Child Kidney Dis.
2021 Dec;25(2):117-121. 10.3339/jkspn.2021.25.2.117.
Extraskeletal Calcifications in Children with Maintenance Peritoneal Dialysis
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Republic of Korea
- 2Department of Pediatrics, Uijeongbu Eulji Medical Center, Uijeongbu-si, Republic of Korea
- 3Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Republic of Korea
- 4Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
- 5Kidney Research Institute, Seoul National University College of Medicine, Seoul, Republic of Korea
- 6Wide River Institute of Immunology, Seoul National University, Hongcheon, Republic of Korea
- KMID: 2524513
- DOI: http://doi.org/10.3339/jkspn.2021.25.2.117
Abstract
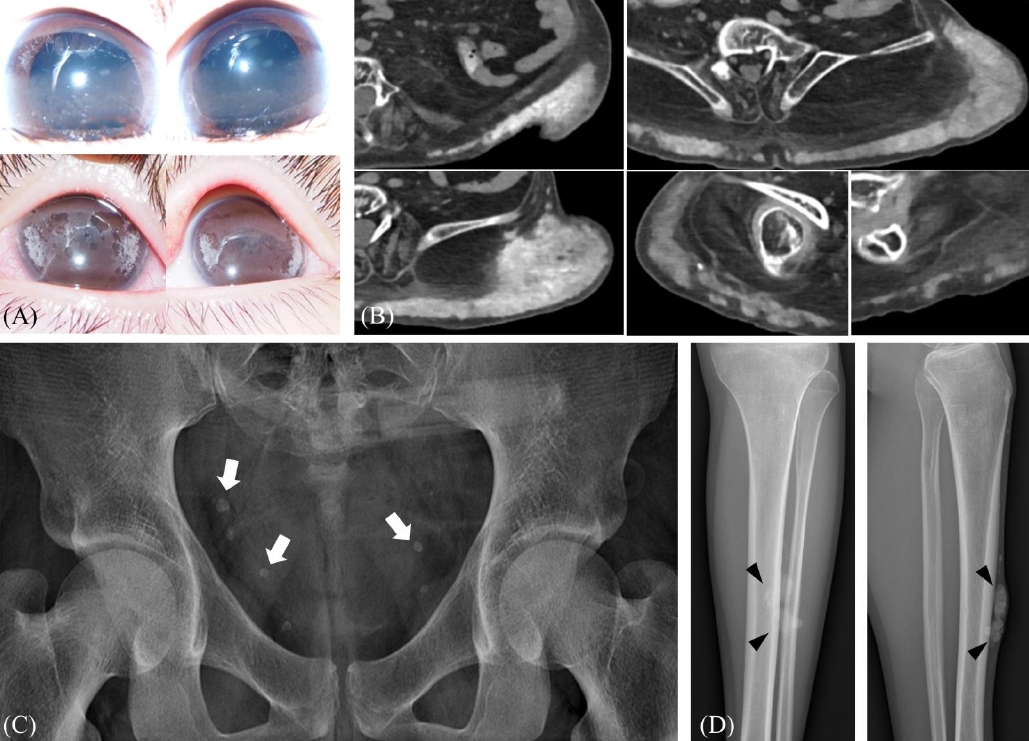
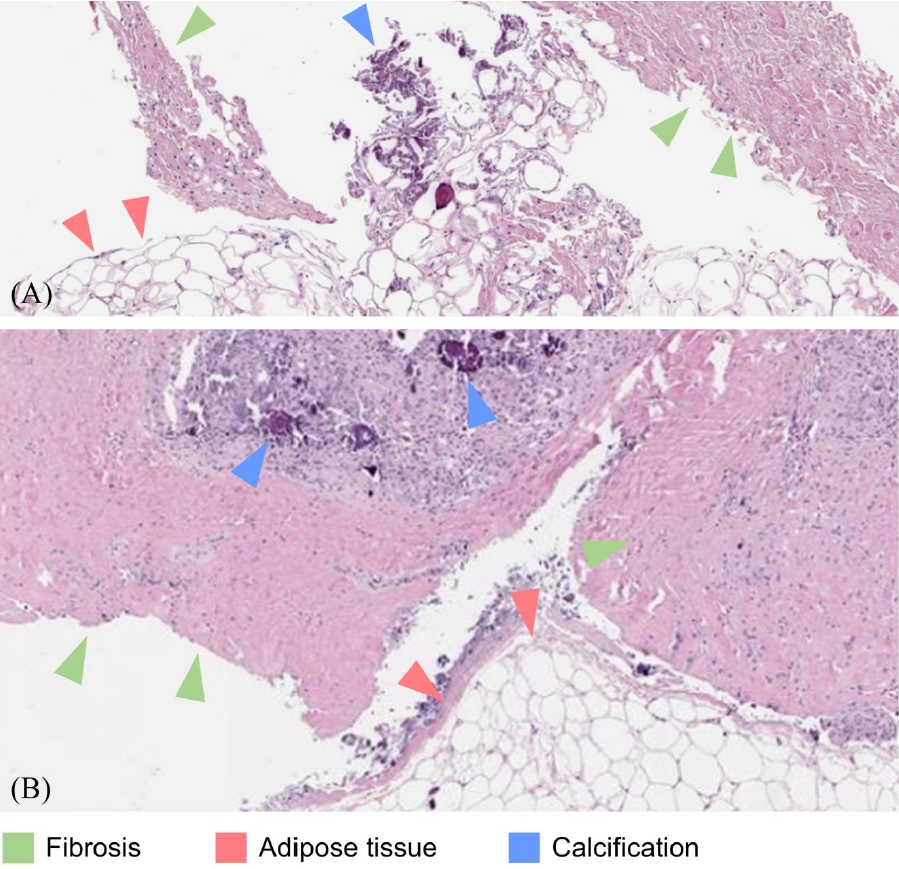
- Chronic kidney disease (CKD)-mineral and bone disorder (CKD-MBD) is a common complication of CKD, often accompanied by extra-skeletal calcification in adult patients. As increased vascular calcification is predicted to increase cardiovascular mortality and morbidity, the revised Kidney Disease: Improving Global Outcomes guidelines recommend avoiding calcium-containing phosphate chelators. However, extra-skeletal calcification is less commonly noticed in pediatric patients. Here, we report our experience of such a complication in pediatric patients receiving maintenance peritoneal dialysis. Extra-skeletal calcification was noticed at the corneas, pelvic cavity, and soft tissues of the lower leg in 4 out of 32 patients on maintenance peritoneal dialysis. These patients experienced the aggravation of extra-skeletal calcifications during peritoneal dialysis, and 2 of them underwent excisional operations. It is required to monitor extra-skeletal calcifications in children on kidney replacement therapy.
Keyword
Figure
Reference
-
References
1. Suh JS. Diagnosis and Management of Chronic Kidney DiseaseMineral Bone Disease in Children. Childhood Kidney Diseases. 2020; 24:14–8.
Article2. Heaf JG. Chronic Kidney Disease-Mineral Bone Disorder in the Elderly Peritoneal Dialysis Patient. Perit Dial Int. 2015; 35:640–4.
Article3. Goel SK, Bellovich K, McCullough PA. Treatment of severe metastatic calcification and calciphylaxis in dialysis patients. Int J Nephrol. 2011; 2011:70160.
Article4. Drüeke TB. A clinical approach to the uraemic patient with extraskeletal calcifications. Nephrology Dialysis Transplantation. 1996; 11:37–42.
Article5. Milliner DS, Zinsmeister AR, Lieberman E, Landing B. Soft tissue calcification in pediatric patients with end-stage renal disease. Kidney Int. 1990; 38:931–6.
Article6. Sheth RD, Perez MD, Goldstein SL. Cardiovascular calcifications in pediatric patients receiving maintenance dialysis. Pediatr Nephrol. 2003; 18:810–3.
Article7. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2017; 7:1–59.8. Wesseling K, Bakkaloglu S, Salusky I. Chronic kidney disease mineral and bone disorder in children. Pediatr Nephrol. 2008; 23:195–207.
Article9. Palit S, Kendrick J. Vascular calcification in chronic kidney disease: role of disordered mineral metabolism. Curr Pharm Des. 2014; 20:5829–33.
Article10. Kim C, Cheong HI, Kim JH, Yu YS, Kwon JW. Presumed atypical HDR syndrome associated with Band Keratopathy and pigmentary retinopathy. J Pediatr Ophthalmol Strabismus. 2011; 48 Online:e1–3.
Article11. Khouzam N, Wesseling-Perry K. Pathophysiology and treatment of cardiovascular disease in pediatric chronic kidney disease. Pediatr Nephrol. 2019; 34:1–10.
Article12. Fathallah-Shaykh S, Drozdz D, Flynn J, Jenkins R, Wesseling-Perry K, Swartz SJ, et al. Efficacy and safety of sevelamer carbonate in hyperphosphatemic pediatric patients with chronic kidney disease. Pediatr Nephrol. 2018; 33:325–33.
Article13. Toussaint N, Cooney P, Kerr PG. Review of dialysate calcium concentration in hemodialysis. Hemodial Int. 2006; 10:326–37.
Article14. Warady BA, Iles JN, Ariceta G, Dehmel B, Hidalgo G, Jiang X, et al. A randomized, double-blind, placebo-controlled study to assess the efficacy and safety of cinacalcet in pediatric patients with chronic kidney disease and secondary hyperparathyroidism receiving dialysis. Pediatr Nephrol. 2019; 34:475–86.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peritoneal dialysis in children and adolescents
- Peritoneal-pleural leak improved by switching from continuous ambulatory peritoneal dialysis to automated peritoneal dialysis
- Extensive Peritoneal Calcifications Associated with Continuous Ambulatory Peritoneal Dialysis
- A clinical study of continuous ambulatory peritoneal dialysis in childhood
- A Case of Conjunctival and Corneal Calcification in a Child on Peritoneal Dialysis