Ann Hepatobiliary Pancreat Surg.
2021 Nov;25(4):556-561. 10.14701/ahbps.2021.25.4.556.
Intraductal tubulopapillary neoplasms of the pancreas and biliary tract: The black swan of hepatobiliary surgery
- Affiliations
-
- 1Department of Surgery, University of Connecticut School of Medicine, Farmington, CT, United States
- 2Department of Pathology and Laboratory Medicine, Hartford Hospital, Hartford, CT, United States
- 3Hartford Hospital Transplant Program & Comprehensive Liver Center, Hartford, CT, United States
- KMID: 2523063
- DOI: http://doi.org/10.14701/ahbps.2021.25.4.556
Abstract
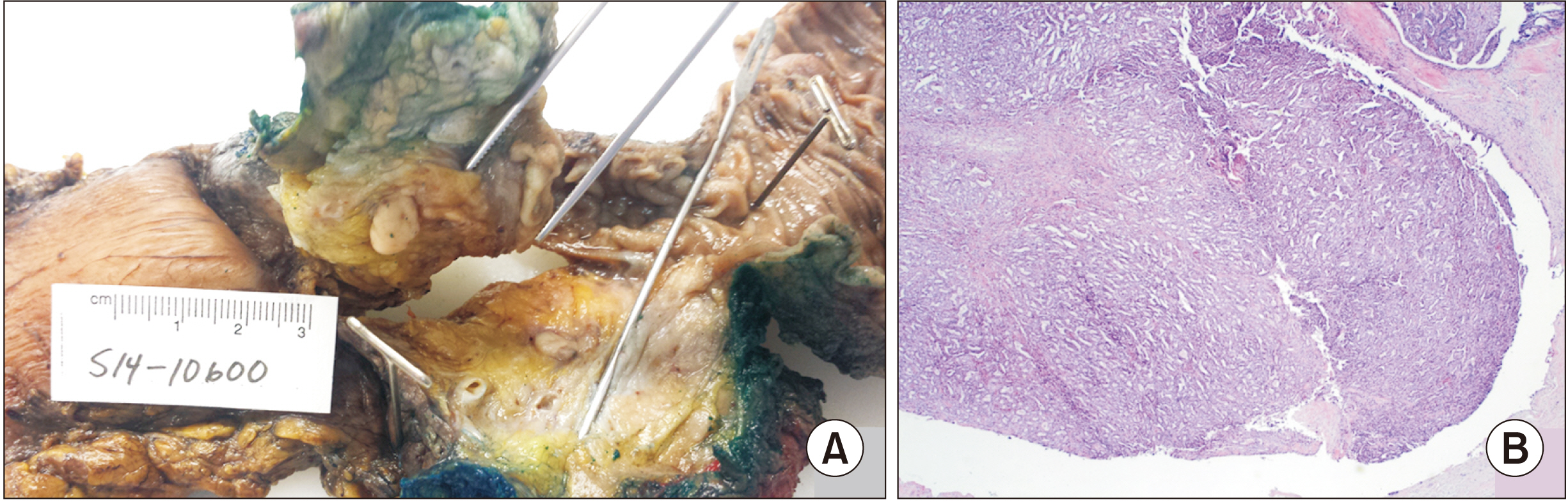
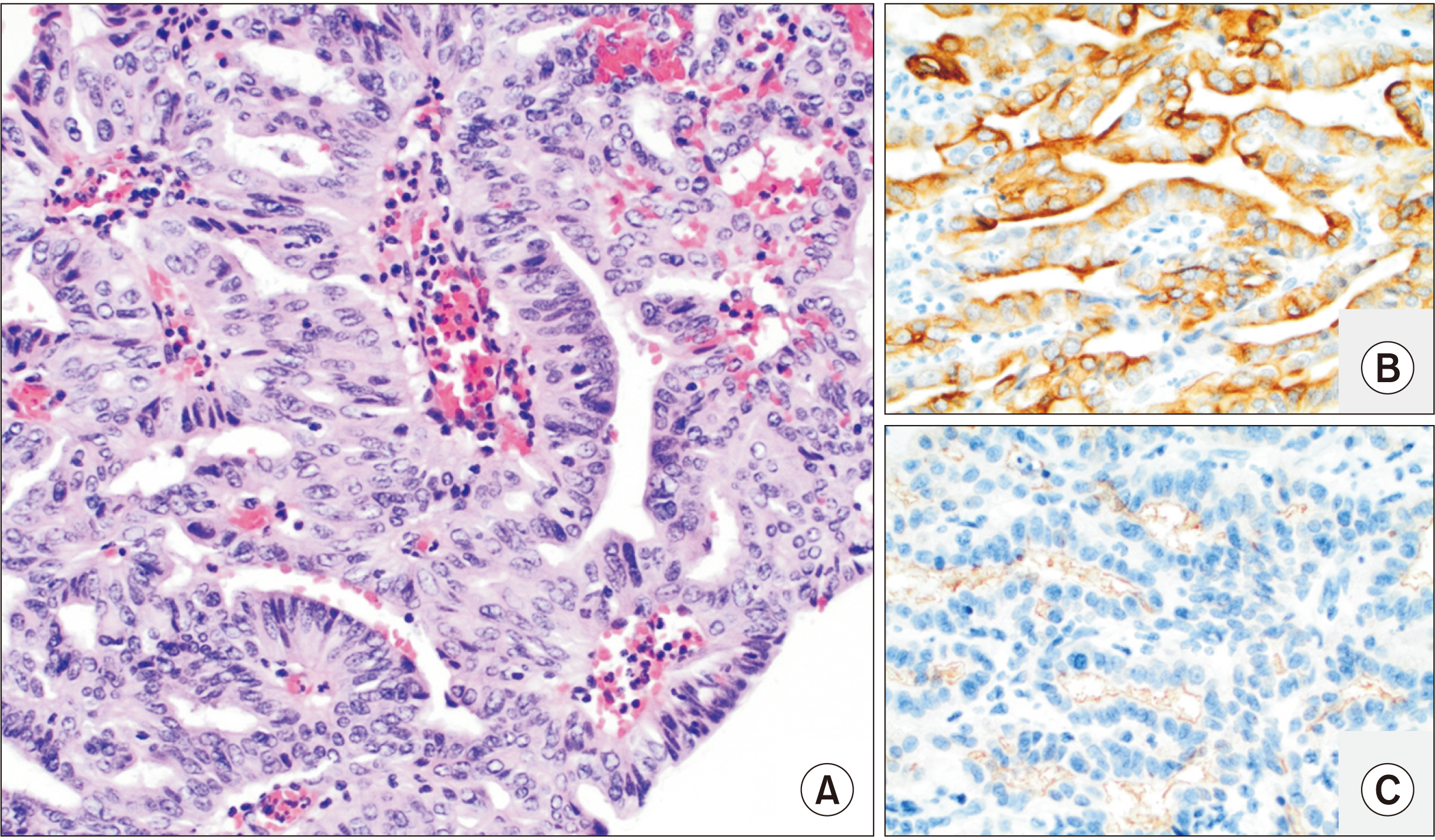
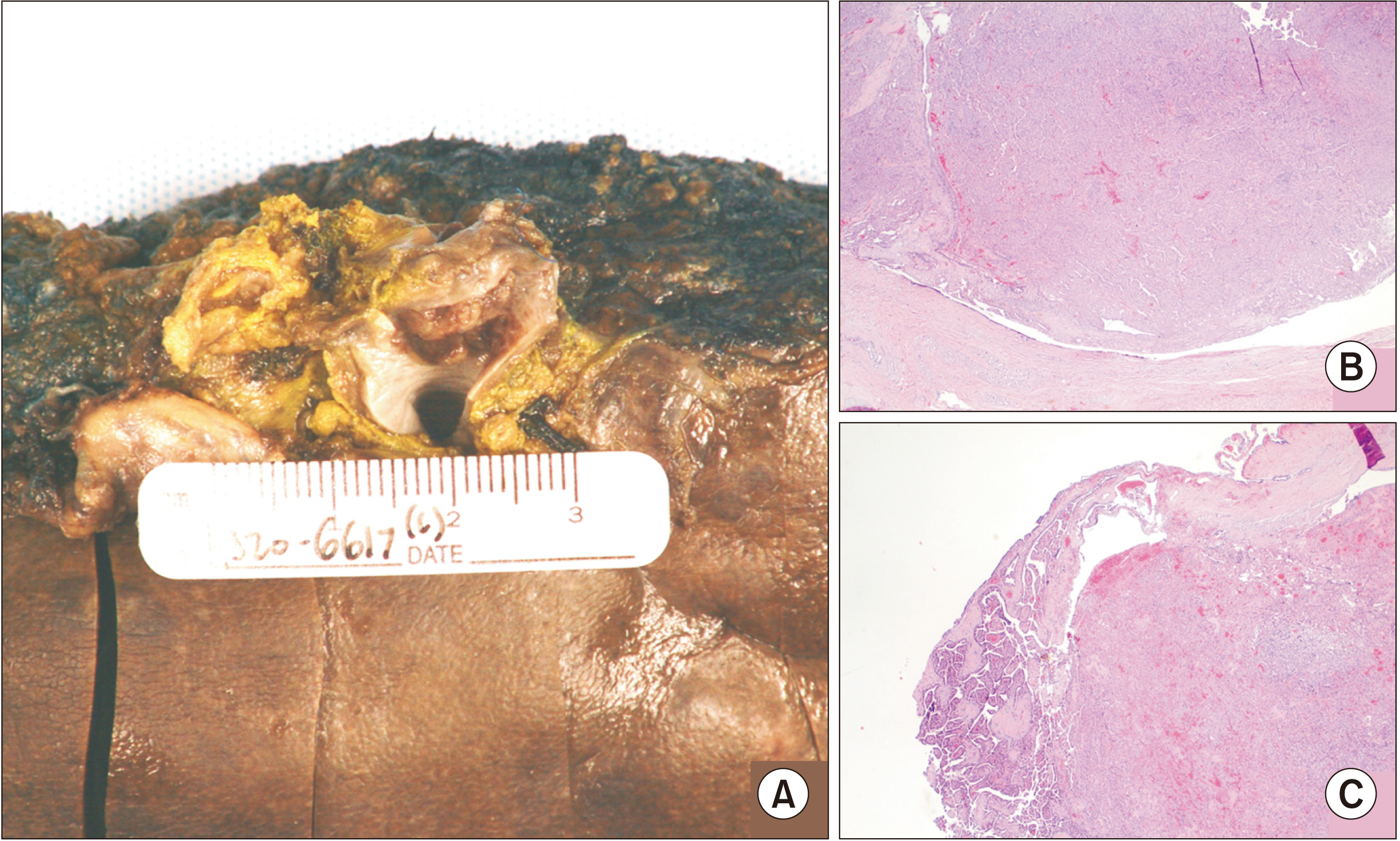
- Intraductal tubulopapillary neoplasms (ITPNs) of the pancreas and biliary tract are rare pre-malignant entities of the biliary tract and pancreas that are difficult to diagnose preoperatively. While there are imaging characteristics that can differentiate these lesions from more common entities like adenocarcinoma or intraductal papillary mucinous neoplasms (IPMN), ITPNs are not always distinctive. Herein we present two cases of ITPN, one of biliary and the other of pancreatic origin, which had a preoperative diagnosis of cholangiocarcinoma and IPMN, respectively. We discuss our findings in these cases, patient presentation and course, review the radiographic and pathologic findings, and propose a more effective approach to the preoperative workup and diagnosis of ITPN based on our review of the contemporary literature.
Figure
Reference
-
1. Kuan LL, Dennison AR, Garcea G. 2020; Intraductal tubulopapillary neoplasm of the pancreas and bile duct: a review. Pancreas. 49:498–502. DOI: 10.1097/MPA.0000000000001518. PMID: 32282762.2. Shahinian HK, Sciadini MF, Springer DJ, Reynolds VH, Lennington WJ. 1992; Tubular adenoma of the main pancreatic duct. Arch Surg. 127:1254–1255. DOI: 10.1001/archsurg.1992.01420100120022. PMID: 1417496.
Article3. Park HJ, Jang KT, Heo JS, Choi YL, Han J, Kim SH. 2010; A potential case of intraductal tubulopapillary neoplasms of the bile duct. Pathol Int. 60:630–635. DOI: 10.1111/j.1440-1827.2010.02572.x. PMID: 20712650.
Article4. Yamaguchi H, Kuboki Y, Hatori T, Yamamoto M, Shiratori K, Kawamura S, et al. 2011; Somatic mutations in PIK3CA and activation of AKT in intraductal tubulopapillary neoplasms of the pancreas. Am J Surg Pathol. 35:1812–1817. DOI: 10.1097/PAS.0b013e31822769a0. PMID: 21945955.
Article5. Schlitter AM, Jang KT, Klöppel G, Saka B, Hong SM, Choi H, et al. 2015; Intraductal tubulopapillary neoplasms of the bile ducts: clinicopathologic, immunohistochemical, and molecular analysis of 20 cases. Mod Pathol. 28:1249–1264. DOI: 10.1038/modpathol.2015.61. PMID: 26111977.
Article6. Visser BC, Yeh BM, Qayyum A, Way LW, McCulloch CE, Coakley FV. 2007; Characterization of cystic pancreatic masses: relative accuracy of CT and MRI. AJR Am J Roentgenol. 189:648–656. DOI: 10.2214/AJR.07.2365. PMID: 17715113.
Article7. Sainani NI, Saokar A, Deshpande V, Fernández-del Castillo C, Hahn P, Sahani DV. 2009; Comparative performance of MDCT and MRI with MR cholangiopancreatography in characterizing small pancreatic cysts. AJR Am J Roentgenol. 193:722–731. DOI: 10.2214/AJR.08.1253. PMID: 19696285.
Article8. Waters JA, Schmidt CM, Pinchot JW, White PB, Cummings OW, Pitt HA, et al. 2008; CT vs MRCP: optimal classification of IPMN type and extent. J Gastrointest Surg. 12:101–109. DOI: 10.1007/s11605-007-0367-9. PMID: 17917784.
Article9. Saeki K, Miyasaka Y, Ohishi Y, Yamamoto T, Matsuda R, Mochidome N, et al. 2018; Intrapancreatic recurrence of intraductal tubulopapillary neoplasm (ITPN) 16 years after the initial surgery for noninvasive ITPN: a case report. Surg Case Rep. 4:96. DOI: 10.1186/s40792-018-0497-1. PMID: 30116990. PMCID: PMC6095932.
Article10. Zhang J, Ren S, Wang J, Ye D, Zhang H, Qiu W, et al. 2019; Imaging findings of intraductal tubulopapillary neoplasm (ITPN) of the pancreas: two case reports and literature review. Medicine (Baltimore). 98:e14426. DOI: 10.1097/MD.0000000000014426. PMID: 30732200. PMCID: PMC6380796.11. Basturk O, Adsay V, Askan G, Dhall D, Zamboni G, Shimizu M, et al. 2017; Intraductal tubulopapillary neoplasm of the pancreas: a clinicopathologic and immunohistochemical analysis of 33 cases. Am J Surg Pathol. 41:313–325. DOI: 10.1097/PAS.0000000000000782. PMID: 27984235. PMCID: PMC5309137.12. Date K, Okabayashi T, Shima Y, Iwata J, Sumiyoshi T, Kozuki A, et al. 2016; Clinicopathological features and surgical outcomes of intraductal tubulopapillary neoplasm of the pancreas: a systematic review. Langenbecks Arch Surg. 401:439–447. DOI: 10.1007/s00423-016-1391-6. PMID: 27001682.
Article13. Kim HJ, Park MS, Chung T, Kim B, Lee JH, Kim JK. 2019; Multimodality imaging studies of intraductal tubulopapillary neoplasms of the pancreas. Diagn Interv Radiol. 25:251–256. DOI: 10.5152/dir.2019.18215. PMID: 31147310. PMCID: PMC6622442.
Article14. Wu CH, Yeh YC, Tsuei YC, Huang LK, Lin CI, Liu CA, et al. 2017; Comparative radiological pathological study of biliary intraductal tubulopapillary neoplasm and biliary intraductal papillary mucinous neoplasm. Abdom Radiol (NY). 42:2460–2469. DOI: 10.1007/s00261-017-1167-7. PMID: 28470400.
Article15. Kim H, Ro JY. 2018; Intraductal tubulopapillary neoplasm of the pancreas: an overview. Arch Pathol Lab Med. 142:420–423. DOI: 10.5858/arpa.2016-0405-RSR2. PMID: 29494224.
Article16. Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. 1990; Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 14:535–543. discussion 544DOI: 10.1007/BF01658686. PMID: 2166381.
Article17. Mizumoto R, Kawarada Y, Suzuki H. 1986; Surgical treatment of hilar carcinoma of the bile duct. Surg Gynecol Obstet. 162:153–158. PMID: 3945893.18. Hwang S. 2021; Standard and modified techniques for parenchyma-preserving hepatectomy focused on segments I+IV resection in patients with perihilar cholangiocarcinoma. Ann Hepatobiliary Pancreat Surg. 25:112–121. DOI: 10.14701/ahbps.2021.25.1.112. PMID: 33649263. PMCID: PMC7952662.
Article19. Yang M, Li WW, Chen JH, Cui MH, Liu JL. 2021; The value of caudate lobectomy in hilar cholangiocarcinoma treatment: a meta-analysis. Medicine (Baltimore). 100:e24727. DOI: 10.1097/MD.0000000000024727. PMID: 33607815. PMCID: PMC7899860.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Pancreatitis Associated with Intraductal Tubulopapillary Neoplasm of the Pancreas
- Surgical Indications and Postsurgical Follow-up Strategy for Pancreatic Cystic Neoplasm
- Intraductal Papillary Mucinous Neoplasm of Pancreas with High-Risk Stigmata or Worrisome Features: What do You Do? Physician’s View
- Intrahepatic and extrahepatic intraductal papillary neoplasms of bile duct
- A Case of Direct Peroral Cholangioscopy-Guided Intraductal Radiofrequency Ablation for Malignancy Biliary Obstruction via Choledochoduodenostomy Orifice