Diabetes Metab J.
2021 Sep;45(5):765-772. 10.4093/dmj.2021.0096.
Effects of Social Distancing on Diabetes Management in Older Adults during COVID-19 Pandemic
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2520858
- DOI: http://doi.org/10.4093/dmj.2021.0096
Abstract
- Background
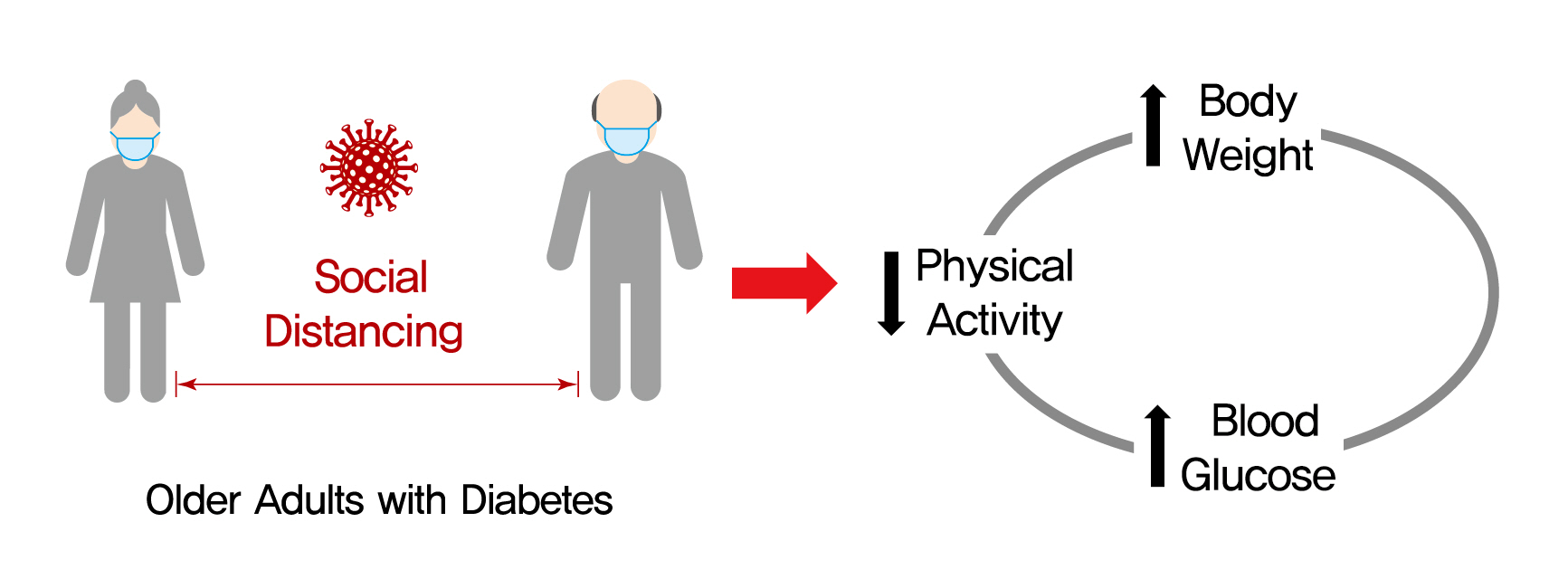
On March 22, 2020, intense social distancing (SD) was implemented in Korea to prevent the spread of coronavirus disease 19 (COVID-19). This study examined the impact of SD on diabetes control in older adults with diabetes.
Methods
Adults aged 60 to 90 years with type 2 diabetes mellitus who were physically and mentally independent were recruited. Participants who had complete blood chemistry data from April to July 2019 (pre-SD era) and April to July 2020 (SD era) were enrolled. Data were obtained about physical activity, nutrition, sarcopenia, and psychological and mental health from questionnaires in April to July 2020. Calf circumference was measured.
Results
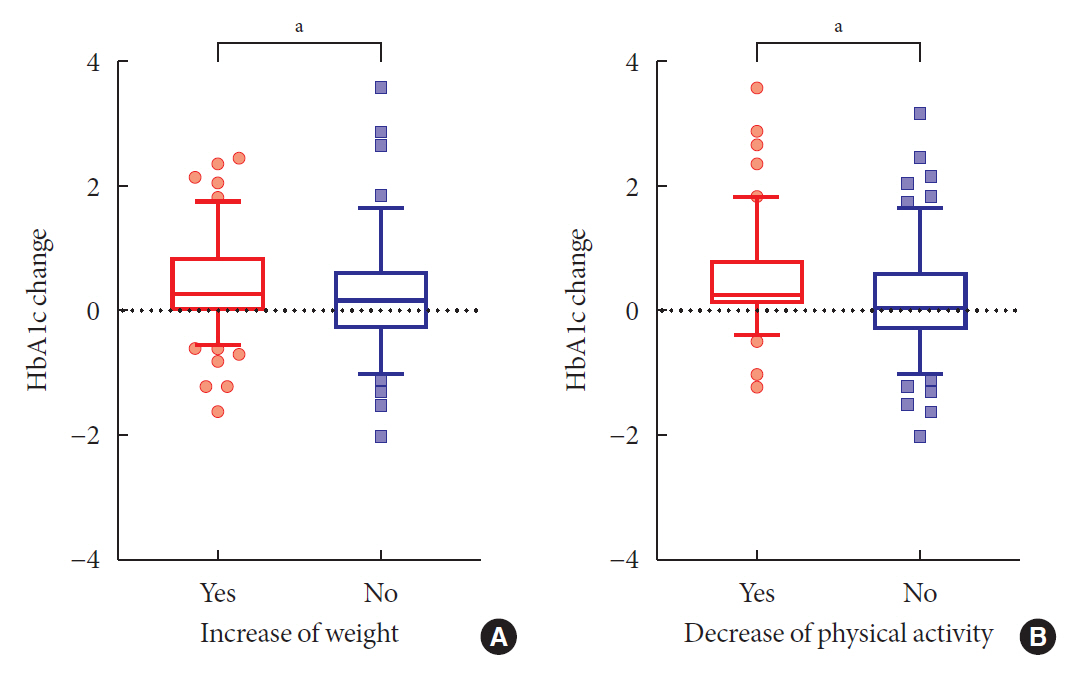
In total, 246 people (100 men, 146 women; mean age, 73.8±5.7 years) participated in this study. The levels of glycated hemoglobin (HbA1c, 7.4%±1.0% vs. 7.1%±0.8%, P<0.001), fasting glucose (142.2±16.7 mg/dL vs. 132.0±27.7 mg/dL, P<0.001), and body weight (62.6±9.4 kg vs. 61.8±10.1 kg, P<0.01) were higher in the SD era than in the pre-SD era. Total physical activity was lower in the SD era (2,584.6±2,624.1 MET-min/week–1 vs. 1,987.3±2,295.0 MET-min/week–1, P<0.001). A larger increase in HbA1c level was associated with increased body weight and decreased physical activity.
Conclusion
SD had negative effects on diabetes management in older adults with diabetes. Fasting glucose and HbA1c levels and body weight increased during the SD era. Participants with reduced physical activity gained more weight and had higher blood glucose levels. Given that the COVID-19 pandemic is ongoing, health professionals and diabetes educators should monitor changes in lifestyle factors in older adults with diabetes.
Keyword
Figure
Reference
-
1. Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020; 35:e112.2. Korean Society of Infectious Diseases and Korea Centers for Disease Control and Prevention. Analysis on 54 mortality cases of coronavirus disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J Korean Med Sci. 2020; 35:e132.3. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020; 324:782–93.4. Myers LC, Parodi SM, Escobar GJ, Liu VX. Characteristics of hospitalized adults with COVID-19 in an integrated health care system in California. JAMA. 2020; 323:2195–8.
Article5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323:1239–42.6. Jordan RE, Adab P, Cheng KK. COVID-19: risk factors for severe disease and death. BMJ. 2020; 368:m1198.
Article7. Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med. 2020; 382:2372–4.
Article8. Park IN, Yum HK. Stepwise strategy of social distancing in Korea. J Korean Med Sci. 2020; 35:e264.
Article9. Munekawa C, Hosomi Y, Hashimoto Y, Okamura T, Takahashi F, Kawano R, et al. Effect of coronavirus disease 2019 pandemic on the lifestyle and glycemic control in patients with type 2 diabetes: a cross-section and retrospective cohort study. Endocr J. 2021; 68:201–10.
Article10. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020; 180:817–8.11. Lim WS, Liang CK, Assantachai P, Auyeung TW, Kang L, Lee WJ, et al. COVID-19 and older people in Asia: Asian Working Group for Sarcopenia calls to actions. Geriatr Gerontol Int. 2020; 20:547–58.12. Oh JY, Yang YJ, Kim BS, Kang JH. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. J Korean Acad Fam Med. 2007; 28:532–41.13. Maugeri G, Castrogiovanni P, Battaglia G, Pippi R, D’Agata V, Palma A, et al. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon. 2020; 6:e04315.
Article14. Kim S, Kim M, Won CW. Validation of the Korean version of the SARC-F questionnaire to assess sarcopenia: Korean frailty and aging cohort study. J Am Med Dir Assoc. 2018; 19:40–5.
Article15. Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020; 21:300–7.
Article16. Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin Geriatr Med. 2002; 18:737–57.17. Eun HJ, Kwon TW, Lee SM, Kim TH, Choi MR, Cho SJ. A study on reliability and validity of the Korean version of Impact of Event Scale-Revised. J Korean Neuropsychiatr Assoc. 2005; 44:303–10.18. Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. 2008; 49:218–23.
Article19. Park SD, Kim SW, Moon JS, Lee YY, Cho NH, Lee JH, et al. Impact of social distancing due to coronavirus disease 2019 on the changes in glycosylated hemoglobin level in people with type 2 diabetes mellitus. Diabetes Metab J. 2021; 45:109–14.
Article20. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients. 2020; 12:1583.21. Lim S, Lim H, Despres JP. Collateral damage of the COVID-19 pandemic on nutritional quality and physical activity: perspective from South Korea. Obesity (Silver Spring). 2020; 28:1788–90.
Article22. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020; 324:93–4.
Article23. Czeisler ME, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic: United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1049–57.24. van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, de Vries DH. Loneliness and mental health during the COVID-19 pandemic: a study among Dutch older adults. J Gerontol B Psychol Sci Soc Sci. 2021; 76:e249–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review of the Health of the Elderly on the Impact of Social Isolation and Loneliness: Focusing on the Coronavirus Disease (COVID-19) Pandemic
- Social Connectedness and Cognitive Function Before and During COVID-19: A Longitudinal Study of Korean Older Adults With an Instrumental Variable Regression
- Dietary Habits of Diabetes Patients during the COVID-19 Pandemic
- A Comparison of the Perception of and Adherence to the COVID-19 Social Distancing Behavior Guidelines among Health Care Workers, Patients, and General Public
- Psychosocial changes in Medical Students Before and After COVID-19 Social Distancing