Kosin Med J.
2018 Dec;33(3):358-368. 10.7180/kmj.2018.33.3.358.
Correlation between nasal mucosal thickness around the lacrimal sac fossa and surgical outcomes in endonasal dacryocystorhinostomy
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Kosin University, Busan, Korea. hhiatus@gmail.com
- 2Department of Anesthesiology and Pain Medicine, Ulsan University Hospital, College of Medicine, Ulsan University, Ulsan, Korea.
- 3Institute for Medicine, College of Medicine, Kosin University, Busan, Korea.
- KMID: 2442546
- DOI: http://doi.org/10.7180/kmj.2018.33.3.358
Abstract
OBJECTIVES
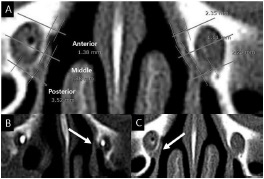
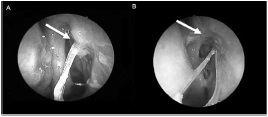
To identify the relationship between surgical success rate and preoperative nasal mucosal thickness around the lacrimal sac fossa, as measured using computed tomography.
METHODS
We reviewed 33 eyes from 27 patients who underwent endoscopic dacryocystorhinostomy after diagnosis of primary nasolacrimal duct obstruction and who were followed-up with for at least six months between 2011 and 2014. We measured preoperative nasal mucosal thickness around the bony lacrimal sac fossa using computed tomography and analyzed patient measurements after classifying them into three groups: the successfully operated group, the failed operation group, and the non-operated group.
RESULTS
Surgery failed in six of the 33 eyes because of a granuloma at the osteotomy site and synechial formation of the nasal mucosa. The failed-surgery group showed a clinically significantly greater decrease in nasal mucosal thickness at the rearward lacrimal sac fossa compared with the successful-surgery group. However, nasal mucosal thickness of fellow eyes (i.e., non-operated eyes) was not significantly different between the two groups, and the location of the uncinate process did not appear to influence mucosal thickness. In the failed group, posteriorly located mucosal thickness of operated eye fossa was thinner than that of the non-operated eyes, but not significantly so.
CONCLUSIONS
Our results from this quantitative anatomical study suggest that nasal mucosal thickness is a predictor of endoscopic dacryocystorhinostomy results.
Figure
Reference
-
1. Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976–2000 (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007; 105:649–666.2. Dietrich C, Mewes T, Kühnemund M, Hashemi B, Mann WJ, Amedee RG. Long-term follow-up of patients with microscopic endonasal dacryocystorhinostomy. Am J Rhinol. 2003; 17:57–61.
Article3. Hartikainen J, Antila J, Varpula M, Puukka P, Seppä H, Grénman R. Prospective randomized comparison of endonasal endoscopic dacryocystorhinostomy and external dacryocystorhinostomy. Laryngoscope. 1998; 108:1861–1866.
Article4. Leong SC, Karkos PD, Burgess P, Halliwell M, Hampal S. A comparison of outcomes between nonlaser endoscopic endonasal and external dacryocystorhinostomy: single-center experience and a review of British trends. Am J Otolaryngol. 2010; 31:32–37.
Article5. Leong SC, Macewen CJ, White PS. A systematic review of outcomes after dacryocystorhinostomy in adults. Am J Rhinol Allergy. 2010; 24:81–90.
Article6. Allen KM, Berlin AJ, Levine HL. Intranasal endoscopic analysis of dacrocystorhinostomy failure. Ophthalmic Plast Reconstr Surg. 1988; 4:143–145.7. Nussbaumer M, Schreiber S, Yung MW. Concomitant nasal procedures in endoscopic dacryocystorhinostomy. J Laryngol Otol. 2004; 118:267–269.
Article8. Goldberg RA. Endonasal dacryocystorhinostomy: is it really less successful? Arch Ophthalmol. 2004; 122:108–110.9. Ali MJ, Mishra DK, Baig F, Naik MN. Histopathology, Immunohistochemistry, and Electron Microscopic features of a Dacryocystorhinostomy Ostium Cicatrix. Ophthalmic Plast Reconstr Surg. 2016; 32:333–336.
Article10. Ali MJ, Baig F, Lakshman M, Naik MN. Electron microscopic features of nasal mucosa treated with topical and circumostial injection of mitomycin C: implications in dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg. 2015; 31:103–107.
Article11. Heindl LM, Junemann A, Holbach LM. A clinicopathologic study of nasal mucosa in 350 patients with external dacryocystorhinostomy. Orbit. 2009; 28:7–11.
Article12. Mauriello JA Jr, Palydowycz S, DeLuca J. Clinicopathologic study of lacrimal sac and nasal mucosa in 44 patients with complete acquired nasolacrimal duct obstruction. Ophthalmic Plast Reconstr Surg. 1992; 8:13–21.
Article13. Onerci M, Orhan M, Ogretmenoğlu O, Irkec M. Long-term results and reasons for failure of intranasal endoscopic dacryocystorhinostomy. Acta Otolaryngol. 2000; 120:319–322.
Article14. Fayet B, Racy E, Assouline M. Systematic unciformectomy for a standardized endonasal dacryocystorhinostomy. Ophthalmology. 2002; 109:530–536.
Article15. Häusler R, Caversaccio M. Microsurgical endonasal dacryocystorhinostomy with long-term insertion of bicanalicular silicone tubes. Arch Otolaryngol Head Neck Surg. 1998; 124:188–191.
Article16. Jokinen K, Kärjä J. Endonasal dacryocystorhinostomy. Arch Otolaryngol. 1974; 100:41–44.
Article17. Wilhelm DL. Regeneration of tracheal epithelium. J Pathol Bacteriol. 1953; 65:543–550.
Article18. Watelet JB, Bachert C, Gevaert P, Van Cauwenberge P. Wound healing of the nasal and paranasal mucosa: a review. Am J Rhinol. 2002; 16:77–84.
Article19. Wynn TA. Cellular and molecular mechanisms of fibrosis. J Pathol. 2008; 214:199–210.
Article20. Smirnov G, Pirinen R, Tuomilehto H, Seppä J, Teräsvirta M, Uusitalo H, et al. Strong expression of HSP47 in metaplastic nasal mucosa may predict a poor outcome after primary endoscopic dacryocystorhinostomy: a prospective study. Acta Ophthalmol. 2011; 89:e132–e136.
Article21. Gul A, Aslan K, Karli R, Ariturk N, Can E. A Possible Cause of Nasolacrimal Duct Obstruction: Narrow Angle Between Inferior Turbinate and Upper Part of the Medial Wall of the Maxillary Sinus. Curr Eye Res. 2016; 41:729–733.
Article22. Yong AM, Zhao DB, Siew SC, Goh PS, Liao J, Amrith S. Assessment of bony nasolacrimal parameters among Asians. Ophthalmic Plast Reconstr Surg. 2014; 30:322–327.
Article23. McCormick A, Sloan B. The diameter of the nasolacrimal canal measured by computed tomography: gender and racial differences. Clin Exp Ophthalmol. 2009; 37:357–361.
Article24. Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 3. Ophthalmic Plast Reconstr Surg. 1993; 9:11–26.25. Onerci M. Dacryocystorhinostomy. Diagnosis and treatment of nasolacrimal canal obstructions. Rhinology. 2002; 40:49–65.26. Ly TH, deShazo RD, Olivier J, Stringer SP, Daley W, Stodard CM. Diagnostic criteria for atrophic rhinosinusitis. Am J Med. 2009; 122:747–753.
Article27. Fayet B, Racy E, Assouline M. Complications of standardized endonasal dacryocystorhinostomy with unciformectomy. Ophthalmology. 2004; 111:837–845.
Article28. Fayet B, Racy E, Assouline M, Zerbib M. Surgical anatomy of the lacrimal fossa a prospective computed tomodensitometry scan analysis. Ophthalmology. 2005; 112:1119–1128.
Article29. Woo KI, Maeng HS, Kim YD. Characteristics of intranasal structures for endonasal dacryocystorhinostomy in asians. Am J Ophthalmol. 2011; 152:491–498.e1.
Article30. Yang JW, Oh HN. Success rate and complications of endonasal dacryocystorhinostomy with unciformectomy. Graefes Arch Clin Exp Ophthalmol. 2012; 250:1509–1513.
Article31. Jung SK, et al. Surgical outcomes of endoscopic dacryocystorhinostomy: analysis of 1083 consecutive cases. Can J Ophthalmol. 2015; 50:466–470.
Article32. Karim R, et al. A comparison of external and endoscopic endonasal dacryocystorhinostomy for acquired nasolacrimal duct obstruction. Clin Ophthalmol. 2011; 5:979–989.
Article33. Herzallah I, et al. Endoscopic Dacryocystorhinostomy (DCR): a comparative study between powered and non-powered technique. J Otolaryngol Head Neck Surg. 2015; 44:56.
Article34. Sarode D, et al. The benefit of silicone stents in primary endonasal dacryocystorhinostomy: a systematic review and meta-analysis. Clin Otolaryngol. 2017; 42:307–314.
Article35. Kim SY, et al. No thermal tool using methods in endoscopic dacryocystorhinostomy: no cautery, no drill, no illuminator, no more tears. Eur Arch Otorhinolaryngol. 2013; 270:2677–2682.
Article36. Beshay N, Ghabrial R. Anatomical and subjective success rates of endonasal dacryocystorhinostomy over a seven-year period. Eye (Lond). 2016; 30:1458–1461.
Article37. Kostis WJ, et al. Small pulmonary nodules: reproducibility of three-dimensional volumetric measurement and estimation of time to follow-up CT. Radiology. 2004; 231:446–452.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcome of Endonasal Dacryocystorhinostomy with Nasal and Lacrimal Sac Mucosal Flaps
- Clinical Outcomes of Endonasal Dacryocystorhinostomy Using Fibrin Glue for Lacrimal Sac and Nasal Mucosal Flaps
- Effect of Lacrimal Sac Incision Using Keratome in Endonasal Dacryocystorhinostomy
- Success Rate of Endonasal Dacryocystorhinostomy Based on the Location of the Lacrimal Sac
- The Correlation between Organisms Cultured from the Lacrimal Sac and Lacrimal Punctum in Dacryocystitis