Child Kidney Dis.
2021 Dec;25(2):122-127. 10.3339/jkspn.2021.25.2.122.
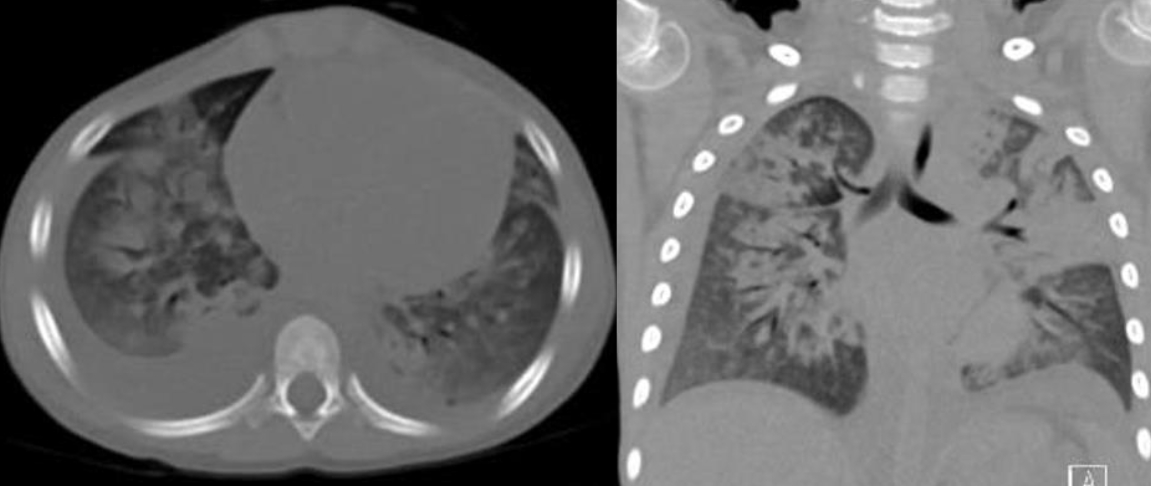
Acute Respiratory Distress Syndrome after Rotavirus Infection in a C1q Nephropathy Patient: A Case Report
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Korea
- 2Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Pediatrics,Anyang University Seoul Hospital, Seoul, Korea
- 4Department of Pediatrics, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 5Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2524514
- DOI: http://doi.org/10.3339/jkspn.2021.25.2.122
Abstract
- C1q nephropathy is a rare glomerulopathy that typically presents with nephrotic syndrome in children. Treatment with immunosuppressive agents renders patients vulnerable to infection and its complications. Gastroenteritis is common in children, and rotavirus is a leading cause. Extraintestinal manifestations of rotavirus have recently been reported; however, there is a paucity of cases exploring the involvement of a rotavirus on the respiratory system. Acute respiratory distress syndrome (ARDS) is a rapid onset respiratory failure characterized by noncardiogenic pulmonary edema and hypoxemia. Causes of ARDS include sepsis, pneumonia, pancreatitis, aspiration, and trauma. In this paper, we report a case of ARDS after rotavirus infection in a child with C1q nephropathy who had been treated with immunosuppressive agents.
Keyword
Figure
Reference
-
References
1. Jennette JC, Hipp CG. C1q nephropathy: a distinct pathologic entity usually causing nephrotic syndrome. Am J Kidney Dis. 1985; 6:103–10.2. Bishop RF, Davidson GP, Holmes IH, Ruck BJ. Virus particles in epithelial cells of duodenal mucosa from children with acute non-bacterial gastroenteritis. Lancet. 1973; 2:1281–3.
Article3. Lynch M, Shieh WJ, Tatti K, Gentsch JR, Harris TF, Jiang B, et al. The Pathology of Rotavirus-Associated Deaths, Using New Molecular Diagnostics. Clinical Infectious Diseases. 2003; 37:1327–3.
Article4. Group PALICC. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatric Critical Care Medicine. 2015; 16:428–39.5. Tai IC, Huang YC, Lien RI, Huang CG, Tsao KC, Lin TY. Clinical manifestations of a cluster of rotavirus infection in young infants hospitalized in neonatal care units. Journal of Microbiology, Immunology and Infection. 2012; 45:15–21.
Article6. Sasek L, Pazdiora P, Kobr J, Pizingerová K. Lethal course of rotavirus gastroenteritis-a case history. Klinicka Mikrobiologie a Infekcni Lekarstvi. 2005; 11:67–9.7. Blutt SE, Matson DO, Crawford SE, Staat MA, Azimi P, Bennett BL, et al. Rotavirus Antigenemia in Children Is Associated with Viremia. PLOS Medicine. 2007; 4:e121.
Article8. Gilger MA, Matson DO, Conner ME, Rosenblatt HM, Finegold MJ, Estes MK. Extraintestinal rotavirus infections in children with immunodeficiency. J Pediatr. 1992; 120:912–7.
Article9. Zhaori G, Fu L, Xu Y, Guo Y, Peng Z, Shan W. Detection of rotavirus antigen in tracheal aspirates of infants and children with pneumonia. Chinese Medical Journal. 1991; 104:830–3.10. Santosham M, Yolken RH, Quiroz E, Dillman L, Oro G, Reeves WC, et al. Detection of rotavirus in respiratory secretions of children with pneumonia. The Journal of Pediatrics. 1983; 103:583–5.
Article11. Lewis HM, Parry JV, Davies HA, Parry RP, Mott A, Dourmashkin RR, et al. A year's experience of the rotavirus syndrome and its association with respiratory illness. Arch Dis Child. 1979; 54:339–46.
Article12. Goldwater PN, Chrystie IL, Banatvala J. Rotaviruses and the respiratory tract. British Medical Journal. 1979; 2:1551.
Article13. Saulsbury FT, Winkelstein JA, Yolken RH. Chronic rotavirus infection in immunodeficiency. The Journal of Pediatrics. 1980; 97:61–5.
Article14. Blutt SE, Kirkwood CD, Parreño V, Warfield KL, Ciarlet M, Estes MK, et al. Rotavirus antigenaemia and viraemia: a common event? The lancet. 2003; 362:1445–9.
Article15. Dhokarh R, Li G, Schmickl CN, Kashyap R, Assudani J, Limper AH, et al. Drug-associated acute lung injury: a population-based cohort study. Chest. 2012; 142:845–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complete Remission from C1q Nephropathy with Disappearance of C1q Deposition after Steroid Therapy
- A Case of C1q Nephropathy in Steroid-Dependent Nephrotic Syndrome
- Two Cases of C1q Nephropathy in Siblings
- Proteinuria in a Boy with Infectious Mononucleosis, C1q Nephropathy, and Dent's Disease
- A Case of C1q Mediated Glomerulonephritis Manifested by Asymptomatic Hematuria