Anat Cell Biol.
2021 Dec;54(4):441-447. 10.5115/acb.21.081.
Anatomy of lacrimal sac fossa affecting success rate in endoscopic and external dacryocystorhinostomy surgery in Mongolians
- Affiliations
-
- 1Department of Ophthalmology, Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia
- 2Department of Anatomy, Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia
- KMID: 2523575
- DOI: http://doi.org/10.5115/acb.21.081
Abstract
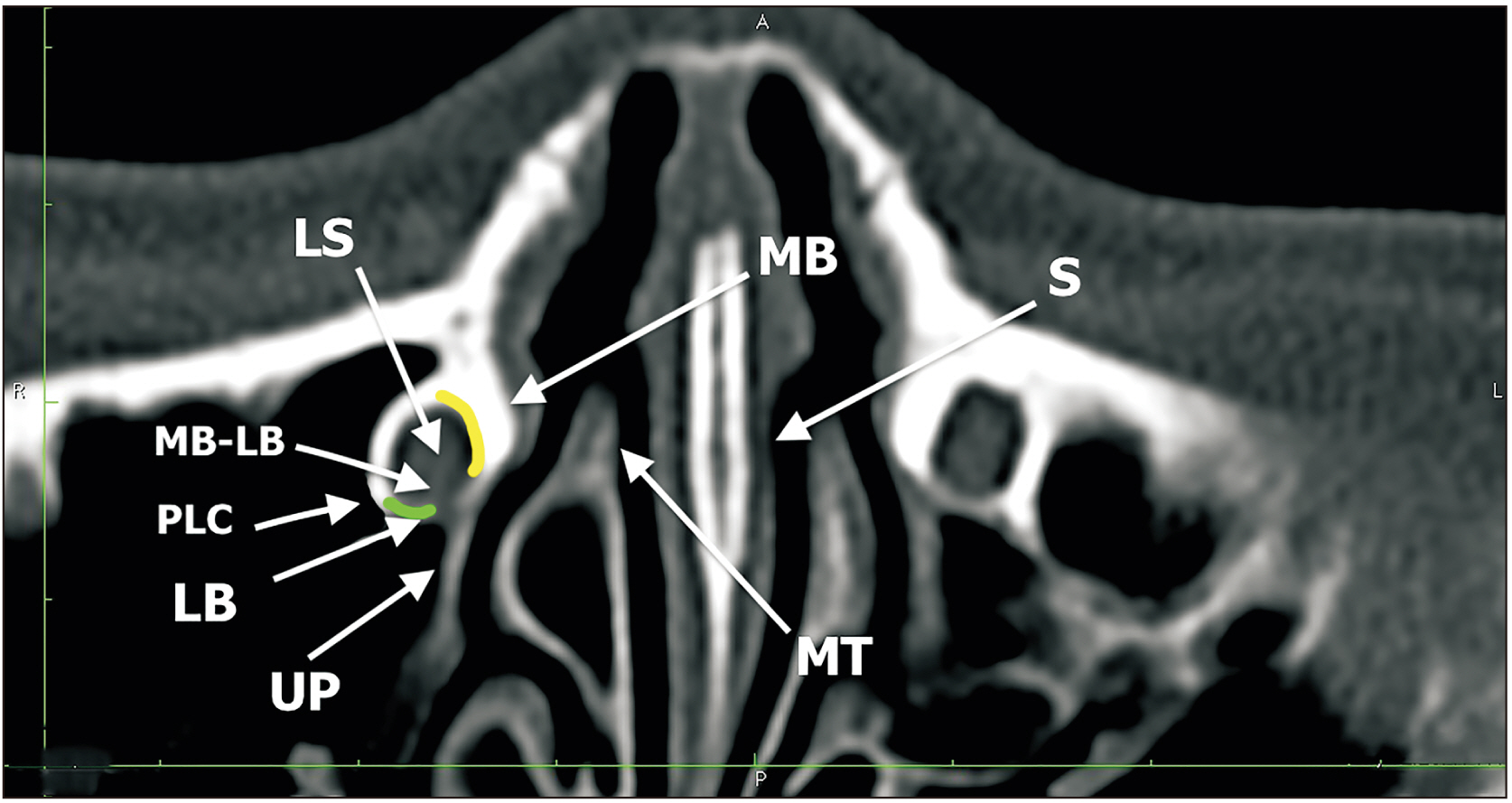
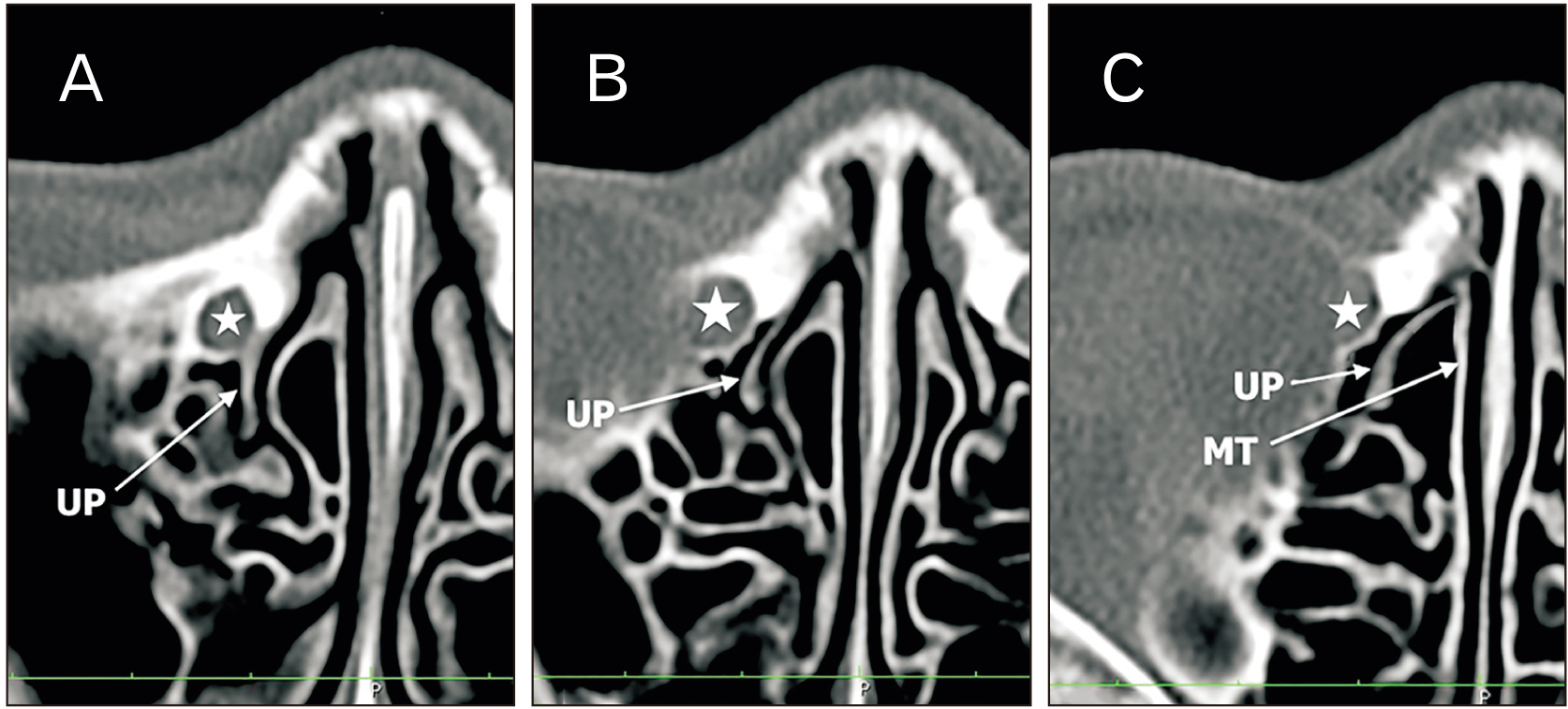
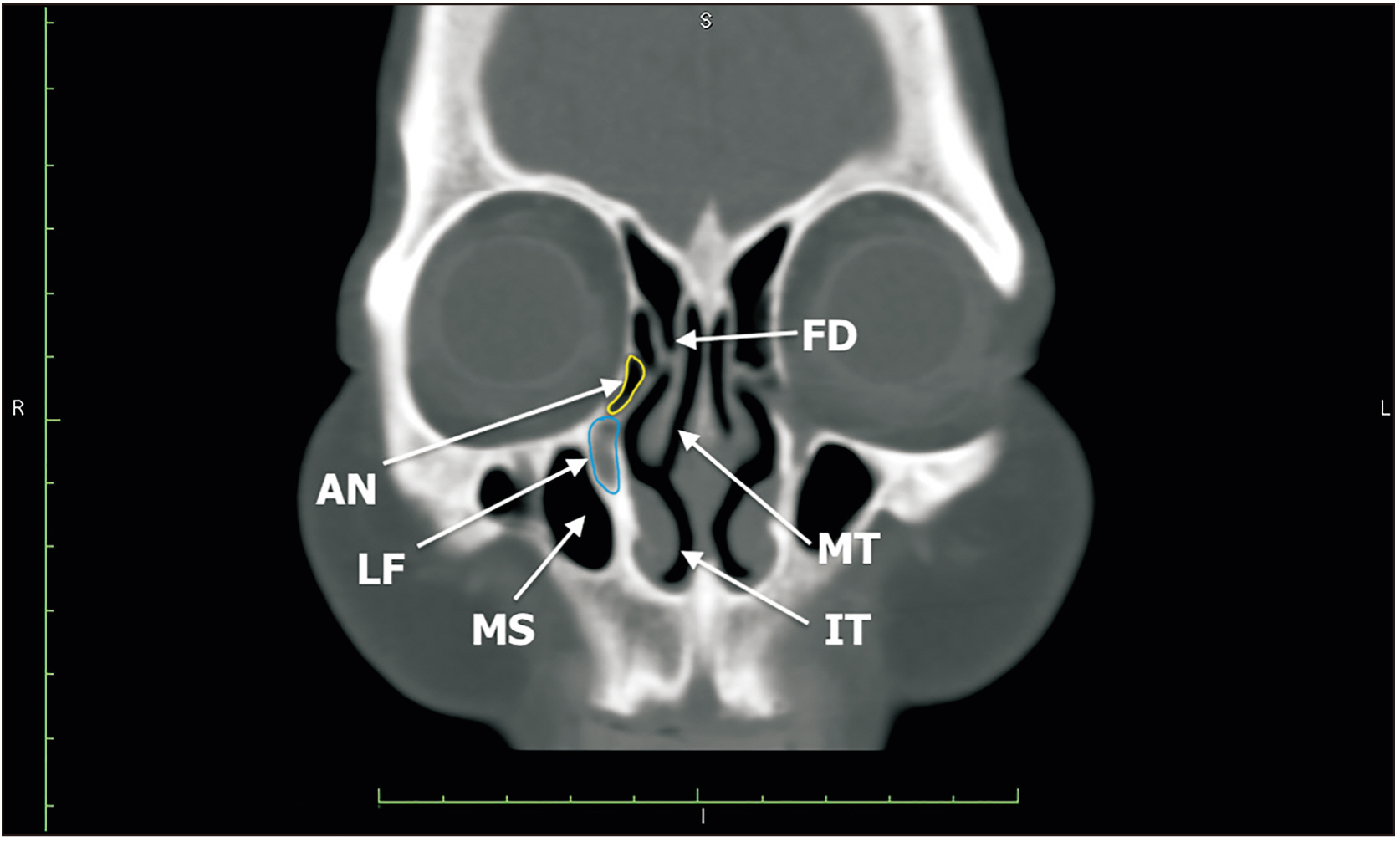
- To study the affect of anatomical variance of lacrimal sac fossa on dacryocystorhinostomies (DCR) performed by the traditional external (EX-DCR) approach or an endoscopic (EN-DCR) endonasal approach. A total of 292 consecutive cases with primary nasolacrimal obstruction underwent DCR surgery. Orbital computed tomography scan was used to measure lacrimal sac fossa and other related structures and Lac-Q questionnaire was used to compare surgery result. Maxillary portion of lacrimal sac fossa is thicker in failed surgery group than successful surgery group (P<0.05). Lateral nasal structures (uncinate process, operculum of the middle turbinate, agger nasi) are dominantly adjusting to lacrimal sac fossa in failed surgery group (P<0.05). Patients who underwent EX-DCR has a 6.0-point and EN-DCR group 11.0-point improvement (P<0.016) in Lac-Q questionnaire. Patients who have a thick frontal process of the maxilla and uncinate process, operculum of the middle turbinate, ethmoid cells adjusting to lacrimal fossa are prone to have recurrence of nasolacrimal duct obstruction after DCR surgery. The EN-DCR and the EX-DCR approach have an equivalent surgical success rate but improvement in quality of life by using the Lac-Q questionnaire is greater in the endoscopic group when compared with the external.
Keyword
Figure
Cited by 1 articles
-
Computed tomographic assessment of the lacrimal sac fossa in southwest population of Iran
Samad Shahryari, Mohammad Ghasem Hanafi, Rouhangiz Kamankesh, Atefeh Mahdianrad, Ali Reza Eftekhari Moghadam
Anat Cell Biol. 2022;55(3):277-283. doi: 10.5115/acb.22.001.
Reference
-
References
1. Walker RA, Al-Ghoul A, Conlon MR. 2011; Comparison of nonlaser nonendoscopic endonasal dacryocystorhinostomy with external dacryocystorhinostomy. Can J Ophthalmol. 46:191–5. DOI: 10.3129/i10-096. PMID: 21708090.
Article2. Bulbul E, Yazici A, Yanik B, Yazici H, Demirpolat G. 2016; Morphometric evaluation of bony nasolacrimal canal in a Caucasian population with primary acquired nasolacrimal duct obstruction: a multidetector computed tomography study. Korean J Radiol. 17:271–6. DOI: 10.3348/kjr.2016.17.2.271. PMID: 26957913. PMCID: PMC4781767.
Article3. Dolman PJ. 2003; Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Ophthalmology. 110:78–84. DOI: 10.1016/S0161-6420(02)01452-5. PMID: 12511350.
Article4. Wong WK, Dean S, Nair S. 2018; Comparison between endoscopic and external dacryocystorhinostomy by using the Lacrimal Symptom Questionnaire: a pilot study. Am J Rhinol Allergy. 32:46–51. DOI: 10.2500/ajra.2018.32.4494. PMID: 29336290.
Article5. Fayet B, Racy E, Assouline M, Zerbib M. 2005; Surgical anatomy of the lacrimal fossa a prospective computed tomodensitometry scan analysis. Ophthalmology. 112:1119–28. DOI: 10.1016/j.ophtha.2005.01.012. PMID: 15885790.6. Fayet B, Racy E, Assouline M. 2004; Complications of standardized endonasal dacryocystorhinostomy with unciformectomy. Ophthalmology. 111:837–45. DOI: 10.1016/j.ophtha.2003.08.023. PMID: 15051221.7. Woo KI, Maeng HS, Kim YD. 2011; Characteristics of intranasal structures for endonasal dacryocystorhinostomy in asians. Am J Ophthalmol. 152:491–8.e1. DOI: 10.1016/j.ajo.2011.02.019. PMID: 21669403.
Article8. Sham CL, van Hasselt CA. 2000; Endoscopic terminal dacryocystorhinostomy. Laryngoscope. 110:1045–9. DOI: 10.1097/00005537-200006000-00029. PMID: 10852528.
Article9. Zhang T, Wang J, Wang L, Shan Y, Wang Q. 2003; The clinical anatomy of lacrimal sac fossa. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 17:652–3. Chinese. PMID: 14971197.10. Steadman MG. 1985; Transnasal dacryocystorhinostomy. Otolaryngol Clin North Am. 18:107–11. DOI: 10.1016/S0030-6665(20)31898-3. PMID: 3991199.11. Hartikainen J, Aho HJ, Seppä H, Grenman R. 1996; Lacrimal bone thickness at the lacrimal sac fossa. Ophthalmic Surg Lasers. 27:679–84. DOI: 10.3928/1542-8877-19960801-07. PMID: 8858634.
Article12. McDonogh M, Meiring JH. 1989; Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 103:585–7. DOI: 10.1017/S0022215100109405. PMID: 2769026.
Article13. Yung MW, Logan BM. 1999; The anatomy of the lacrimal bone at the lateral wall of the nose: its significance to the lacrimal surgeon. Clin Otolaryngol Allied Sci. 24:262–5. DOI: 10.1046/j.1365-2273.1999.00235.x. PMID: 10472456.
Article14. Ye H, Feng Y, Yin S. 2007; Anatomy study of the lacrimal bone in dacryocystorhinostomy. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 21:774–6. Chinese. PMID: 17993012.15. Shigeta K, Takegoshi H, Kikuchi S. 2007; Sex and age differences in the bony nasolacrimal canal: an anatomical study. Arch Ophthalmol. 125:1677–81. DOI: 10.1001/archopht.125.12.1677. PMID: 18071122.16. Tarbet KJ, Custer PL. 1995; External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology. 102:1065–70. DOI: 10.1016/S0161-6420(95)30910-4. PMID: 9121754.17. Hartikainen J, Grenman R, Puukka P, Seppä H. 1998; Prospective randomized comparison of external dacryocystorhinostomy and endonasal laser dacryocystorhinostomy. Ophthalmology. 105:1106–13. DOI: 10.1016/S0161-6420(98)96015-8. PMID: 9627664.
Article18. Hester KM, Rahimi OB, Fry CL, Nation HL. 2021; Apr. 8. A cadaveric study investigating the anatomy of the medial orbital wall. Anat Cell Biol. [Epub]. https://doi.org/10.5115/acb.21.013. DOI: 10.5115/acb.21.013. PMID: 33827992. PMCID: PMC8493022.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Success Rate of Endonasal Dacryocystorhinostomy Based on the Location of the Lacrimal Sac
- Correlation between nasal mucosal thickness around the lacrimal sac fossa and surgical outcomes in endonasal dacryocystorhinostomy
- Posterior Lacrimal Sac Approach in Endoscopic Dacryocystorhinostomy
- The Correlation between Organisms Cultured from the Lacrimal Sac and Lacrimal Punctum in Dacryocystitis
- Results of Endoscopic Dacryocystorhinostomy for the Nasolacrimal Duct Obstruction