Arch Hand Microsurg.
2021 Dec;26(4):265-269. 10.12790/ahm.21.0126.
Malignant Nodular Hidradenoma of the Fingertip: A Case Report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae General Hospital, Gwangmyeong, Korea
- 2Department of Pathology, Gwangmyeong Sungae General Hospital, Gwangmyeong, Korea
- 3Department of Plastic and Reconstructive Surgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2522624
- DOI: http://doi.org/10.12790/ahm.21.0126
Abstract
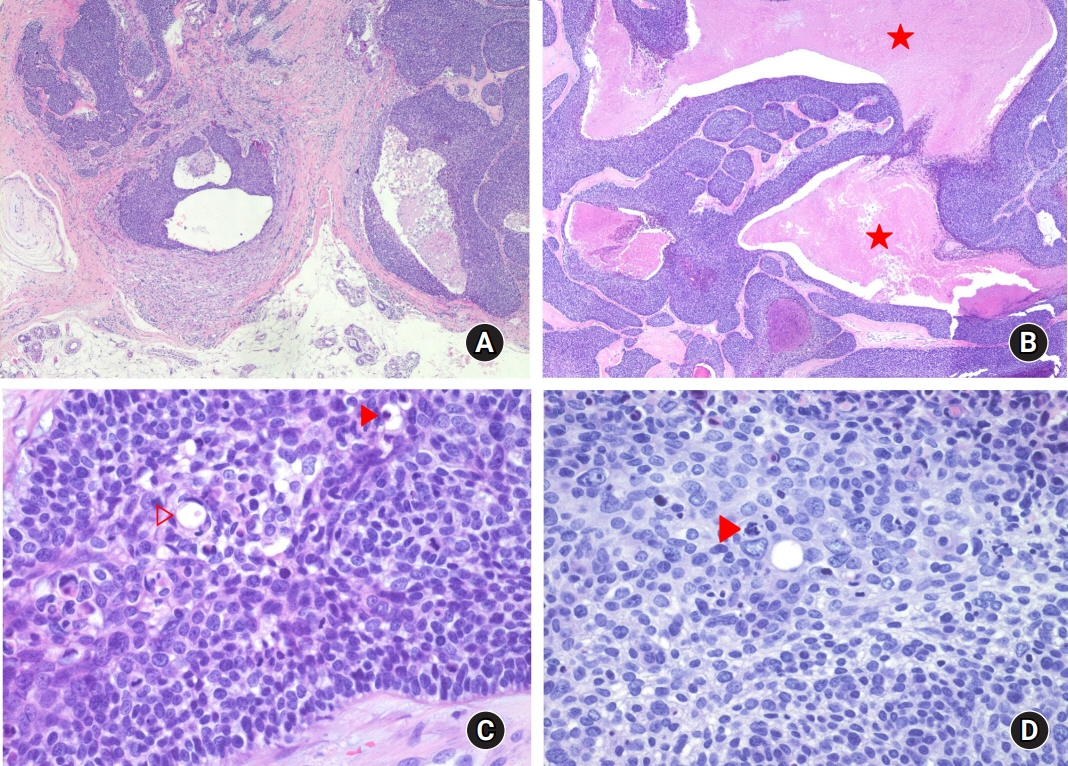
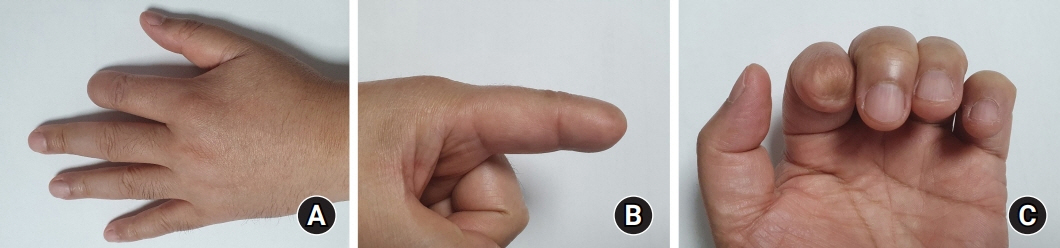
- Malignant nodular hidradenoma (MNH) is an infrequent, highly malignant tumor derived from eccrine sweat glands. MNH usually occurs on the scalp, trunk, and proximal extremities, and rarely on the hand. A 55-year-old male patient visited clinics with a gradually enlarging painless mass at fingertip. It begins a year ago. Recently, it has grown rapidly and starts ulceration, and bleeding over the past 3 weeks. According to the biopsy report, it has focal necrosis, atypia, atypical mitoses, and nuclear pleomorphism suggested that the mass was MNH. After histological diagnosis, tiny bone erosion was observed in the re-read radiographic finding. For the oncologic evaluation, the patient was transferred to the cancer center. Radical amputation was performed to the residual tumor that might remain based on re-reading of radiographs. MNH of the finger is especially difficult to the diagnosis given its rarity and variable histology. When ulcerative skin lesion and radiographic bone erosion are observed, one should suspect malignancy and makes out a proper therapeutic plan after histologic biopsy.
Keyword
Figure
Reference
-
1. Souvatzidis P, Sbano P, Mandato F, Fimiani M, Castelli A. Malignant nodular hidradenoma of the skin: report of seven cases. J Eur Acad Dermatol Venereol. 2008; 22:549–54.
Article2. Chang CH, Chang KP, Huang SH, et al. Hidradenocarcinoma of the fingertip: a case report and literature review. Dermatol Surg. 2011; 37:704–8.
Article3. Nazerali RS, Tan C, Fung MA, Chen SL, Wong MS. Hidradenocarcinoma of the finger. Ann Plast Surg. 2013; 70:423–6.
Article4. Kasbekar PU, Shailaja PJ. Case study of a rare case of nodular hidradenoma of the finger. Int J Sci Res. 2013; 3:1–4.5. Lee JH, Cho SI, Do NY, Dong KW, et al. A case of giant malignant clear cell hidradenoma. Korean J Otolaryngol-Head Neck Surg. 2005; 48:1305–8.6. Stout AP, Cooley SG. Carcinoma of sweat glands. Cancer. 1951; 4:521–36.
Article7. Choi BS, Kim YJ, Kim JY, Jo HJ. Nodular hidradenoma on the fourth finger. J Korean Soc Surg Hand. 2013; 18:143–6.
Article8. Dhawan SS, Nanda VS, Grekin S, Rabinovitz HS. Apocrine adenocarcinoma: case report and review of the literature. J Dermatol Surg Oncol. 1990; 16:468–70.
Article9. Robson A, Greene J, Ansari N, et al. Eccrine porocarcinoma (malignant eccrine poroma): a clinicopathologic study of 69 cases. Am J Surg Pathol. 2001; 25:710–20.