Anesth Pain Med.
2021 Oct;16(4):338-343. 10.17085/apm.21022.
Awake craniotomy using a high-flow nasal cannula with oxygen reserve index monitoring - A report of two cases -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Dankook University Dental Hospital, Cheonan, Korea
- 3Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2524445
- DOI: http://doi.org/10.17085/apm.21022
Abstract
- Background
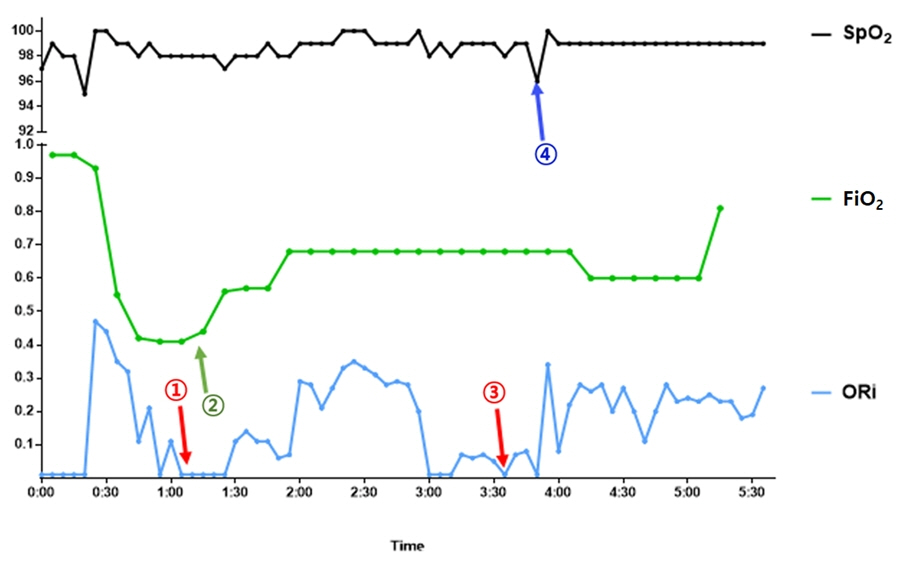
Awake craniotomy is a well-tolerated procedure for the resection of brain tumors residing within or close to the eloquent cortical areas. Monitored anesthesia care (MAC) is a dominant anesthetic approach for awake craniotomy; however, it is associated with inherent challenges such as desaturation and hypercapnia, which may lead to various complications. The prevention of respiratory insufficiency is important for successful awake craniotomy. As measures to avoid respiratory depression, the use of high-flow nasal cannula (HFNC) can improve patient oxygenation and monitor the oxygen reserve index (ORi) to detect hypoxia earlier. Case: We report two cases of awake craniotomy with MAC using HFNC and ORi. We adjusted the fraction of inspired oxygen of the HFNC according to the ORi level. The patient underwent successful awake craniotomy without a desaturation event or additional airway intervention.
Conclusions
Combined HFNC and ORi monitoring may provide adequate oxygen reserves in patients undergoing awake craniotomy.
Keyword
Figure
Reference
-
1. Hervey-Jumper SL, Li J, Lau D, Molinaro AM, Perry DW, Meng L, et al. Awake craniotomy to maximize glioma resection: methods and technical nuances over a 27-year period. J Neurosurg. 2015; 123:325–39.2. Kim SH, Choi SH. Anesthetic considerations for awake craniotomy. Anesth Pain Med (Seoul). 2020; 15:269–74.3. Smith SC, Burbridge M, Jaffe R. High flow nasal cannula, a novel approach to airway management in awake craniotomies. J Neurosurg Anesthesiol. 2018; 30:382.4. Wong JWM, Kong AHS, Lam SY, Woo PYM. High-flow nasal oxygen in patient with obstructive sleep apnea undergoing awake craniotomy: a case report. A A Case Rep. 2017; 9:353–6.5. Scheeren TWL, Belda FJ, Perel A. The oxygen reserve index (ORI): a new tool to monitor oxygen therapy. J Clin Monit Comput. 2018; 32:379–89.6. Fleming NW, Singh A, Lee L, Applegate RL 2nd. Oxygen reserve index: utility as an early warning for desaturation in high-risk surgical patients. Anesth Analg. 2021; 132:770–6.7. Davis DP, Hwang JQ, Dunford JV. Rate of decline in oxygen saturation at various pulse oximetry values with prehospital rapid sequence intubation. Prehosp Emerg Care. 2008; 12:46–51.8. Amato AC, Pescatori M. Effect of perioperative blood transfusions on recurrence of colorectal cancer: meta-analysis stratified on risk factors. Dis Colon Rectum. 1998; 41:570–85.9. Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care. 2011; 56:1151–5.10. Jeong JH, Kim DH, Kim SC, Kang C, Lee SH, Kang TS, et al. Changes in arterial blood gases after use of high-flow nasal cannula therapy in the ED. Am J Emerg Med. 2015; 33:1344–9.11. Applegate RL 2nd, Dorotta IL, Wells B, Juma D, Applegate PM. The relationship between oxygen reserve index and arterial partial pressure of oxygen during surgery. Anesth Analg. 2016; 123:626–33.12. Szmuk P, Steiner JW, Olomu PN, Ploski RP, Sessler DI, Ezri T. Oxygen reserve index: a novel noninvasive measure of oxygen reserve--a pilot study. Anesthesiology. 2016; 124:779–84.13. Schaffranietz L, Vetter B, Rudolph C, König F. [Hyperoxia-induced liberation of big-endothelin into jugular venous blood of electric neurosurgical patients]. Anaesthesiol Reanim. 2001; 26:123–32. German.14. Lumb AB, Walton LJ. Perioperative oxygen toxicity. Anesthesiol Clin. 2012; 30:591–605.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study on the Changes of SaO2, According to the Different Type of Oxygen Suppliers
- The Effect of Different Oxygen Flow Rates on Arterial Oxygenation and End-Tidal CO2 Measurements via a Nasal Cannula in Spinal Anesthesia
- Factors about Failure after High Flow Oxygen through Nasal Cannula Therapy in Hypoxic Respiratory Failure Patients at Emergency Department Presentation
- Development of Nursing Practice Guidelines for Non-humidified Low Flow Oxygen Therapy by Nasal Cannula
- High Flow Nasal Cannula Assisted Tracheostomy for Securing Airways in Patients with Acute Respiratory Distress Induced by Glottic Cancer