Anat Cell Biol.
2021 Sep;54(3):361-374. 10.5115/acb.21.034.
Therapeutic efficiency of adipose-derived mesenchymal stem cells in healing of experimentally induced gastric ulcers in rats
- Affiliations
-
- 1Histology and Cell Biology Department, Faculty of Medicine, Assiut University, Assiut, Egypt
- 2Histology and Cell Biology Department, Sphinx University, Assiut, Egypt
- KMID: 2521049
- DOI: http://doi.org/10.5115/acb.21.034
Abstract
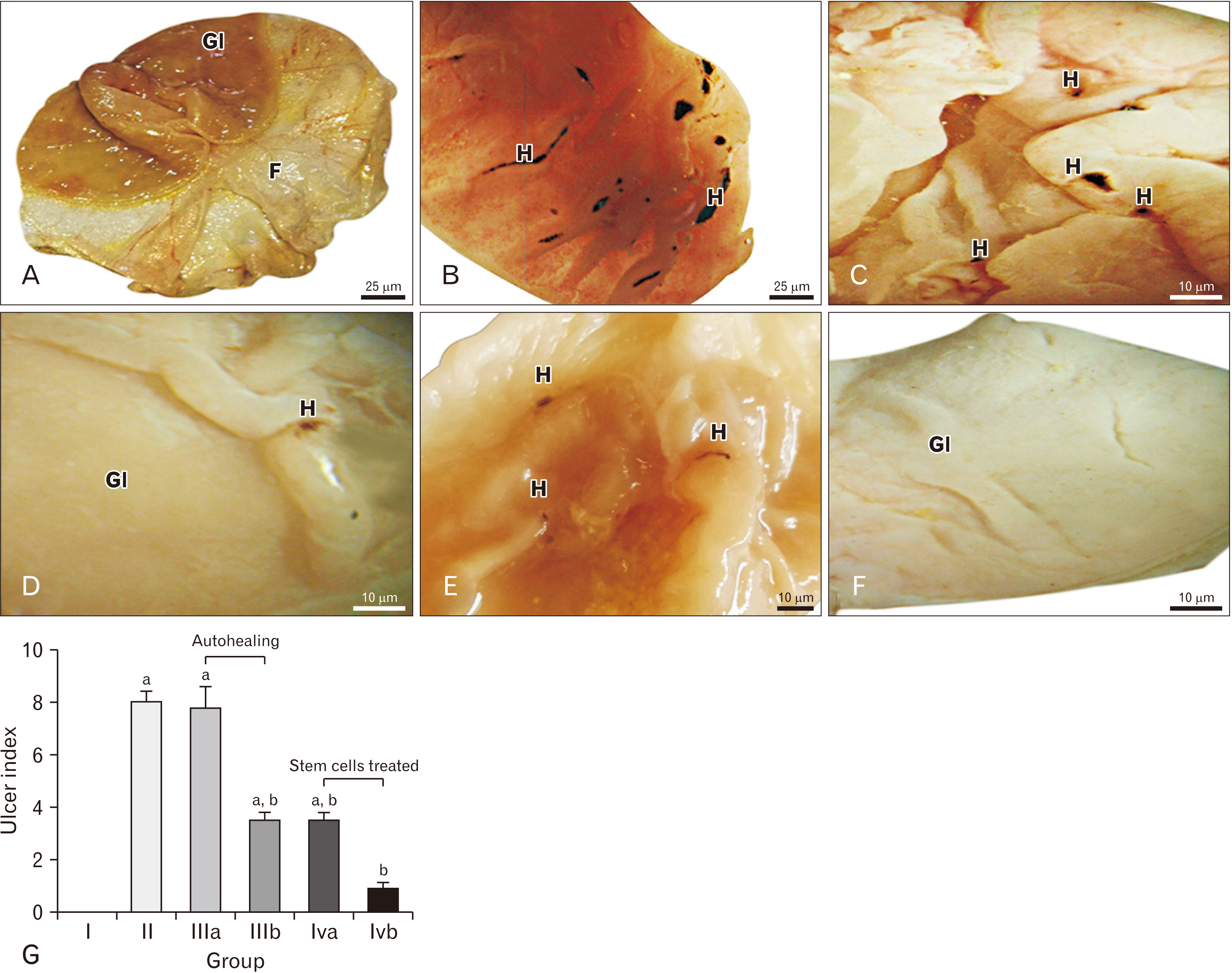
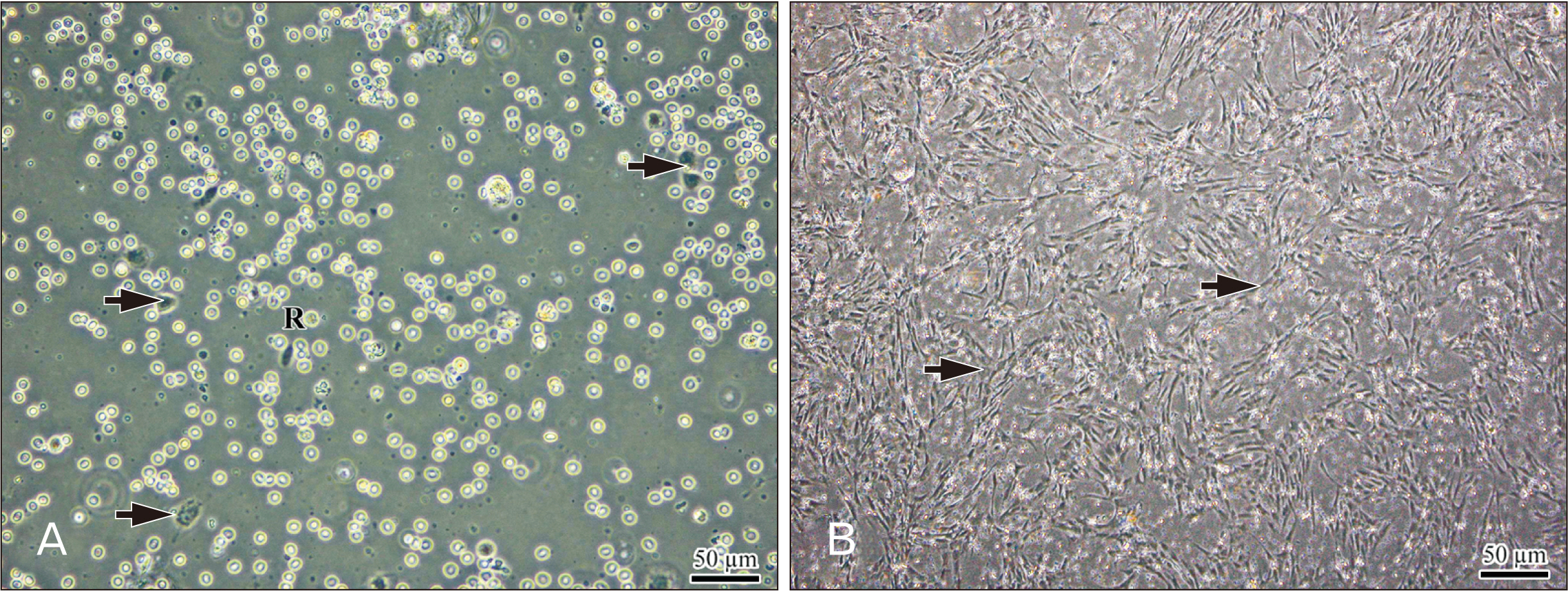
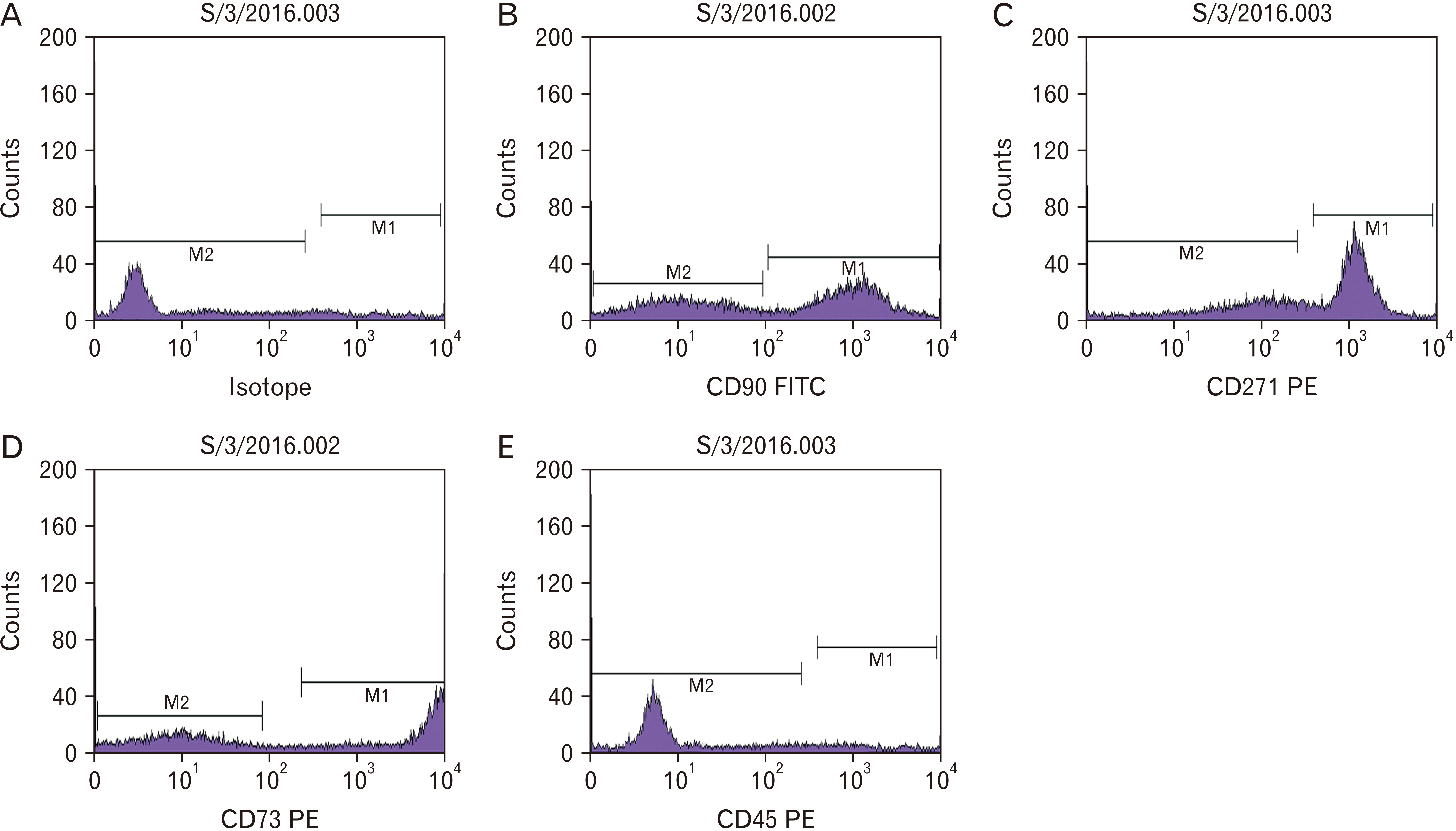
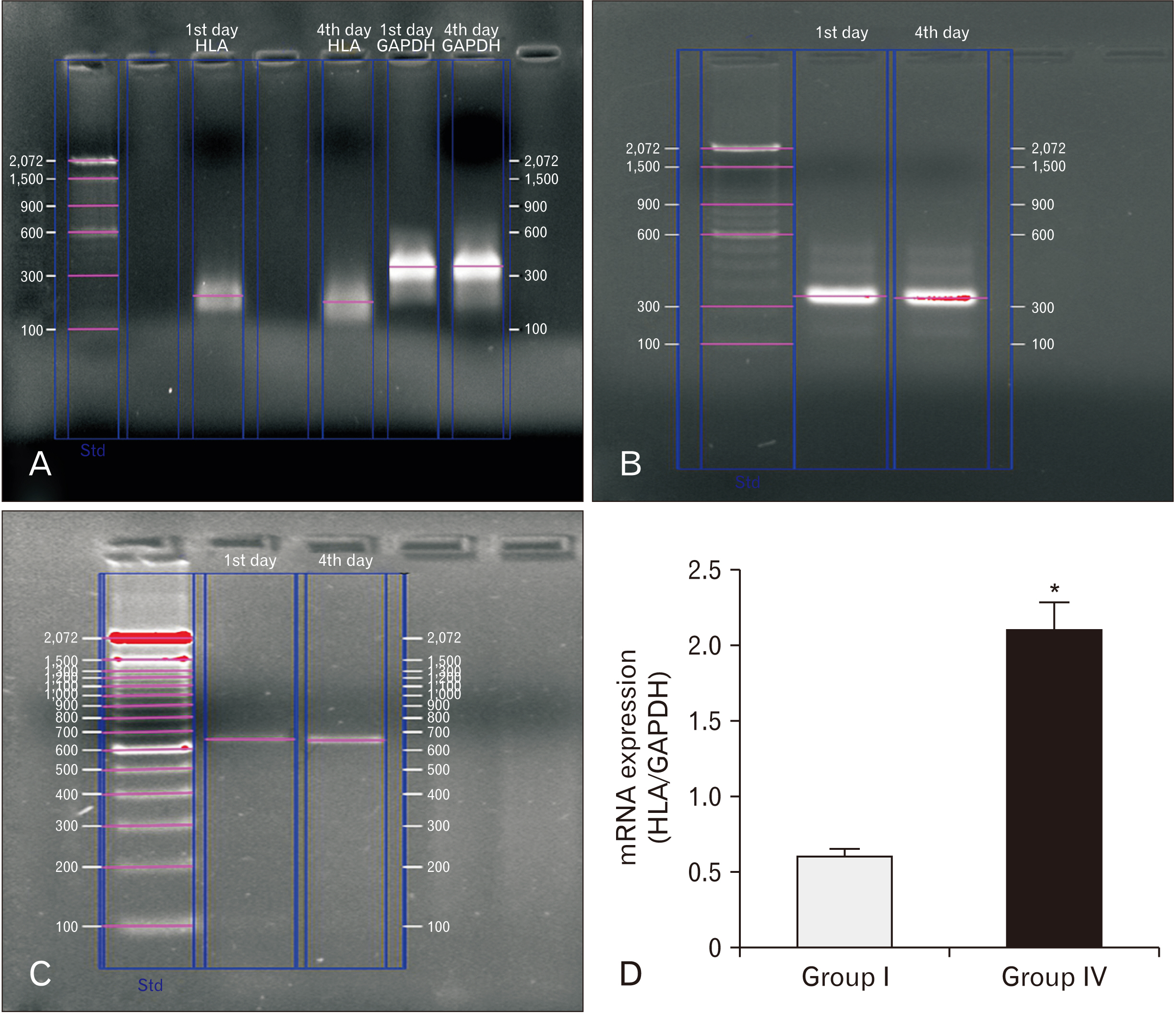
- Gastric (peptic) ulcer is a major gastrointestinal disorder with high morbidity and mortality. While several drugs have been used to treat gastric ulcers, such as proton pump inhibitor-based triple therapy for Helicobacter pylori eradication, but hey result in adverse side effects. Therefore, development of new alternative therapies is desirable. Many recent studies have shown that mesenchymal stem cells (MSCs) might have an enhancing effect on the ulcerated gastric mucosa. The aim of this study is to evaluate the efficacy of MSCs in the treatment of indomethacin-induced gastric ulcer, and to compare it with the normal ulcer autohealing. This work was performed on 36 adult male albino rats, divided into four groups: Group I (control group), Group II (ulcer group), Group III (autohealing group), and Group IV (stem cells-treated group). The histological changes of gastric mucosa were examined in sections stained with H&E using light microscope for expression of vascular endothelial growth factors (VEGF) and proliferating cell nuclear antigen (PCNA) in immunohistochemical stained sections using image analyzer. The results from MSCs-treated group revealed restoration of the normal architecture of the gastric mucosa with comparison to the autohealing group which showed excessive granulation tissue and heavy cellular infiltration with disorganized architecture of the fundic mucosa. Immunohistochemical examination showed strong expression of both VEGF and PCNA in the MSCs-treated group. So it was concluded that MSCs accelerate gastric ulcer healing when injected intraperitoneally, compared to autohealing process which showed delayed healing.
Keyword
Figure
Reference
-
References
1. Abd-Elmenm S, Greish S, Atwa M, Fathelbab M. 2016; Evaluation of the role of adipose-derived stem cells in the healing of indomethacin-induced gastric ulceration in rats. J Cell Sci Ther. 7:246. DOI: 10.4172/2157-7013.1000246.
Article2. Chaturvedi A, Kumar MM, Bhawani G, Chaturvedi H, Kumar M, Goel RK. 2007; Effect of ethanolic extract of Eugenia jambolana seeds on gastric ulceration and secretion in rats. Indian J Physiol Pharmacol. 51:131–40. PMID: 18175656.3. Chang Q, Yan L, Wang CZ, Zhang WH, Hu YZ, Wu BY. 2012; In vivo transplantation of bone marrow mesenchymal stem cells accelerates repair of injured gastric mucosa in rats. Chin Med J (Engl). 125:1169–74. PMID: 22613549.4. Jones MK, Wang H, Peskar BM, Levin E, Itani RM, Sarfeh IJ, Tarnawski AS. 1999; Inhibition of angiogenesis by nonsteroidal anti-inflammatory drugs: insight into mechanisms and implications for cancer growth and ulcer healing. Nat Med. 5:1418–23. DOI: 10.1038/70995. PMID: 10581086.
Article5. Najm WI. 2011; Peptic ulcer disease. Prim Care. 38:383–94. viiDOI: 10.1016/j.pop.2011.05.001. PMID: 21872087.
Article6. Sonnenberg A. 1985; Geographic and temporal variations in the occurrence of peptic ulcer disease. Scand J Gastroenterol Suppl. 110:11–24. DOI: 10.3109/00365528509095826. PMID: 2862697.
Article7. Badhani S, Jasrotia N, Sharma I, Parashar B, Gupta R. 2012; A review on some Indian medicinal plants for antiulcer activity. J Sci Res Pharm. 1:6–9.8. Abraham NS, El-Serag HB, Johnson ML, Hartman C, Richardson P, Ray WA, Smalley W. 2005; National adherence to evidence-based guidelines for the prescription of nonsteroidal anti-inflammatory drugs. Gastroenterology. 129:1171–8. DOI: 10.1053/j.gastro.2005.08.003. PMID: 16230071.
Article9. Atuma C, Strugala V, Allen A, Holm L. 2001; The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver Physiol. 280:G922–9. DOI: 10.1152/ajpgi.2001.280.5.G922. PMID: 11292601.10. Lichtenberger LM. 1999; Gastroduodenal mucosal defense. Curr Opin Gastroenterol. 15:463–72. DOI: 10.1097/00001574-199911000-00003. PMID: 17023992. PMCID: PMC4711914.
Article11. Modlin IM, Kidd M, Lye KD, Wright NA. 2003; Gastric stem cells: an update. Keio J Med. 52:134–7. DOI: 10.2302/kjm.52.134. PMID: 12862366.
Article12. Yang H, Ara A, Magilnick N, Xia M, Ramani K, Chen H, Lee TD, Mato JM, Lu SC. 2008; Expression pattern, regulation, and functions of methionine adenosyltransferase 2beta splicing variants in hepatoma cells. Gastroenterology. 134:281–91. DOI: 10.1053/j.gastro.2007.10.027. PMID: 18045590. PMCID: PMC2409110.13. Ham M, Kaunitz JD. 2007; Gastroduodenal defense. Curr Opin Gastroenterol. 23:607–16. DOI: 10.1097/MOG.0b013e3282f02607. PMID: 17906436.
Article14. Chatzaki E, Lambropoulou M, Constantinidis TC, Papadopoulos N, Taché Y, Minopoulos G, Grigoriadis DE. 2006; Corticotropin-releasing factor (CRF) receptor type 2 in the human stomach: protective biological role by inhibition of apoptosis. J Cell Physiol. 209:905–11. DOI: 10.1002/jcp.20792. PMID: 16972272.
Article15. Baatar D, Kawanaka H, Szabo I, Pai R, Jones M, Kitano S, Tarnawski AS. 2002; Esophageal ulceration activates keratinocyte growth factor and its receptor in rats: implications for ulcer healing. Gastroenterology. 122:458–68. DOI: 10.1053/gast.2002.31004. PMID: 11832460.
Article16. Vanwijck R. 2001; [Surgical biology of wound healing]. Bull Mem Acad R Med Belg. 156:175–84. discussion 185French. PMID: 11789398.17. Tuch BE. 2006; Stem cells--a clinical update. Aust Fam Physician. 35:719–21. PMID: 16969445.18. Sibov TT, Severino P, Marti LC, Pavon LF, Oliveira DM, Tobo PR, Campos AH, Paes AT, Amaro E Jr, F Gamarra L, Moreira-Filho CA. 2012; Mesenchymal stem cells from umbilical cord blood: parameters for isolation, characterization and adipogenic differentiation. Cytotechnology. 64:511–21. DOI: 10.1007/s10616-012-9428-3. PMID: 22328147. PMCID: PMC3432537.
Article19. Rafei M, Birman E, Forner K, Galipeau J. 2009; Allogeneic mesenchymal stem cells for treatment of experimental autoimmune encephalomyelitis. Mol Ther. 17:1799–803. DOI: 10.1038/mt.2009.157. PMID: 19602999. PMCID: PMC2835011.
Article20. González MA, Gonzalez-Rey E, Rico L, Büscher D, Delgado M. 2009; Adipose-derived mesenchymal stem cells alleviate experimental colitis by inhibiting inflammatory and autoimmune responses. Gastroenterology. 136:978–89. DOI: 10.1053/j.gastro.2008.11.041. PMID: 19135996.
Article21. Bai L, Lennon DP, Caplan AI, DeChant A, Hecker J, Kranso J, Zaremba A, Miller RH. 2012; Hepatocyte growth factor mediates mesenchymal stem cell-induced recovery in multiple sclerosis models. Nat Neurosci. 15:862–70. DOI: 10.1038/nn.3109. PMID: 22610068. PMCID: PMC3427471.
Article22. Ren G, Zhang L, Zhao X, Xu G, Zhang Y, Roberts AI, Zhao RC, Shi Y. 2008; Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell. 2:141–50. DOI: 10.1016/j.stem.2007.11.014. PMID: 18371435.
Article23. Francis MP, Sachs PC, Elmore LW, Holt SE. 2010; Isolating adipose-derived mesenchymal stem cells from lipoaspirate blood and saline fraction. Organogenesis. 6:11–4. DOI: 10.4161/org.6.1.10019. PMID: 20592860. PMCID: PMC2861738.
Article24. Thong-Ngam D, Choochuai S, Patumraj S, Chayanupatkul M, Klaikeaw N. 2012; Curcumin prevents indomethacin-induced gastropathy in rats. World J Gastroenterol. 18:1479–84. DOI: 10.3748/wjg.v18.i13.1479. PMID: 22509079. PMCID: PMC3319943.
Article25. Ali S, ElGibaly R, Abdel-Maksoud S. 2018; Effect of Musa sapientum (Banana) on indomethacin-induced gastric mucosal injury in rats: histological study. J Med Histol. 2:11–28. DOI: 10.21608/jmh.2018.4452.1034.
Article26. Choi HS, Kim HJ, Oh JH, Park HG, Ra JC, Chang KA, Suh YH. 2015; Therapeutic potentials of human adipose-derived stem cells on the mouse model of Parkinson's disease. Neurobiol Aging. 36:2885–92. DOI: 10.1016/j.neurobiolaging.2015.06.022. PMID: 26242706.
Article27. Zickri MB, Fadl SG, Metwally HG. 2014; Comparative study between intravenous and intraperitoneal stem cell therapy in amiodarone induced lung injury in rat. Int J Stem Cells. 7:1–11. DOI: 10.15283/ijsc.2014.7.1.1. PMID: 24921022. PMCID: PMC4049726.
Article28. Kunchandy J, Khanna S, Kulkarni SK. 1985; Effect of alpha2 agonists clonidine, guanfacine and B-HT 920 on gastric acid secretion and ulcers in rats. Arch Int Pharmacodyn Ther. 275:123–38. PMID: 2862848.29. Bancroft JD, Gamble M. 2008. Theory and practice of histological techniques. 6the ed. Churchill Livingstone Elsevier;Philadelphia:30. Takahashi H, Fujita S, Yamabe S, Moriishi T, Okabe H, Tajima Y, Mizuno A. 1998; Comparison of proliferating cell nuclear antigen expression in odontogenic keratocyst and ameloblastoma: an immunohistochemical study. Anal Cell Pathol. 16:185–92. DOI: 10.1155/1998/105193. PMID: 9762365. PMCID: PMC4611129.
Article31. Jo YY, Lee HJ, Kook SY, Choung HW, Park JY, Chung JH, Choung YH, Kim ES, Yang HC, Choung PH. 2007; Isolation and characterization of postnatal stem cells from human dental tissues. Tissue Eng. 13:767–73. DOI: 10.1089/ten.2006.0192. PMID: 17432951.
Article32. Fakhry J, Wang J, Martins P, Fothergill LJ, Hunne B, Prieur P, Shulkes A, Rehfeld JF, Callaghan B, Furness JB. 2017; Distribution and characterisation of CCK containing enteroendocrine cells of the mouse small and large intestine. Cell Tissue Res. 369:245–53. DOI: 10.1007/s00441-017-2612-1. PMID: 28413860.
Article33. Khazaei M, Salehi H. 2006; Protective effect of falcaria vulgaris extract on ethanol induced gastric ulcer in rat. Iran J Pharmacol Ther. 5:43–6.34. Nauta AJ, Fibbe WE. 2007; Immunomodulatory properties of mesenchymal stromal cells. Blood. 110:3499–506. DOI: 10.1182/blood-2007-02-069716. PMID: 17664353.
Article35. Satija NK, Singh VK, Verma YK, Gupta P, Sharma S, Afrin F, Sharma M, Sharma P, Tripathi RP, Gurudutta GU. 2009; Mesenchymal stem cell-based therapy: a new paradigm in regenerative medicine. J Cell Mol Med. 13:4385–402. DOI: 10.1111/j.1582-4934.2009.00857.x. PMID: 19602034. PMCID: PMC4515054.
Article36. Inas Z, Hala A, Gehan H. 2011; Gastroprotective effect of Cordia myxa L. fruit extract against indomethacin-induced gastric ulceration in rats. Life Sci J. 8:433–45.37. Abbas AM, Sakr HF. 2013; Effect of selenium and grape seed extract on indomethacin-induced gastric ulcers in rats. J Physiol Biochem. 69:527–37. DOI: 10.1007/s13105-013-0241-z. PMID: 23456451.
Article38. Suleyman H, Albayrak A, Bilici M, Cadirci E, Halici Z. 2010; Different mechanisms in formation and prevention of indomethacin-induced gastric ulcers. Inflammation. 33:224–34. DOI: 10.1007/s10753-009-9176-5. PMID: 20084447.
Article39. Wallace JL, McKnight W, Reuter BK, Vergnolle N. 2000; NSAID-induced gastric damage in rats: requirement for inhibition of both cyclooxygenase 1 and 2. Gastroenterology. 119:706–14. DOI: 10.1053/gast.2000.16510. PMID: 10982765.
Article40. Werther JL. 2000; The gastric mucosal barrier. Mt Sinai J Med. 67:41–53. PMID: 10677782.41. Seifried HE, Anderson DE, Fisher EI, Milner JA. 2007; A review of the interaction among dietary antioxidants and reactive oxygen species. J Nutr Biochem. 18:567–79. DOI: 10.1016/j.jnutbio.2006.10.007. PMID: 17360173.
Article42. Al-sagaaf S, Ramadan WS, Abunasef SK. 2011; Does commercial aloe vera protects the structure of the gastric mucosa against acute nonsteroidal anti-inflammatory drug (diclofenac sodium)-induced damage? Egypt J Histol. 34:80–91. DOI: 10.1097/01.EHX.0000394887.77401.3d.
Article43. El-Mehi AE, El-Sherif NM. 2015; Influence of acrylamide on the gastric mucosa of adult albino rats and the possible protective role of rosemary. Tissue Cell. 47:273–83. DOI: 10.1016/j.tice.2015.03.005. PMID: 25882756.
Article44. Connolly DT. 1991; Vascular permeability factor: a unique regulator of blood vessel function. J Cell Biochem. 47:219–23. DOI: 10.1002/jcb.240470306. PMID: 1791186.
Article45. Razban V, Lotfi AS, Soleimani M, Ahmadi H, Massumi M, Khajeh S, Ghaedi M, Arjmand S, Najavand S, Khoshdel A. 2012; HIF-1α overexpression induces angiogenesis in mesenchymal stem cells. Biores Open Access. 1:174–83. DOI: 10.1089/biores.2012.9905. PMID: 23514846. PMCID: PMC3559201.
Article46. Thomson AW, Turnquist HR, Raimondi G. 2009; Immunoregulatory functions of mTOR inhibition. Nat Rev Immunol. 9:324–37. DOI: 10.1038/nri2546. PMID: 19390566. PMCID: PMC2847476.
Article47. Devine SM, Bartholomew AM, Mahmud N, Nelson M, Patil S, Hardy W, Sturgeon C, Hewett T, Chung T, Stock W, Sher D, Weissman S, Ferrer K, Mosca J, Deans R, Moseley A, Hoffman R. 2001; Mesenchymal stem cells are capable of homing to the bone marrow of non-human primates following systemic infusion. Exp Hematol. 29:244–55. DOI: 10.1016/S0301-472X(00)00635-4. PMID: 11166464.
Article48. Bernardo ME, Zaffaroni N, Novara F, Cometa AM, Avanzini MA, Moretta A, Montagna D, Maccario R, Villa R, Daidone MG, Zuffardi O, Locatelli F. 2007; Human bone marrow derived mesenchymal stem cells do not undergo transformation after long-term in vitro culture and do not exhibit telomere maintenance mechanisms. Cancer Res. 67:9142–9. DOI: 10.1158/0008-5472.CAN-06-4690. PMID: 17909019.49. Binato R, de Souza Fernandez T, Lazzarotto-Silva C, Du Rocher B, Mencalha A, Pizzatti L, Bouzas LF, Abdelhay E. 2013; Stability of human mesenchymal stem cells during in vitro culture: considerations for cell therapy. Cell Prolif. 46:10–22. DOI: 10.1111/cpr.12002. PMID: 23163975. PMCID: PMC6496525.50. Teixeira FG, Salgado AJ. 2020; Mesenchymal stem cells secretome: current trends and future challenges. Neural Regen Res. 15:75–7. DOI: 10.4103/1673-5374.264455. PMID: 31535654. PMCID: PMC6862404.
Article51. Toma C, Pittenger MF, Cahill KS, Byrne BJ, Kessler PD. 2002; Human mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult murine heart. Circulation. 105:93–8. DOI: 10.1161/hc0102.101442. PMID: 11772882.
Article52. Fan H, Zhao G, Liu L, Liu F, Gong W, Liu X, Yang L, Wang J, Hou Y. 2012; Pre-treatment with IL-1β enhances the efficacy of MSC transplantation in DSS-induced colitis. Cell Mol Immunol. 9:473–81. DOI: 10.1038/cmi.2012.40. PMID: 23085948. PMCID: PMC4002219.
Article53. Danese S, Rutella S, Vetrano S. 2013; Mesenchymal stromal cells in inflammatory bowel disease: conspirators within the 'colitogenic niche'? Gut. 62:1098–9. DOI: 10.1136/gutjnl-2012-303903. PMID: 23263523.
Article54. Hayashi Y, Tsuji S, Tsujii M, Nishida T, Ishii S, Iijima H, Nakamura T, Eguchi H, Miyoshi E, Hayashi N, Kawano S. 2008; Topical transplantation of mesenchymal stem cells accelerates gastric ulcer healing in rats. Am J Physiol Gastrointest Liver Physiol. 294:G778–86. DOI: 10.1152/ajpgi.00468.2007. PMID: 18202110.
Article55. Matsumoto K, Nakamura T. 1997; Hepatocyte growth factor (HGF) as a tissue organizer for organogenesis and regeneration. Biochem Biophys Res Commun. 239:639–44. DOI: 10.1006/bbrc.1997.7517. PMID: 9367820.
Article56. Ezquer F, Bahamonde J, Huang YL, Ezquer M. 2017; Administration of multipotent mesenchymal stromal cells restores liver regeneration and improves liver function in obese mice with hepatic steatosis after partial hepatectomy. Stem Cell Res Ther. 8:20. DOI: 10.1186/s13287-016-0469-y. PMID: 28129776. PMCID: PMC5273822.
Article57. Jiang H, Qu L, Dou R, Lu L, Bian S, Zhu W. 2013; Potential role of mesenchymal stem cells in alleviating intestinal ischemia/reperfusion impairment. PLoS One. 8:e74468. DOI: 10.1371/journal.pone.0074468. PMID: 24058571. PMCID: PMC3772852.
Article58. Liu ZJ, Zhuge Y, Velazquez OC. 2009; Trafficking and differentiation of mesenchymal stem cells. J Cell Biochem. 106:984–91. DOI: 10.1002/jcb.22091. PMID: 19229871.
Article59. Meligy FY, Shigemura K, Behnsawy HM, Fujisawa M, Kawabata M, Shirakawa T. 2012; The efficiency of in vitro isolation and myogenic differentiation of MSCs derived from adipose connective tissue, bone marrow, and skeletal muscle tissue. In Vitro Cell Dev Biol Anim. 48:203–15. DOI: 10.1007/s11626-012-9488-x. PMID: 22396125.60. Kallmeyer K, Pepper MS. 2015; Homing properties of mesenchymal stromal cells. Expert Opin Biol Ther. 15:477–9. DOI: 10.1517/14712598.2015.997204. PMID: 25539087.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- L-Theanine-Treated Adipose-Derived Mesenchymal Stem Cells Alleviate the Cytotoxicity Induced by N-Nitrosodiethylamine in Liver
- Adipose Stem Cells as Alternatives for Bone Marrow Mesenchymal Stem Cells in Oral Ulcer Healing
- Adipose Tissue - Adequate, Accessible Regenerative Material
- Clinical Application of Adipose Stem Cells in Plastic Surgery
- Concise Review: Differentiation of Human Adult Stem Cells Into Hepatocyte-like Cells In vitro