Funct. 5:2981–8. DOI: 10.1039/C4FO00509K. PMID: 25228206.30. Hajishengallis G, Chavakis T, Lambris JD. 2020; Current understanding of periodontal disease pathogenesis and targets for host-modulation therapy. Periodontol 2000. 84:14–34. DOI: 10.1111/prd.12331. PMID: 32844416. PMCID: PMC7457922.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-Thermal Atmospheric-Pressure Plasma Possible Application in Wound Healing
- New Conversing Technology; Plasma Medicine
- Evaluation of the safety of non-thermal atmospheric-pressure plasma in hairless mouse tissues
- Sterilization effect of atmospheric pressure non-thermal air plasma on dental instruments
- Non-thermal Atmospheric Plasma for the Treatment of Onychomycosis: in vitro and ex vivo Ultrastructural Study