Korean J Women Health Nurs.
2021 Sep;27(3):180-195. 10.4069/kjwhn.2021.09.17.
Effects of nonpharmacological interventions on the psychological health of high-risk pregnant women: a systematic review and meta-analysis
- Affiliations
-
- 1College of Nursing, Chungnam National University, Daejeon, Korea
- KMID: 2521514
- DOI: http://doi.org/10.4069/kjwhn.2021.09.17
Abstract
- Purpose
This study aimed to summarize the current evidence on the effects of nonpharmacological interventions on psychological health outcomes for women with high-risk pregnancies due to conditions such as preeclampsia, gestational diabetes, or preterm labor.
Methods
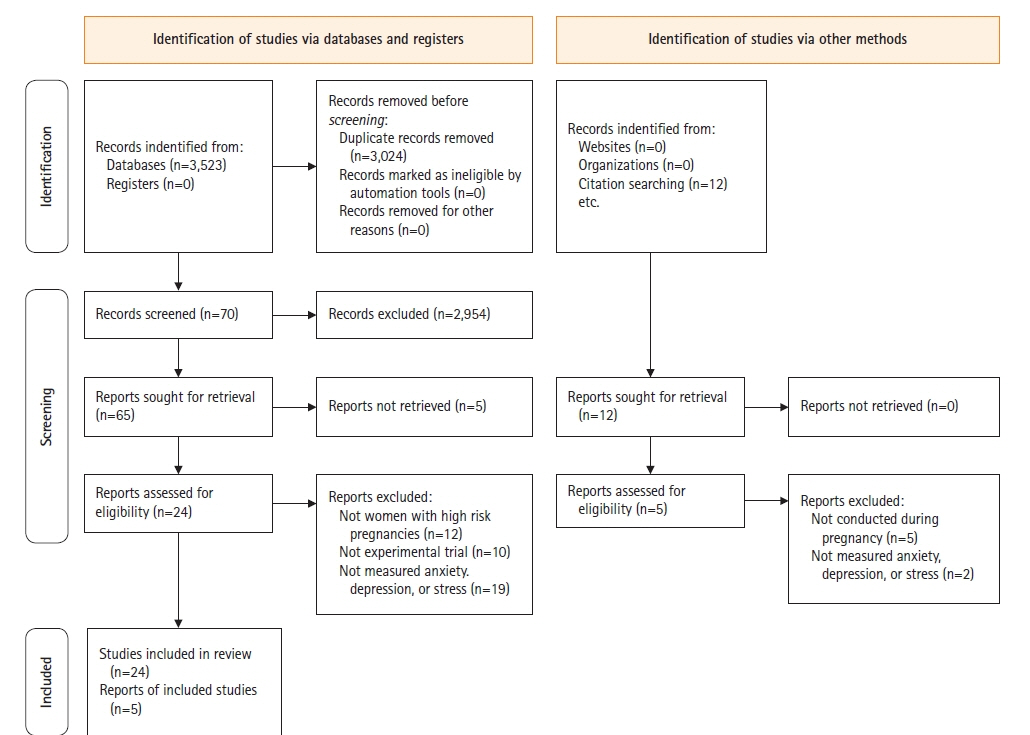
The following databases were searched from January 2000 to December 2020: PubMed, Ovid Embase, CINAHL, Web of Science, DBpia, RISS, and KISS. Two investigators independently reviewed and selected articles according to the inclusion/exclusion criteria. RoB 2 and the ROBINS-I checklist were used to evaluate study quality.
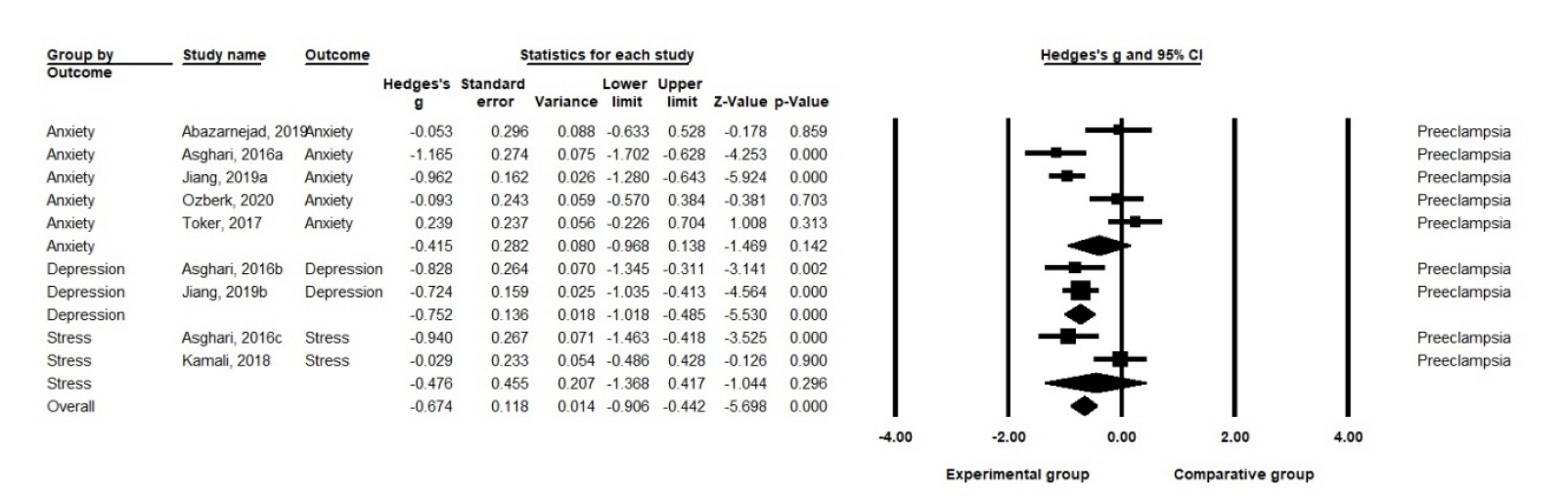
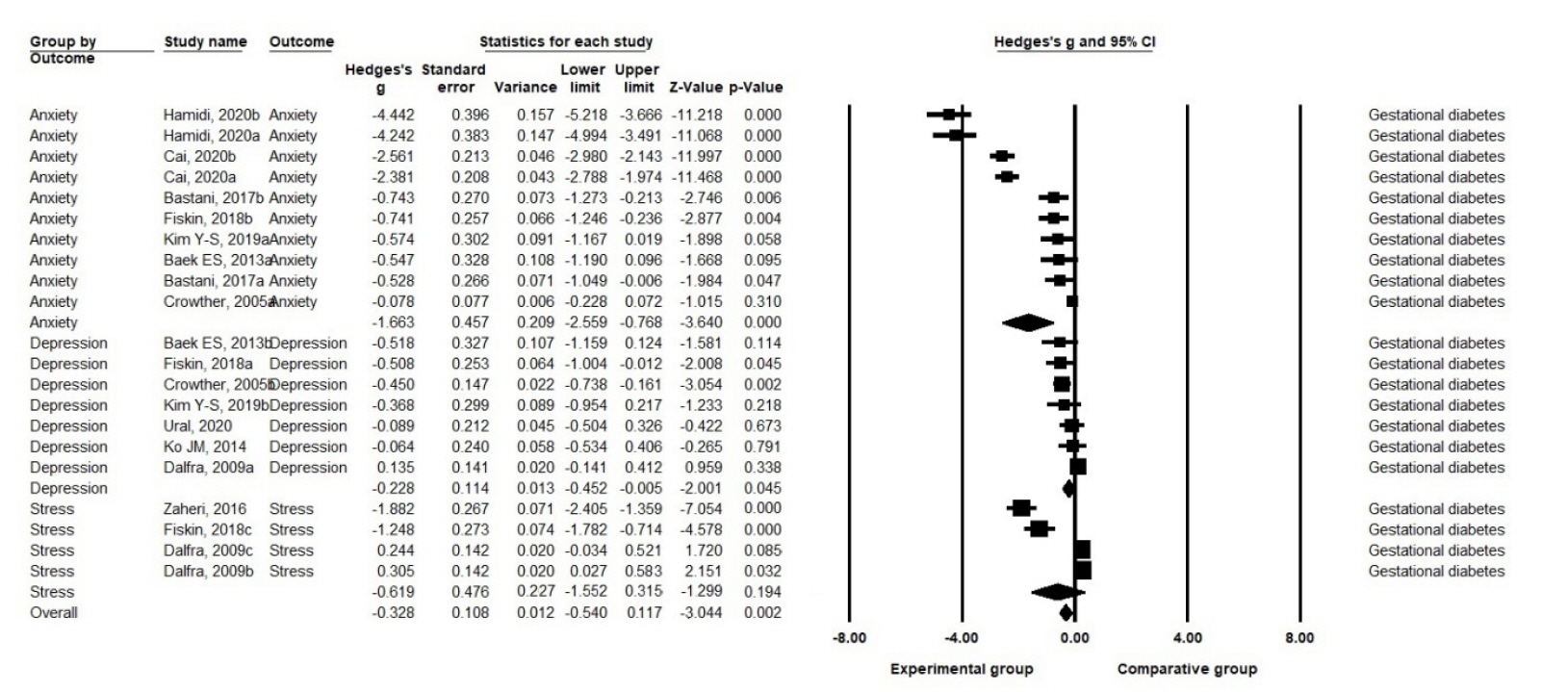
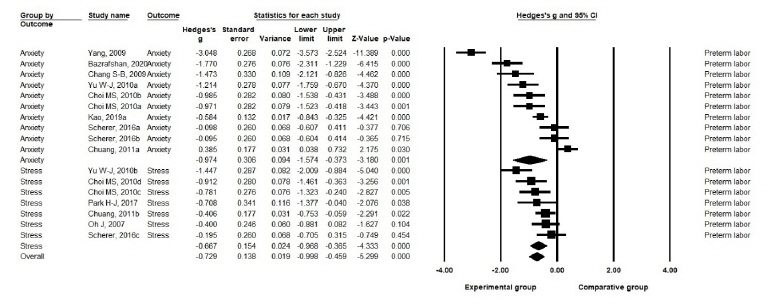
Results
Twenty-nine studies with a combined total of 1,806 pregnant women were included in the systematic review and meta-analysis. Psychological health improvements were found in women with preeclampsia (Hedges’ g=–0.67; 95% confidence interval [CI], –0.91 to –0.44), gestational diabetes (Hedges’ g=–0.38; 95% CI, –0.54 to –0.12), and preterm labor (Hedges’ g=–0.73; 95% CI, –1.00 to –0.46). The funnel plot was slightly asymmetrical, but the fail-safe N value and the trim-and-fill method showed no publication bias.
Conclusion
Nonpharmacological interventions for women with high-risk pregnancies due to conditions such as preeclampsia, gestational diabetes, and preterm labor can improve psychological parameters such as anxiety, stress, and depression. Nurses can play a pivotal role in the nursing management of pregnant women with high-risk conditions and apply various types of nonpharmacological interventions to meet their needs in uncertain and anxious times during pregnancy.
Keyword
Figure
Reference
-
References
1. Hwang JY. Reclassification of high-risk pregnancy for maternal-fetal healthcare providers. J Korean Soc Matern Child Health. 2020; 24(2):65–74. https://doi.org/10.21896/jksmch.2020.24.2.65.
Article2. Ahn TG, Kim T, Kim Y, Hwang JY. The current state of maternity care and suggestions for improvement in the management of high-risk pregnancies in South Korea. J Korean Soc Matern Child Health. 2018; 22(3):134–141. https://doi.org/10.21896/jksmch.2018.22.3.134.
Article3. Isaacs NZ, Andipatin MG. A systematic review regarding women’s emotional and psychological experiences of high-risk pregnancies. BMC Psychol. 2020; 8(1):45. https://doi.org/10.1186/s40359-020-00410-8.
Article4. Palma E, Armijo I, Cifuentes J, Ambiado S, Rochet P, Díaz B, et al. Hospitalisation in high-risk pregnancy patients: is prenatal attachment affected? J Reprod Infant Psychol. 2021; 39(1):30–42. https://doi.org/10.1080/02646838.2020.1740661.
Article5. Ko SY, Bae JG, Jung SW. A comparative study on the anxiety, depression, and maternal-fetal attachment of high-risk pregnant women and normal pregnant women. J Korean Soc Biol Ther Psychiatry. 2019; 25(2):117–126. https://doi.org/10.22802/jksbtp.2019.25.2.117.
Article6. Jung SH, Bae JG, Jung SW, Kim MK, Kim HC, Kim JB. Effects of the temperament and character on depression, anxiety, and maternal-fetal attachment in high-risk pregnant women. Anxiety Mood. 2018; 14(2):106–11. https://doi.org/10.24986/anxmod.2018.14.2.007.
Article7. Fairbrother N, Young AH, Zhang A, Janssen P, Antony MM. The prevalence and incidence of perinatal anxiety disorders among women experiencing a medically complicated pregnancy. Arch Womens Ment Health. 2017; 20(2):311–319. https://doi.org/10.1007/s00737-016-0704-7.
Article8. Tsakiridis I, Bousi V, Dagklis T, Sardeli C, Nikolopoulou V, Papazisis G. Epidemiology of antenatal depression among women with high-risk pregnancies due to obstetric complications: a scoping review. Arch Gynecol Obstet. 2019; 300(4):849–859. https://doi.org/10.1007/s00404-019-05270-1.
Article9. Kim H, Park H. Health-care needs of high-risk pregnant women hospitalized in maternal-fetal Intensive care units: a mixed-methods design. Korean J Women Health Nurs. 2018; 24(2):196–208. https://doi.org/10.4069/kjwhn.2018.24.2.196.
Article10. Ali AA, Sayed AK, El Sherif L, Loutfi GO, Ahmed AM, Mohamed HB, et al. Systematic review and meta-analysis of randomized controlled trials of atosiban versus nifedipine for inhibition of preterm labor. Int J Gynaecol Obstet. 2019; 145(2):139–148. https://doi.org/10.1002/ijgo.12793.
Article11. Martis R, Crowther CA, Shepherd E, Alsweiler J, Downie MR, Brown J. Treatments for women with gestational diabetes mellitus: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. 2018; 8(8):CD012327. https://doi.org/10.1002/14651858.CD012327.pub2.
Article12. Smith CA, Tuson A, Thornton C, Dahlen HG. The safety and effectiveness of mind body interventions for women with pregnancy induced hypertension and or preeclampsia: a systematic review and meta-analysis. Complement Ther Med. 2020; 52:102469. https://doi.org/10.1016/j.ctim.2020.102469.
Article13. Park SJ, Lee J. The effects of health care programs for gestational diabetes mellitus in South Korea: a systematic review. Korean J Women Health Nurs. 2020; 26(4):274–284. https://doi.org/10.4069/kjwhn.2020.10.28.
Article14. Brown J, Alwan NA, West J, Brown S, McKinlay CJ, Farrar D, et al. Lifestyle interventions for the treatment of women with gestational diabetes. Cochrane Database Syst Rev. 2017; 5(5):CD011970. https://doi.org/10.1002/14651858.CD011970.pub2.
Article15. Berghella V, Palacio M, Ness A, Alfirevic Z, Nicolaides KH, Saccone G. Cervical length screening for prevention of preterm birth in singleton pregnancy with threatened preterm labor: systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet Gynecol. 2017; 49(3):322–329. https://doi.org/10.1002/uog.17388.
Article16. Medley N, Poljak B, Mammarella S, Alfirevic Z. Clinical guidelines for prevention and management of preterm birth: a systematic review. BJOG. 2018; 125(11):1361–1369. https://doi.org/10.1111/1471-0528.15173.
Article17. Kim J, Chung C. Effects of nursing intervention programs for women with gestational diabetes: a systematic review of randomized controlled trials. Korean J Women Health Nurs. 2021; 27(1):14–26. https://doi.org/10.4069/kjwhn.2021.03.02.
Article18. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71. https://doi.org/10.1136/bmj.n71.
Article19. Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Chapter 8: Assessing risk of bias in a randomized trial. 2021. Cochrane Handbook for Systematic Reviews of Interventions version 62 (updated February 2021) [Internet]. London: Cochrane;2021. [cited Year Mon date]. Available from: www.training.cochrane.org/handbook.20. Sterne JA, Hernán MA, McAleenan A, Reeves BC, JPT H. Chapter 25: Assessing risk of bias in a non-randomized study [Internet]. Cochrane Handbook for Systematic Reviews of Interventions version 60 (updated July 2019). London: Cochrane;2019. [cited Year Mon date]. Available from: www.training.cochrane.org/handbook.21. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557.
Article22. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629.
Article23. Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull. 1979; 86(3):638–641. https://doi.org/10.1037/0033-2909.86.3.638.
Article24. Duval S. The trim and fill method. Publication bias in meta-analysis: prevention, assessment and adjustments. 2005; 127–144. https://doi.org/10.1002/0470870168.ch8.
Article25. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000; 56(2):455–463. https://doi.org/10.1111/j.0006-341x.2000.00455.x.
Article26. Yang M, Li L, Zhu H, Alexander IM, Liu S, Zhou W, et al. Music therapy to relieve anxiety in pregnant women on bedrest: a randomized, controlled trial. MCN Am J Matern Child Nurs. 2009; 34(5):316–323. https://doi.org/10.1097/01.NMC.0000360425.52228.95.
Article27. Bastani F. Effect of acupressure on maternal anxiety in women with gestational diabetes mellitus: a randomized clinical trial. Clin Nurs Res. 2016; 25(3):325–341. https://doi.org/10.1177/1054773815579344.
Article28. Abazarnejad T, Ahmadi A, Nouhi E, Mirzaee M, Atghai M. Effectiveness of psycho-educational counseling on anxiety in preeclampsia. Trends Psychiatry Psychother. 2019; 41(3):276–282. https://doi.org/10.1590/2237-6089-2017-0134.
Article29. Bazrafshan S, Kheirkhah M, Inanlou M, Rasouli M. Controlling the anxiety in Iranian pregnant women at risk of preterm labor by undergoing the counseling group intervention. J Family Med Prim Care. 2020; 9(8):4016–4025. https://doi.org/10.4103/jfmpc.jfmpc_1227_19.
Article30. Chuang LL, Lin LC, Cheng PJ, Chen CH, Wu SC, Chang CL. The effectiveness of a relaxation training program for women with preterm labour on pregnancy outcomes: a controlled clinical trial. Int J Nurs Stud. 2012; 49(3):257–264. https://doi.org/10.1016/j.ijnurstu.2011.09.007.
Article31. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005; 352(24):2477–2486. https://doi.org/10.1056/NEJMoa042973.
Article32. Fiskin G, Sahin NH. Effect of diaphragmatic breathing exercise on psychological parameters in gestational diabetes: a randomised controlled trial. Eur J Integr Med. 2018; 23:505–6. https://doi.org/10.1016/j.eujim.2018.09.006.
Article33. Hamidi F, Javadnoori M, Hoss Einifard SM, Nikbakht R. The effectiveness of mindfulness-based training on anxiety in pregnant women with gestational diabetes. Fam Med Prim Care Rev. 2020; 22(4):279–283. https://doi.org/10.5114/fmpcr.2020.100430.
Article34. Jiang J, Wang F. Comprehensive nursing on postpartum complications and negative emotions of patients with pregnancy induced hypertension syndrome. Int J Clin Exp Med. 2019; 12(9):11982–11989.35. Kamali Z, Tafazoli M, Ebrahimi M, Hosseini M, Saki A, Fayyazi-Bordbar MR, et al. Effect of spiritual care education on postpartum stress disorder in women with preeclampsia. J Educ Health Promot. 2018; 7:73. https://doi.org/10.4103/jehp.jehp_170_17.
Article36. Kao MH, Hsu PF, Tien SF, Chen CP. Effects of support interventions in women hospitalized with preterm labor. Clin Nurs Res. 2019; 28(6):726–743. https://doi.org/10.1177/1054773817744323.
Article37. Özberk H, Mete S, Bektaş M. Effects of relaxation-focused nursing care in women in preterm labor. Biol Res Nurs. 2021; 23(2):160–170. https://doi.org/10.1177/1099800420941253.
Article38. Scherer S, Alder J, Gaab J, Berger T, Ihde K, Urech C. Patient satisfaction and psychological well-being after internet-based cognitive behavioral stress management (IB-CBSM) for women with preterm labor: a randomized controlled trial. J Psychosom Res. 2016; 80:37–43. https://doi.org/10.1016/j.jpsychores.2015.10.011.
Article39. Toker E, Kömürcü N. Effect of Turkish classical music on prenatal anxiety and satisfaction: a randomized controlled trial in pregnant women with pre-eclampsia. Complement Ther Med. 2017; 30:1–9. https://doi.org/10.1016/j.ctim.2016.11.005.
Article40. Ural A, Kizilkaya Beji N. The effect of health-promoting lifestyle education program provided to women with gestational diabetes mellitus on maternal and neonatal health: a randomized controlled trial. Psychol Health Med. 2021; 26(6):657–670. https://doi.org/10.1080/13548506.2020.1856390.
Article41. Zaheri H, Najar S, Abbaspoor Z. Effectiveness of cognitive-behavioral stress management on psychological stress and glycemic control in gestational diabetes: a randomized controlled trial. J Matern Fetal Neonatal Med. 2017; 30(11):1378–1382. https://doi.org/10.1080/14767058.2016.1214699.
Article42. Zhao Y, Munro-Kramer ML, Shi S, Wang J, Luo J. A randomized controlled trial: effects of a prenatal depression intervention on perinatal outcomes among Chinese high-risk pregnant women with medically defined complications. Arch Womens Ment Health. 2017; 20(2):333–344. https://doi.org/10.1007/s00737-016-0712-7.
Article43. Kim HJ, Chun N. Effects of a supportive program on uncertainty, anxiety, and maternal-fetal attachment in women with high-risk pregnancy. Korean J Women Health Nurs. 2020; 26(2):180–190. https://doi.org/10.4069/kjwhn.2020.06.17.
Article44. Park HJ, Sung MH. Effects of music therapy on stress of preterm labor and uterine contraction in pregnant women with preterm labor. Korean J Women Health Nurs. 2017; 23(2):109–116. https://doi.org/10.4069/kjwhn.2017.23.2.109.
Article45. Oh J. Effects of providing information on stress and maternal role confidence of women with preterm labor. Korean Parent-Child Health J. 2007; 10(2):99–109.46. Chang SB, Kim HS, Ko YH, Bae CH, An SE. Effects of abdominal breathing on anxiety, blood pressure, peripheral skin temperature and saturation oxygen of pregnant women in preterm labor. Korean J Women Health Nurs. 2009; 15(1):32–42. https://doi.org/10.4069/kjwhn.2009.15.1.32.
Article47. Asghari E, Faramarzi M, Mohammmadi AK. The effect of cognitive behavioural therapy on anxiety, depression and stress in women with preeclampsia. J Clin Diagn Res. 2016; 10(11):QC04–QC07. https://doi.org/10.7860/JCDR/2016/21245.8879.
Article48. Baek ES, Park HJ. Effects of a case management program on self-efficacy, depression and anxiety in pregnant women with gestational diabetes mellitus. Korean J Women Health Nurs. 2013; 19(2):88–98. https://doi.org/10.4069/kjwhn.2013.19.2.88.
Article49. Cai Q, Xiao C, Zhou Y, Chen J, Du P, Wu Y, et al. Effect of comprehensive nursing on blood glucose level, unhealthy emotion, and pregnancy outcome of patients with gestational diabetes mellitus. Int J Clin Exp Med. 2020; 13(10):8158–8166.50. Choi MS, Park YJ. The effects of relaxation therapy on anxiety and stress of pregnant women with preterm labor. Korean J Women Health Nurs. 2010; 16(4):336–347. https://doi.org/10.4069/kjwhn.2010.16.4.336.
Article51. Dalfrà MG, Nicolucci A, Lapolla A; TISG. The effect of telemedicine on outcome and quality of life in pregnant women with diabetes. J Telemed Telecare. 2009; 15(5):238–242. https://doi.org/10.1258/jtt.2009.081213.
Article52. Kim YS, Kim HS, Kim YL. Effects of a web-based self-management program on the behavior and blood glucose levels of women with gestational diabetes mellitus. Telemed J E Health. 2019; 25(5):407–414. https://doi.org/10.1089/tmj.2017.0332.
Article53. Ko JM, Lee JK. Effects of a coaching program on comprehensive lifestyle modification for women with gestational diabetes mellitus. J Korean Acad Nurs. 2014; 44(6):672–681. https://doi.org/10.4040/jkan.2014.44.6.672.
Article54. Yu WJ, Song JE. Effects of abdominal breathing on state anxiety, stress, and tocolytic dosage for pregnant women in preterm labor. J Korean Acad Nurs. 2010; 40(3):442–452. https://doi.org/10.4040/jkan.2010.40.3.442.
Article55. Choi Y. Active running medical health support project in Ganghwa-gun [Internet]. Seoul: Newsworks;2021. [cited 2021 Sep 16]. Available from: http://www.newsworks.co.kr/news/articleView.html?idxno=564657.56. Kim Y. Running a contacless prenatal education class for pregnant women in Hadong-gun [Internet]. Seoul: NEWSIS;2021. [cited 2021 Sep 16]. Available from: https://newsis.com/view/?id=NISX20210824_0001557961&cID=10812&pID=10800#.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Systematic Review of Nonpharmacological Interventions for Moderate to Severe Dementia: A Study Protocol for a Systematic Review and Meta-Analysis
- Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis
- Fatigue relief by aromatherapy use in prenatal and postnatal women: a systematic review and meta-analysis
- The effects of health care programs for gestational diabetes mellitus in South Korea: a systematic review
- The Effects of Advance Care Planning on Decision Conflict and Psychological Distress: A Systematic Review and Meta-Analysis of Randomized Controlled Trials