J Stroke.
2021 Sep;23(3):411-419. 10.5853/jos.2020.04889.
Thrombolysis Improves Reperfusion and the Clinical Outcome in Tandem Occlusion Stroke Related to Cervical Dissection: TITAN and ETIS Pooled Analysis
- Affiliations
-
- 1Department of Neuroradiology, University Hospital of Bordeaux, Bordeaux, France
- 2Department of Neurology, University Hospital of Bordeaux, Bordeaux, France
- 3Department of Neuroradiology, University Hospital of Nantes, Nantes, France
- 4Department of Neurology, Washington University School of Medicine, St. Louis, MO, USA
- 5Department of Biostatistics, University of Lille, Lille, France
- 6Department of Interventional Neuroradiology, Rothschild Foundation, Paris, France
- 7Department of Neuroradiology, CHRU Gui-de-Chauliac, Montpellier, France
- 8Department of Neuroradiology, Foch Hospital, Versailles Saint-Quentin-en-Yvelines University, Suresnes, France
- 9Department of Diagnostic and Therapeutic Neuroradiology, University of Lorraine, CHRU-Nancy, Nancy, France
- 10Université de Lorraine, IADI, INSERM U1254, Nancy, France
- 11Department of Anesthesiology and Intensive Care, University of Lorraine, University Hospital of Nancy, Nancy, France
- 12Stroke Unit, Department of Neurology, University of Lorraine, University Hospital of Nancy, and INSERM U1116, Nancy, France
- 13Department of Neurology, Foch Hospital, Versailles Saint-Quentin-en-Yvelines University, Suresnes, France
- KMID: 2520918
- DOI: http://doi.org/10.5853/jos.2020.04889
Abstract
- Background and Purpose
Despite the widespread adoption of mechanical thrombectomy (MT) for the treatment of large vessel occlusion stroke (LVOS) in the anterior circulation, the optimal strategy for the treatment tandem occlusion related to cervical internal carotid artery (ICA) dissection is still debated. This individual patient pooled analysis investigated the safety and efficacy of prior intravenous thrombolysis (IVT) in anterior circulation tandem occlusion related to cervical ICA dissection treated with MT.
Methods
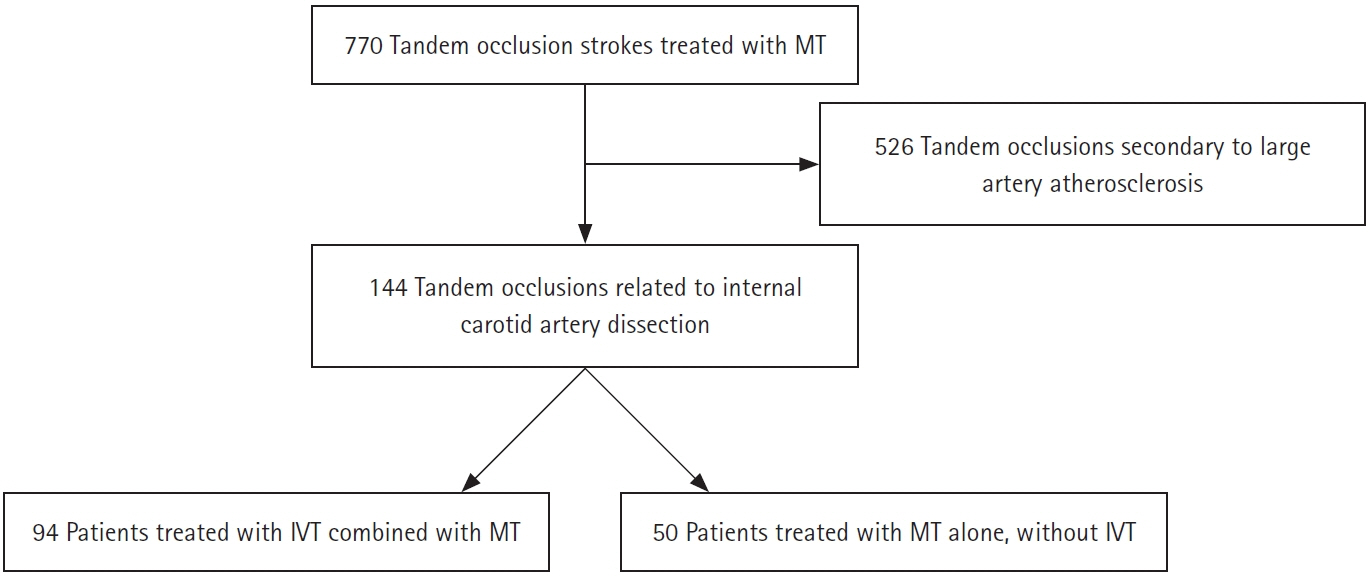
We performed a retrospective analysis of two merged prospective multicenter international real-world observational registries: Endovascular Treatment in Ischemic Stroke (ETIS) and Thrombectomy In TANdem occlusions (TITAN) registries. Data from MT performed in the treatment of tandem LVOS related to cervical ICA dissection between January 2012 and December 2019 at 24 comprehensive stroke centers were analyzed. The primary endpoint was a favorable outcome defined as 90-day modified Rankin Scale (mRS) score of 0–2.
Results
The study included 144 patients with tandem occlusion LVOS due to cervical ICA dissection, of whom 94 (65.3%) received IVT before MT. Prior IVT was significantly associated with a better clinical outcome considering the mRS shift analysis (common odds ratio, 2.59; 95% confidence interval [CI], 1.35 to 4.93; P=0.004 for a 1-point improvement) and excellent outcome (90-day mRS 0–1) (adjusted odds ratio [aOR], 4.23; 95% CI, 1.60 to 11.18). IVT was also associated with a higher rate of intracranial successful reperfusion (83.0% vs. 64.0%; aOR, 2.70; 95% CI, 1.21 to 6.03) and a lower rate of symptomatic intracranial hemorrhage (4.3% vs. 14.8%; aOR, 0.21; 95% CI, 0.05 to 0.80).
Conclusions
Prior IVT before MT for the treatment of tandem occlusion related to cervical ICA dissection was safe and associated with an improved 90-day functional outcome.
Figure
Reference
-
References
1. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article2. Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. 2020; 382:1981–1993.
Article3. Suzuki K, Matsumaru Y, Takeuchi M, Morimoto M, Kanazawa R, Takayama Y, et al. Effect of mechanical thrombectomy without vs with intravenous thrombolysis on functional outcome among patients with acute ischemic stroke: the SKIP randomized clinical trial. JAMA. 2021; 325:244–253.4. Zi W, Qiu Z, Li F, Sang H, Wu D, Luo W, et al. Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: the DEVT randomized clinical trial. JAMA. 2021; 325:234–243.5. Treurniet KM, LeCouffe NE, Kappelhof M, Emmer BJ, van Es ACGM, Boiten J, et al. MR CLEAN-NO IV: intravenous treatment followed by endovascular treatment versus direct endovascular treatment for acute ischemic stroke caused by a proximal intracranial occlusion-study protocol for a randomized clinical trial. Trials. 2021; 22:141.
Article6. Lin J, Sun Y, Zhao S, Xu J, Zhao C. Safety and efficacy of thrombolysis in cervical artery dissection-related ischemic stroke: a meta-analysis of observational studies. Cerebrovasc Dis. 2016; 42:272–279.
Article7. Engelter ST, Dallongeville J, Kloss M, Metso TM, Leys D, Brandt T, et al. Thrombolysis in cervical artery dissection: data from the Cervical Artery Dissection and Ischaemic Stroke Patients (CADISP) database. Eur J Neurol. 2012; 19:1199–1206.8. CADISS trial investigators, Markus HS, Hayter E, Levi C, Feldman A, Venables G, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015; 14:361–367.9. Marnat G, Bühlmann M, Eker OF, Gralla J, Machi P, Fischer U, et al. Multicentric experience in distal-to-proximal revascularization of tandem occlusion stroke related to internal carotid artery dissection. AJNR Am J Neuroradiol. 2018; 39:1093–1099.
Article10. Marnat G, Lapergue B, Sibon I, Gariel F, Bourcier R, Kyheng M, et al. Safety and outcome of carotid dissection stenting during the treatment of tandem occlusions: a pooled analysis of TITAN and ETIS. Stroke. 2020; 51:3713–3718.11. Compagne KCJ, Goldhoorn RB, Uyttenboogaart M, van Oostenbrugge RJ, van Zwam WH, van Doormaal PJ, et al. Acute endovascular treatment of patients with ischemic stroke from intracranial large vessel occlusion and extracranial carotid dissection. Front Neurol. 2019; 10:102.
Article12. Gory B, Piotin M, Haussen DC, Steglich-Arnholm H, Holtmannspötter M, Labreuche J, et al. Thrombectomy in acute stroke with tandem occlusions from dissection versus atherosclerotic cause. Stroke. 2017; 48:3145–3148.
Article13. Mistry EA, Mistry AM, Nakawah MO, Chitale RV, James RF, Volpi JJ, et al. Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients: a meta-analysis. Stroke. 2017; 48:2450–2456.
Article14. Gariel F, Lapergue B, Bourcier R, Berge J, Barreau X, Mazighi M, et al. Mechanical thrombectomy outcomes with or without intravenous thrombolysis. Stroke. 2018; 49:2383–2390.
Article15. Ospel JM, Singh N, Almekhlafi MA, Menon BK, Butt A, Poppe AY, et al. Early recanalization with alteplase in stroke because of large vessel occlusion in the ESCAPE trial. Stroke. 2021; 52:304–307.
Article16. Zhu F, Anadani M, Labreuche J, Spiotta A, Turjman F, Piotin M, et al. Impact of antiplatelet therapy during endovascular therapy for tandem occlusions: a collaborative pooled analysis. Stroke. 2020; 51:1522–1529.17. Georgiadis D, Lanczik O, Schwab S, Engelter S, Sztajzel R, Arnold M, et al. IV thrombolysis in patients with acute stroke due to spontaneous carotid dissection. Neurology. 2005; 64:1612–1614.
Article18. Tsivgoulis G, Zand R, Katsanos AH, Sharma VK, Goyal N, Krogias C, et al. Safety and outcomes of intravenous thrombolysis in dissection-related ischemic stroke: an international multicenter study and comprehensive meta-analysis of reported case series. J Neurol. 2015; 262:2135–2143.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Emergent Recanalization with Stenting for Acute Stroke due to Athero-Thrombotic Occlusion of the Cervical Internal Carotid Artery : A Single Center Experience
- Thrombolytic Treatment of Acute Stroke
- Successful Endovascular Mechanical Thrombolysis in a Patient with Hyperacute Tandem Occlusions of Middle Cerebral Artery and Extracranial Internal Carotid Artery
- Review of Stroke Thrombolytics
- Reperfusion therapy in acute ischemic stroke