Cancer Res Treat.
2022 Jan;54(1):118-129. 10.4143/crt.2021.101.
Long-term Survivals, Toxicities and the Role of Chemotherapy in Early-Stage Nasopharyngeal Carcinoma Patients Treated with Intensity-Modulated Radiation Therapy: A Retrospective Study with 15-Year Follow-up
- Affiliations
-
- 1Department of Nasopharyngeal Carcinoma, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangdong Key Laboratory of Nasopharyngeal Carcinoma Diagnosis and Therapy, Guangzhou, China
- 2Department of Radiotherapy, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangdong Key Laboratory of Nasopharyngeal Carcinoma Diagnosis and Therapy, Guangzhou, China
- KMID: 2524593
- DOI: http://doi.org/10.4143/crt.2021.101
Abstract
- Purpose
This study was aimed to investigate long-term survivals and toxicities of early-stage nasopharyngeal carcinoma (NPC) in endemic area, evaluating the role of chemotherapy in stage II patients.
Materials and Methods
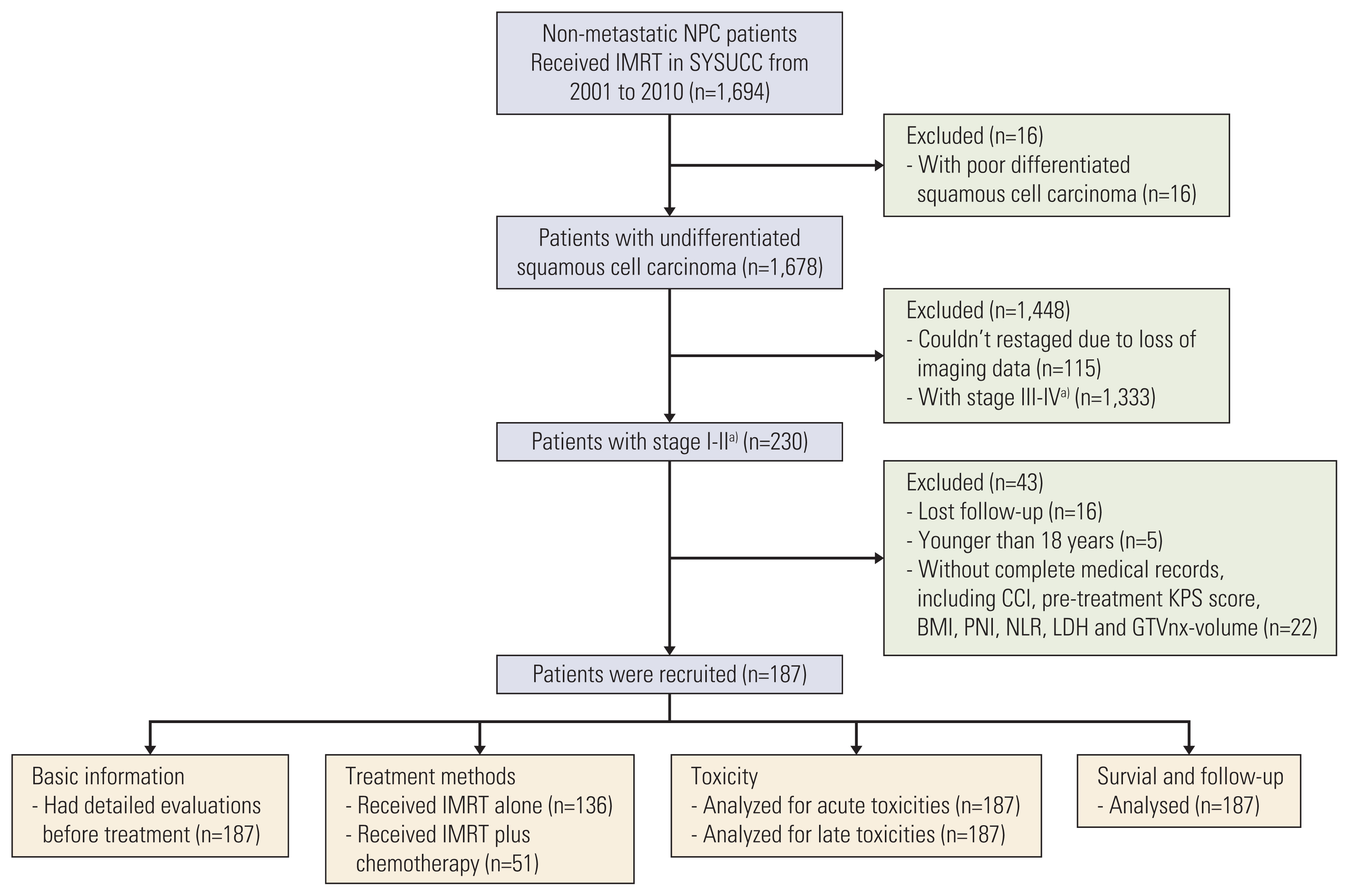
Totally 187 patients with newly diagnosed NPC and restaged American Joint Committee on Cancer/ International Union Against Cancer 8th T1-2N0-1M0 were retrospectively recruited. All received intensity-modulated radiotherapy (IMRT)±chemotherapy (CT) from 2001 to 2010.
Results
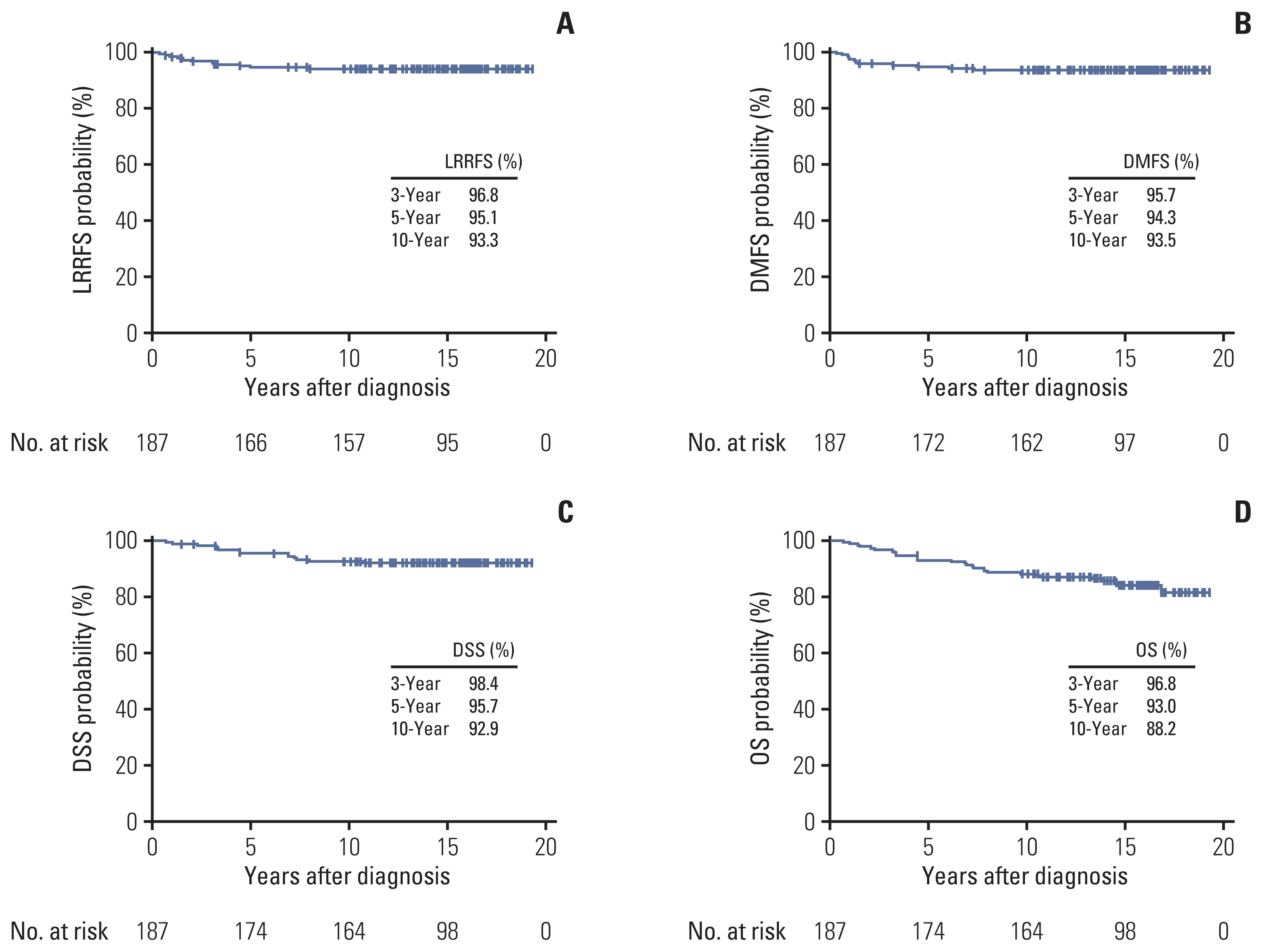
With 15.7-year median follow-up, 10-year locoregional recurrence-free survival, distant metastasis-free survival (DMFS), disease-specific survival (DSS), and overall survival (OS) were 93.3%, 93.5%, 92.9% and 88.2%, respectively. Multivariable analyses showed cervical lymph nodes positive and pre-treatment prognostic nutritional index ≥ 52.0 could independently predict DMFS (p=0.036 and p=0.011), DSS (p=0.014 and p=0.026), and OS (p=0.002 and p < 0.001); Charlson comorbidity index < 3 points could predict DSS (p=0.011); age > 45 years (p=0.002) and pre-treatment lactate dehydrogenase ≥ 240 U/L (p < 0.001) predicted OS. No grade 4 late toxicity happened; grade 3 late toxicities included subcutaneous fibrosis (4.3%), deafness or otitis (4.8%), skin dystrophy (2.1%), and xerostomia (1.1%). No differences on survivals were shown between IMRT+CT vs. IMRT alone in stage II patients, even in T2N1M0 (p > 0.05). Unsurprising, patients in IMRT+CT had more acute gastrointestinal reaction, myelosuppression, mucositis, late ear toxicity, and cranial nerve injury (all p < 0.05) than IMRT alone group.
Conclusion
Superior tumor control and satisfying long-term outcomes could be achieved with IMRT in early-stage NPC with mild late toxicities. As CT would bring more toxicities, it should be carefully performed to stage II patients.
Keyword
Figure
Reference
-
References
1. Wei KR, Zheng RS, Zhang SW, Liang ZH, Li ZM, Chen WQ. Nasopharyngeal carcinoma incidence and mortality in China, 2013. Chin J Cancer. 2017; 36:90.
Article2. O’Sullivan B, Rumble RB, Warde P. Members of the IMRT Indications Expert Panel. Intensity-modulated radiotherapy in the treatment of head and neck cancer. Clin Oncol (R Coll Radiol). 2012; 24:474–87.3. Peng G, Wang T, Yang KY, Zhang S, Zhang T, Li Q, et al. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol. 2012; 104:286–93.
Article4. Chua DT, Ma J, Sham JS, Mai HQ, Choy DT, Hong MH, et al. Improvement of survival after addition of induction chemotherapy to radiotherapy in patients with early-stage nasopharyngeal carcinoma: Subgroup analysis of two Phase III trials. Int J Radiat Oncol Biol Phys. 2006; 65:1300–6.
Article5. Xiao WW, Han F, Lu TX, Chen CY, Huang Y, Zhao C. Treatment outcomes after radiotherapy alone for patients with early-stage nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2009; 74:1070–6.
Article6. Song CH, Wu HG, Heo DS, Kim KH, Sung MW, Park CI. Treatment outcomes for radiotherapy alone are comparable with neoadjuvant chemotherapy followed by radiotherapy in early-stage nasopharyngeal carcinoma. Laryngoscope. 2008; 118:663–70.
Article7. Su SF, Han F, Zhao C, Chen CY, Xiao WW, Li JX, et al. Long-term outcomes of early-stage nasopharyngeal carcinoma patients treated with intensity-modulated radiotherapy alone. Int J Radiat Oncol Biol Phys. 2012; 82:327–33.
Article8. Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. New York: Springer;2017.9. Luo S, Zhao L, Wang J, Xu M, Li J, Zhou B, et al. Clinical outcomes for early-stage nasopharyngeal carcinoma with predominantly WHO II histology treated by intensity-modulated radiation therapy with or without chemotherapy in nonendemic region of China. Head Neck. 2014; 36:841–7.
Article10. Ding XC, Fan PP, Xie P, Fan BJ, Yang J, Jiang LY, et al. Ten-year outcomes of intensity-modulated radiotherapy (IMRT) combine with chemotherapy versus IMRT alone for stage II nasopharyngeal carcinoma in the real-world study (RWD). Cancer Manag Res. 2019; 11:8893–903.11. Huang X, Chen X, Zhao C, Wang J, Wang K, Wang L, et al. Adding concurrent chemotherapy to intensity-modulated radiotherapy does not improve treatment outcomes for stage II nasopharyngeal carcinoma: a phase 2 multicenter clinical trial. Front Oncol. 2020; 10:1314.
Article12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.
Article13. Huang Y, Chen W, Haque W, Verma V, Xing Y, Teh BS, et al. The impact of comorbidity on overall survival in elderly nasopharyngeal carcinoma patients: a National Cancer Data Base analysis. Cancer Med. 2018; 7:1093–101.
Article14. Miao J, Wang L, Zhu M, Xiao W, Wu H, Di M, et al. Reprint of long-term survival and late toxicities of elderly nasopharyngeal carcinoma (NPC) patients treated by high-total-and fractionated-dose simultaneous modulated accelerated radiotherapy with or without chemotherapy. Oral Oncol. 2019; 90:126–33.15. Ikeya T, Shibutani M, Maeda K, Sugano K, Nagahara H, Ohtani H, et al. Maintenance of the nutritional prognostic index predicts survival in patients with unresectable metastatic colorectal cancer. J Cancer Res Clin Oncol. 2015; 141:307–13.
Article16. Miao J, Xiao W, Wang L, Han F, Wu H, Deng X, et al. The value of the prognostic nutritional index (PNI) in predicting outcomes and guiding the treatment strategy of nasopharyngeal carcinoma (NPC) patients receiving intensity-modulated radiotherapy (IMRT) with or without chemotherapy. J Cancer Res Clin Oncol. 2017; 143:1263–73.
Article17. Hong S, Zhou T, Fang W, Xue C, Hu Z, Qin T, et al. The prognostic nutritional index (PNI) predicts overall survival of small-cell lung cancer patients. Tumour Biol. 2015; 36:3389–97.
Article18. Hofbauer SL, Pantuck AJ, de Martino M, Lucca I, Haitel A, Shariat SF, et al. The preoperative prognostic nutritional index is an independent predictor of survival in patients with renal cell carcinoma. Urol Oncol. 2015; 33:68.
Article19. Jiang N, Deng JY, Ding XW, Ke B, Liu N, Zhang RP, et al. Prognostic nutritional index predicts postoperative complications and long-term outcomes of gastric cancer. World J Gastroenterol. 2014; 20:10537–44.
Article20. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995; 31:1341–6.
Article21. Miao J, Di M, Chen B, Wang L, Cao Y, Xiao W, et al. A prospective 10-year observational study of reduction of radiation therapy clinical target volume and dose in early-stage nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2020; 107:672–82.
Article22. Chen QY, Wen YF, Guo L, Liu H, Huang PY, Mo HY, et al. Concurrent chemoradiotherapy vs radiotherapy alone in stage II nasopharyngeal carcinoma: phase III randomized trial. J Natl Cancer Inst. 2011; 103:1761–70.
Article23. Aftab O, Liao S, Zhang R, Tang N, Luo M, Zhang B, et al. Efficacy and safety of intensity-modulated radiotherapy alone versus intensity-modulated radiotherapy plus chemotherapy for treatment of intermediate-risk nasopharyngeal carcinoma. Radiat Oncol. 2020; 15:66.
Article24. Xu T, Shen C, Zhu G, Hu C. Omission of chemotherapy in early stage nasopharyngeal carcinoma treated with IMRT: a paired cohort study. Medicine (Baltimore). 2015; 94:e1457.25. Xu C, Sun R, Tang LL, Chen L, Li WF, Mao YP, et al. Role of sequential chemoradiotherapy in stage II and low-risk stage III–IV nasopharyngeal carcinoma in the era of intensity-modulated radiotherapy: a propensity score-matched analysis. Oral Oncol. 2018; 78:37–45.
Article26. Xu C, Zhang LH, Chen YP, Liu X, Zhou GQ, Lin AH, et al. Chemoradiotherapy versus radiotherapy alone in stage II nasopharyngeal carcinoma: a systemic review and meta-analysis of 2138 patients. J Cancer. 2017; 8:287–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term results of forward intensity-modulated radiation therapy for patients with early-stage breast cancer
- Neoadjuvant Chemotherapy and Radiation Therapy inAdvanced Stage Nasopharyngeal Carcinoma
- Long-Term Results of 2-Dimensional Radiation Therapy in Patients with Nasopharyngeal Cancer
- Locoregionally advanced nasopharyngeal carcinoma treated with intensity-modulated radiotherapy plus concurrent weekly cisplatin with or without neoadjuvant chemotherapy
- Results of Radiation Therapy in Nasopharyngeal Cancer