Diabetes Metab J.
2021 Sep;45(5):698-707. 10.4093/dmj.2020.0118.
Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2520852
- DOI: http://doi.org/10.4093/dmj.2020.0118
Abstract
- Background
This study aimed to investigate the association between hepatic steatosis burden and albuminuria in Korean patients with type 2 diabetes mellitus (T2DM) and nonalcoholic fatty liver disease (NAFLD).
Methods
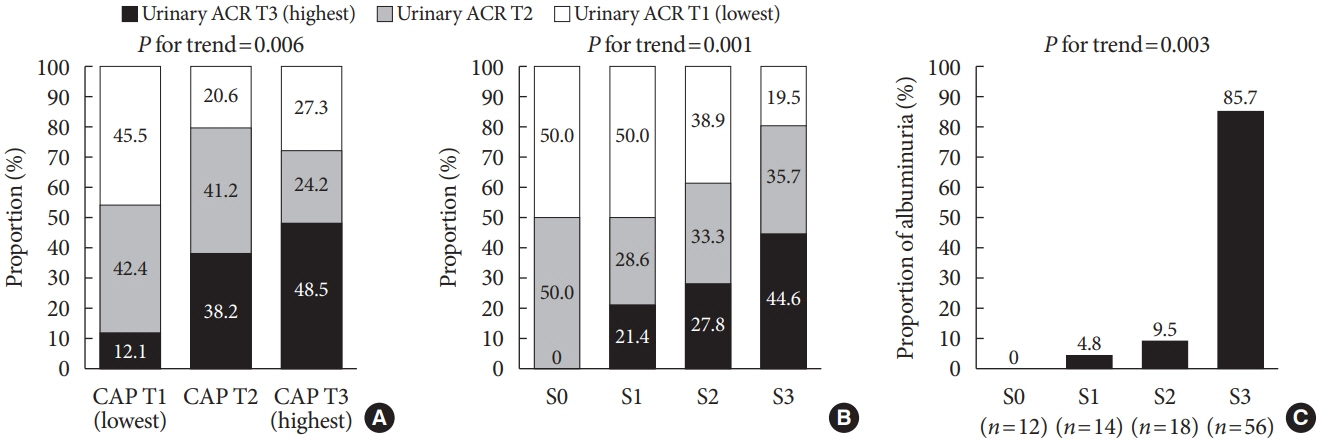
We recruited 100 patients with both T2DM and NAFLD, but without chronic kidney disease. Albuminuria was defined as a spot urinary albumin-to-creatinine ratio (ACR) ≥30 mg/g. Transient elastography was performed, and the steatosis burden was quantified by controlled attenuation parameter (CAP) with significant steatosis defined as CAP >302 dB/m.
Results
The prevalence of significant steatosis and albuminuria was 56.0% and 21.0%, respectively. Subjects with significant steatosis were significantly younger and had a significantly shorter duration of T2DM, greater waist circumference, and higher body mass index, total cholesterol, triglyceride, and low density lipoprotein cholesterol levels, than subjects without severe NAFLD (all P<0.05). Albuminuria was higher in patients with significant steatosis than in patients without significant steatosis (32.1% vs. 6.8%, P=0.002). Urinary ACR showed a correlation with CAP (r=0.331, P=0.001), and multiple linear regression analysis revealed a significant association between a high degree of albuminuria and high CAP value (r=0.321, P=0.001). Additionally, multivariate logistic regression analysis demonstrated the independent association between urinary ACR and significant steatosis after adjustment for confounding factors including age, body mass index, duration of T2DM, low density lipoprotein level, and renin-angiotensin system blocker use (odds ratio, 1.88; 95% confidence interval, 1.31 to 2.71; P=0.001).
Conclusion
T2DM patients with NAFLD had a higher prevalence of albuminuria, which correlated with their steatosis burden.
Figure
Cited by 3 articles
-
Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (
Diabetes Metab J 2021;45:698-707)
Eugene Han, Hye Soon Kim
Diabetes Metab J. 2021;45(6):972-973. doi: 10.4093/dmj.2021.0315.Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (
Diabetes Metab J 2021;45:698-707)
Mi-kyung Kim
Diabetes Metab J. 2021;45(6):968-969. doi: 10.4093/dmj.2021.0311.Beyond Liver Disease: Non-Alcoholic Fatty Liver Disease and Advanced Liver Fibrosis in Kidney Disease
Eugene Han
Diabetes Metab J. 2022;46(4):564-566. doi: 10.4093/dmj.2022.0203.
Reference
-
1. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease: meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016; 64:73–84.
Article2. Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol. 2019; 71:793–801.
Article3. Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Serag HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016; 14:301–8.4. Lee YH, Cho Y, Lee BW, Park CY, Lee DH, Cha BS, et al. Nonalcoholic fatty liver disease in diabetes. Part I: epidemiology and diagnosis. Diabetes Metab J. 2019; 43:31–45.
Article5. Torres DM, Harrison SA. Nonalcoholic steatohepatitis and noncirrhotic hepatocellular carcinoma: fertile soil. Semin Liver Dis. 2012; 32:30–8.
Article6. Yu J, Shen J, Sun TT, Zhang X, Wong N. Obesity, insulin resistance, NASH and hepatocellular carcinoma. Semin Cancer Biol. 2013; 23(6 Pt B):483–91.
Article7. Yoo JS, Lee YM, Lee EH, Kim JW, Lee SY, Jeong KC, et al. Serum cystatin C reflects the progress of albuminuria. Diabetes Metab J. 2011; 35:602–9.
Article8. Yun KJ, Kim HJ, Kim MK, Kwon HS, Baek KH, Roh YJ, et al. Risk factors for the development and progression of diabetic kidney disease in patients with type 2 diabetes mellitus and advanced diabetic retinopathy. Diabetes Metab J. 2016; 40:473–81.
Article9. Han E, Cho NH, Kim MK, Kim HS. Lower leg fat depots are associated with albuminuria independently of obesity, insulin resistance, and metabolic syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011). Diabetes Metab J. 2019; 43:461–73.
Article10. Han E, Lee YH, Kim G, Kim SR, Lee BW, Kang ES, et al. Sarcopenia is associated with albuminuria independently of hypertension and diabetes: KNHANES 2008-2011. Metabolism. 2016; 65:1531–40.
Article11. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020; 43(Suppl 1):S14–31.12. Lee YH, Kim JH, Kim SR, Jin HY, Rhee EJ, Cho YM, et al. Lobeglitazone, a novel thiazolidinedione, improves non-alcoholic fatty liver disease in type 2 diabetes: its efficacy and predictive factors related to responsiveness. J Korean Med Sci. 2017; 32:60–9.
Article13. Han E, Lee YH, Lee BW, Kang ES, Cha BS. Ipragliflozin additively ameliorates non-alcoholic fatty liver disease in patients with type 2 diabetes controlled with metformin and pioglitazone: a 24-week randomized controlled trial. J Clin Med. 2020; 9:259.
Article14. Chon YE, Jung KS, Kim SU, Park JY, Park YN, Kim DY, et al. Controlled attenuation parameter (CAP) for detection of hepatic steatosis in patients with chronic liver diseases: a prospective study of a native Korean population. Liver Int. 2014; 34:102–9.
Article15. Eddowes PJ, Sasso M, Allison M, Tsochatzis E, Anstee QM, Sheridan D, et al. Accuracy of fibroscan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019; 156:1717–30.
Article16. Imajo K, Kessoku T, Honda Y, Tomeno W, Ogawa Y, Mawatari H, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology. 2016; 150:626–37.
Article17. Bellan M, Colletta C, Barbaglia MN, Salmi L, Clerici R, Mallela VR, et al. Severity of nonalcoholic fatty liver disease in type 2 diabetes mellitus: relationship between nongenetic factors and PNPLA3/HSD17B13 polymorphisms. Diabetes Metab J. 2019; 43:700–10.
Article18. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999; 130:461–70.19. Oh SW. Obesity and metabolic syndrome in Korea. Diabetes Metab J. 2011; 35:561–6.
Article20. Han E, Lee YH. Non-alcoholic fatty liver disease: the emerging burden in cardiometabolic and renal diseases. Diabetes Metab J. 2017; 41:430–7.
Article21. Targher G, Bertolini L, Rodella S, Lippi G, Zoppini G, Chonchol M. Relationship between kidney function and liver histology in subjects with nonalcoholic steatohepatitis. Clin J Am Soc Nephrol. 2010; 5:2166–71.
Article22. Wijarnpreecha K, Thongprayoon C, Boonpheng B, Panjawatanan P, Sharma K, Ungprasert P, et al. Nonalcoholic fatty liver disease and albuminuria: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2018; 30:986–94.
Article23. Yeung MW, Wong GL, Choi KC, Luk AO, Kwok R, Shu SS, et al. Advanced liver fibrosis but not steatosis is independently associated with albuminuria in Chinese patients with type 2 diabetes. J Hepatol. 2018; 68:147–56.
Article24. Hwang ST, Cho YK, Yun JW, Park JH, Kim HJ, Park DI, et al. Impact of non-alcoholic fatty liver disease on microalbuminuria in patients with prediabetes and diabetes. Intern Med J. 2010; 40:437–42.
Article25. Jia G, Di F, Wang Q, Shao J, Gao L, Wang L, et al. Non-alcoholic fatty liver disease is a risk factor for the development of diabetic nephropathy in patients with type 2 diabetes mellitus. PLoS One. 2015; 10:e0142808.
Article26. Fraquelli M, Rigamonti C, Casazza G, Conte D, Donato MF, Ronchi G, et al. Reproducibility of transient elastography in the evaluation of liver fibrosis in patients with chronic liver disease. Gut. 2007; 56:968–73.
Article27. McPherson S, Hardy T, Dufour JF, Petta S, Romero-Gomez M, Allison M, et al. Age as a confounding factor for the accurate non-invasive diagnosis of advanced NAFLD fibrosis. Am J Gastroenterol. 2017; 112:740–51.
Article28. Chang PE, Lui HF, Chau YP, Lim KH, Yap WM, Tan CK, et al. Prospective evaluation of transient elastography for the diagnosis of hepatic fibrosis in Asians: comparison with liver biopsy and aspartate transaminase platelet ratio index. Aliment Pharmacol Ther. 2008; 28:51–61.
Article29. McPherson S, Anstee QM, Henderson E, Day CP, Burt AD. Are simple noninvasive scoring systems for fibrosis reliable in patients with NAFLD and normal ALT levels? Eur J Gastroenterol Hepatol. 2013; 25:652–8.
Article30. Pilz S, Rutters F, Nijpels G, Stehouwer CD, Hojlund K, Nolan JJ, et al. Insulin sensitivity and albuminuria: the RISC study. Diabetes Care. 2014; 37:1597–603.
Article31. Kim KS, Lee BW, Kim YJ, Lee DH, Cha BS, Park CY. Nonalcoholic fatty liver disease and diabetes. Part II: treatment. Diabetes Metab J. 2019; 43:127–43.
Article32. Gupta J, Mitra N, Kanetsky PA, Devaney J, Wing MR, Reilly M, et al. Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC. Clin J Am Soc Nephrol. 2012; 7:1938–46.
Article33. Haukeland JW, Damas JK, Konopski Z, Loberg EM, Haaland T, Goverud I, et al. Systemic inflammation in nonalcoholic fatty liver disease is characterized by elevated levels of CCL2. J Hepatol. 2006; 44:1167–74.
Article34. Eardley KS, Zehnder D, Quinkler M, Lepenies J, Bates RL, Savage CO, et al. The relationship between albuminuria, MCP-1/CCL2, and interstitial macrophages in chronic kidney disease. Kidney Int. 2006; 69:1189–97.
Article35. Matthew Morris E, Fletcher JA, Thyfault JP, Rector RS. The role of angiotensin II in nonalcoholic steatohepatitis. Mol Cell Endocrinol. 2013; 378:29–40.
Article36. Musso G, Cassader M, Cohney S, Pinach S, Saba F, Gambino R. Emerging liver-kidney interactions in nonalcoholic fatty liver disease. Trends Mol Med. 2015; 21:645–62.
Article37. Sun DQ, Zheng KI, Xu G, Ma HL, Zhang HY, Pan XY, et al. PNPLA3 rs738409 is associated with renal glomerular and tubular injury in NAFLD patients with persistently normal ALT levels. Liver Int. 2020; 40:107–19.38. Dong XC. PNPLA3: a potential therapeutic target for personalized treatment of chronic liver disease. Front Med (Lausanne). 2019; 6:304.
Article39. Hu X, Huang Y, Bao Z, Wang Y, Shi D, Liu F, et al. Prevalence and factors associated with nonalcoholic fatty liver disease in Shanghai work-units. BMC Gastroenterol. 2012; 12:123.
Article40. Wong VW, Chu WC, Wong GL, Chan RS, Chim AM, Ong A, et al. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography. Gut. 2012; 61:409–15.
Article41. Mor A, Svensson E, Rungby J, Ulrichsen SP, Berencsi K, Nielsen JS, et al. Modifiable clinical and lifestyle factors are associated with elevated alanine aminotransferase levels in newly diagnosed type 2 diabetes patients: results from the nationwide DD2 study. Diabetes Metab Res Rev. 2014; 30:707–15.
Article42. Doycheva I, Cui J, Nguyen P, Costa EA, Hooker J, Hofflich H, et al. Non-invasive screening of diabetics in primary care for NAFLD and advanced fibrosis by MRI and MRE. Aliment Pharmacol Ther. 2016; 43:83–95.
Article43. Doycheva I, Watt KD, Alkhouri N. Nonalcoholic fatty liver disease in adolescents and young adults: the next frontier in the epidemic. Hepatology. 2017; 65:2100–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
- Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
- Noninvasive serum biomarkers for liver steatosis in nonalcoholic fatty liver disease: Current and future developments
- Management of Patients with Nonalcoholic Fatty Liver Disease with Lifestyle Modification
- Recent update on pathogenesis of nonalcoholic fatty liver disease