Anesth Pain Med.
2021 Oct;16(4):353-359. 10.17085/apm.21049.
Preoperative hyperlactatemia and early mortality after liver transplantation: selection of important variables using random forest survival analysis
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Laboratory for Cardiovascular Dynamics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Seoul Teunteun Neurosurgery, Wonju, Korea
- 3Department of Anesthesiology and Pain Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- KMID: 2524447
- DOI: http://doi.org/10.17085/apm.21049
Abstract
- Background
Generally, lactate levels > 2 mmol/L represent hyperlactatemia, whereas lactic acidosis is often defined as lactate > 4 mmol/L. Although hyperlactatemia is common finding in liver transplant (LT) candidates, association between lactate and organ failures with Acute-on-chronic Liver Failure (ACLF) is poorly studied. We searched the important variables for pre-LT hyperlactatemia and examined the impact of preoperative hyperlactatemia on early mortality after LT.
Methods
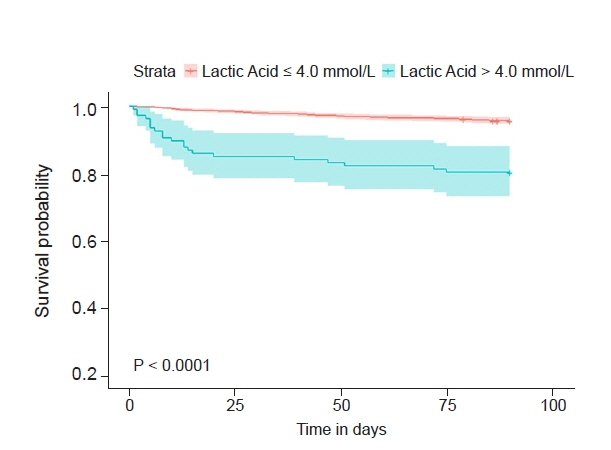
A total of 2,002 patients from LT registry between January 2008 and February 2019 were analyzed. Six organ failures (liver, kidney, brain, coagulation, circulation, and lung) were defined by criteria of EASL-CLIF ACLF Consortium. Variable importance of preoperative hyperlactatemia was examined by machine learning using random survival forest (RSF). Kaplan-Meier Survival curve analysis was performed to assess 90-day mortality.
Results
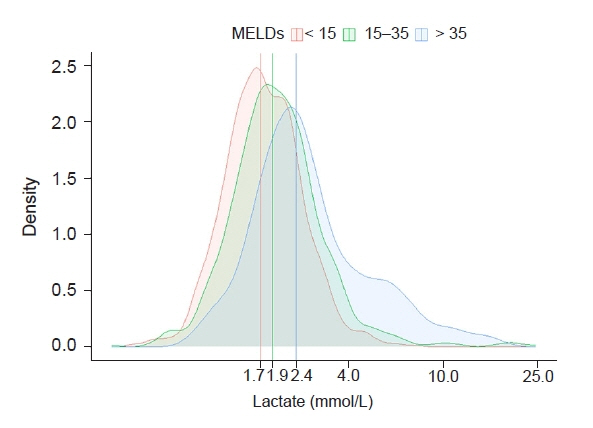
Median lactate level was 1.9 mmol/L (interquartile range: 1.4, 2.4 mmol/L) and 107 (5.3%) patients showed > 4.0 mmol/L. RSF analysis revealed that the four most important variables for hyperlactatemia were MELD score, circulatory failure, hemoglobin, and respiratory failure. The 30-day and 90-day mortality rates were 2.7% and 5.1%, whereas patients with lactate > 4.0 mmol/L showed increased rate of 15.0% and 19.6%, respectively.
Conclusion
About 50% and 5% of LT candidates showed pre-LT hyperlactatemia of > 2.0 mmol/L and > 4.0 mmol/L, respectively. Pre-LT lactate > 4.0 mmol/L was associated with increased early post-LT mortality. Our results suggest that future study of correcting modifiable risk factors may play a role in preventing hyperlactatemia and lowering early mortality after LT.
Figure
Reference
-
1. Cardoso FS, Abraldes JG, Sy E, Ronco JJ, Bagulho L, Mcphail MJ, et al. Lactate and number of organ failures predict intensive care unit mortality in patients with acute-on-chronic liver failure. Liver Int. 2019; 39:1271–80.2. Sundaram V, Jalan R, Wu T, Volk ML, Asrani SK, Klein AS, et al. Factors associated with survival of patients with severe acute-on-chronic liver failure before and after liver transplantation. Gastroenterology. 2019; 156:1381–91.e3.3. Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. 2020; 46(Suppl 1):10–67.4. Jeppesen JB, Mortensen C, Bendtsen F, Møller S. Lactate metabolism in chronic liver disease. Scand J Clin Lab Invest. 2013; 73:293–9.5. Jalan R, Saliba F, Pavesi M, Amoros A, Moreau R, Ginès P, et al. CANONIC study investigators of the EASL-CLIF Consortium. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol. 2014; 61:1038–47.6. Hsich E, Gorodeski EZ, Blackstone EH, Ishwaran H, Lauer MS. Identifying important risk factors for survival in patient with systolic heart failure using random survival forests. Circ Cardiovasc Qual Outcomes. 2011; 4:39–45.7. Ishwaran H, Kogalur UB. Consistency of random survival forests. Stat Probab Lett. 2010; 80:1056–64.8. O'Brien RC, Ishwaran H, Szczotka-Flynn LB, Lass JH; Cornea Preservation Time Study (CPTS) Group. Random survival forests analysis of intraoperative complications as predictors of descemet stripping automated endothelial keratoplasty graft failure in the cornea preservation time study. JAMA Ophthalmol. 2021; 139:191–7.9. Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 2018; 44:925–8.10. Drolz A, Horvatits T, Rutter K, Landahl F, Roedl K, Meersseman P, et al. Lactate improves prediction of short-term mortality in critically ill patients with cirrhosis: a multinational study. Hepatology. 2019; 69:258–69.11. Choudhury A, Jindal A, Maiwall R, Sharma MK, Sharma BC, Pamecha V, et al. APASL ACLF Working Party. Liver failure determines the outcome in patients of acute-on-chronic liver failure (ACLF): comparison of APASL ACLF research consortium (AARC) and CLIF-SOFA models. Hepatol Int. 2017; 11:461–71.12. Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014; 371:2309–19.13. Macquillan GC, Seyam MS, Nightingale P, Neuberger JM, Murphy N. Blood lactate but not serum phosphate levels can predict patient outcome in fulminant hepatic failure. Liver Transpl. 2005; 11:1073–9.14. Freeman RB Jr, Wiesner RH, Harper A, McDiarmid SV, Lake J, Edwards E, et al. UNOS/OPTN Liver Disease Severity Score, UNOS/OPTN Liver and Intestine, and UNOS/OPTN Pediatric Transplantation Committees. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002; 8:851–8.15. Adamo L, Nassif ME, Novak E, LaRue SJ, Mann DL. Prevalence of lactic acidaemia in patients with advanced heart failure and depressed cardiac output. Eur J Heart Fail. 2017; 19:1027–33.16. Ishwaran H, Gerds TA, Kogalur UB, Moore RD, Gange SJ, Lau BM. Random survival forests for competing risks. Biostatistics. 2014; 15:757–73.17. Tang F, Ishwaran H. Random forest missing data algorithms. Stat Anal Data Min. 2017; 10:363–77.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Indication of Pediatric Liver Transplantation
- Intraoperative lactic acid concentration during liver transplantation and cutoff values to predict early mortality: a retrospective analysis of 3,338 cases
- Liver Transplantation for Hepatocellular Carcinoma
- Transplantation Techniques Unique in Pediatric Liver Transplantation
- Changes of Pulmonary Artery Pressure during Liver Transplantation