Diabetes Metab J.
2021 Sep;45(5):629-640. 10.4093/dmj.2021.0163.
A Century of Progress in Diabetes Care with Insulin: A History of Innovations and Foundation for the Future
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Medical Informatics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2520847
- DOI: http://doi.org/10.4093/dmj.2021.0163
Abstract
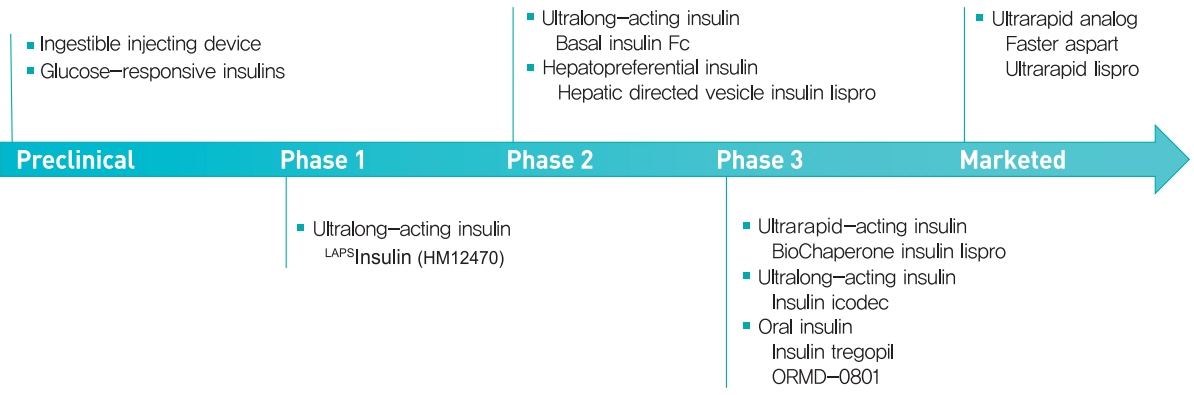
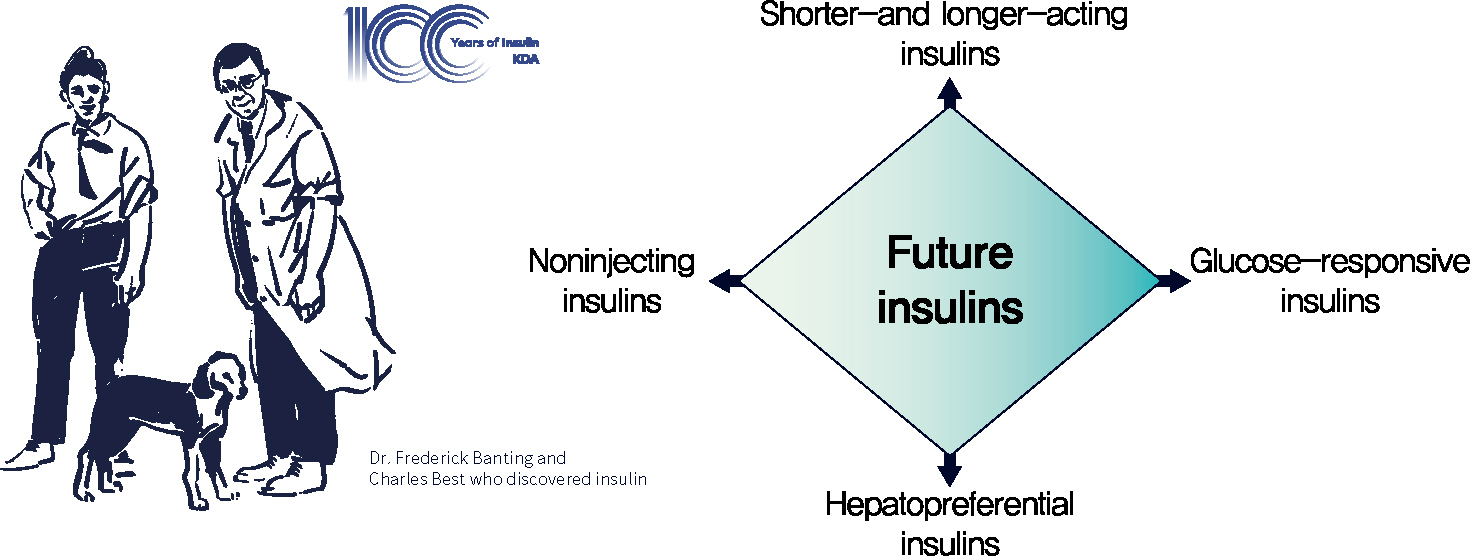
- The year 2021 marks the 100th anniversary of the discovery of insulin, which has greatly changed the lives of people with diabetes and become a cornerstone of advances in medical science. A rapid bench-to-bedside application of the lifesaving pancreatic extract and its immediate commercialization was the result of a promising idea, positive drive, perseverance, and collaboration of Banting and colleagues. As one of the very few proteins isolated in a pure form at that time, insulin also played a key role in the development of important methodologies and in the beginning of various fields of modern science. Since its discovery, insulin has evolved continuously to optimize the care of people with diabetes. Since the 1980s, recombinant DNA technology has been employed to engineer insulin analogs by modifying their amino acid sequence, which has resulted in the production of insulins with various profiles that are currently used. However, unmet needs in insulin treatment still exist, and several forms of future insulins are under development. In this review, we discuss the past, present, and future of insulin, including a history of ceaseless innovations and collective intelligence. We believe that this story will be a solid foundation and an unerring guide for the future.
Keyword
Figure
Cited by 1 articles
-
Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinol Metab. 2022;37(3):415-429. doi: 10.3803/EnM.2022.304.
Reference
-
1. Pickup J, Williams G. Textbook of diabetes. 3rd ed. Oxford: Blackwell Science;2003.2. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021; 45:1–10.
Article3. Rhee EJ. Prevalence and current management of cardiovascular risk factors in Korean adults based on fact sheets. Endocrinol Metab (Seoul). 2020; 35:85–94.
Article4. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843.
Article5. von Mering J, Minkowski O. Diabetes mellitus nach Pankreasextirpation. Arch Exp Pathol Pharmakol. 1890; 26:371–87.6. Laguesse G. Sur la formation des ilots de Langerhans dans le pancréas. C R Soc Biol. 1893; 45:819–20.7. Scott EL. On the influence of intravenous injections of an extract of the pancreas on experimental pancreatic diabetes. Am J Physiol Leg Content. 1912; 29:306–10.
Article8. Paulesco NC. Recherches sur le rôle du pancréas dans l’assimilation nutritive. Arch Int Physiol. 1921; 17:85–109.9. Kleiner IS, Meltzer SJ. Retention in the circulation of dextrose in normal and depancreatized animals, and the effect of an intravenous injection of an emulsion of pancreas upon this retention. Proc Natl Acad Sci U S A. 1915; 1:338–41.
Article10. Murlin JR, Kramer B. The influence of pancreatic and duodenal extracts on the glycosuria and the respiratory metabolism of depancreatized dogs. Proc Soc Exp Biol Med. 1913; 10:171–3.
Article11. Hegele RA, Maltman GM. Insulin’s centenary: the birth of an idea. Lancet Diabetes Endocrinol. 2020; 8:971–7.
Article12. Lewis GF, Brubaker PL. The discovery of insulin revisited: lessons for the modern era. J Clin Invest. 2021; 131:e142239.
Article13. Barron M. The relation of the islets of Langerhans to diabetes with special reference to cases of pancreatic lithiasis. Surg Gynecol Obstet. 1920; 31:437–48.14. Banting FG, Best CH, Collip JB, Campbell WR, Fletcher AA. Pancreatic extracts in the treatment of diabetes mellitus. Can Med Assoc J. 1922; 12:141–6.
Article15. Xu X, D’Hoker J, Stange G, Bonne S, De Leu N, Xiao X, et al. Beta cells can be generated from endogenous progenitors in injured adult mouse pancreas. Cell. 2008; 132:197–207.16. Van de Casteele M, Leuckx G, Baeyens L, Cai Y, Yuchi Y, Coppens V, et al. Neurogenin 3+ cells contribute to β-cell neogenesis and proliferation in injured adult mouse pancreas. Cell Death Dis. 2013; 4:e523.
Article17. Rankin MM, Wilbur CJ, Rak K, Shields EJ, Granger A, Kushner JA. β-Cells are not generated in pancreatic duct ligation-induced injury in adult mice. Diabetes. 2013; 62:1634–45.
Article18. Van de Casteele M, Leuckx G, Cai Y, Yuchi Y, Coppens V, De Groef S, et al. Partial duct ligation: β-cell proliferation and beyond. Diabetes. 2014; 63:2567–77.
Article19. Cavelti-Weder C, Shtessel M, Reuss JE, Jermendy A, Yamada T, Caballero F, et al. Pancreatic duct ligation after almost complete β-cell loss: exocrine regeneration but no evidence of β-cell regeneration. Endocrinology. 2013; 154:4493–502.
Article20. Brown H, Sanger F, Kitai R. The structure of pig and sheep insulins. Biochem J. 1955; 60:556–65.
Article21. Sanger F. Chemistry of insulin: determination of the structure of insulin opens the way to greater understanding of life processes. Science. 1959; 129:1340–4.22. Walker J. Frederick Sanger (1918-2013). Nature. 2014; 505:27.
Article23. Howard JA. Dorothy Hodgkin and her contributions to biochemistry. Nat Rev Mol Cell Biol. 2003; 4:891–6.
Article24. Adams MJ, Blundell TL, Dodson EJ, Dodson GG, Vijayan M, Baker EN, et al. Structure of rhombohedral 2 zinc insulin crystals. Nature. 1969; 224:491–5.
Article25. Yalow RS, Berson SA. Assay of plasma insulin in human subjects by immunological methods. Nature. 1959; 184(Suppl 21):1648–9.
Article26. Yalow RS, Berson SA. Immunoassay of endogenous plasma insulin in man. J Clin Invest. 1960; 39:1157–75.
Article27. In memoriam: Dr. Rosalyn Yalow, PhD., 1921-2011. Mol Endocrinol. 2012; 26:713–4.28. Freychet P, Roth J, Neville DM Jr. Insulin receptors in the liver: specific binding of ( 125 I)insulin to the plasma membrane and its relation to insulin bioactivity. Proc Natl Acad Sci U S A. 1971; 68:1833–7.29. Cuatrecasas P. Affinity chromatography and purification of the insulin receptor of liver cell membranes. Proc Natl Acad Sci U S A. 1972; 69:1277–81.
Article30. Ullrich A, Shine J, Chirgwin J, Pictet R, Tischer E, Rutter WJ, et al. Rat insulin genes: construction of plasmids containing the coding sequences. Science. 1977; 196:1313–9.
Article31. Bell GI, Pictet RL, Rutter WJ, Cordell B, Tischer E, Goodman HM. Sequence of the human insulin gene. Nature. 1980; 284:26–32.
Article32. Ullrich A, Bell JR, Chen EY, Herrera R, Petruzzelli LM, Dull TJ, et al. Human insulin receptor and its relationship to the tyrosine kinase family of oncogenes. Nature. 1985; 313:756–61.
Article33. Ebina Y, Ellis L, Jarnagin K, Edery M, Graf L, Clauser E, et al. The human insulin receptor cDNA: the structural basis for hormone-activated transmembrane signalling. Cell. 1985; 40:747–58.
Article34. Taniguchi CM, Emanuelli B, Kahn CR. Critical nodes in signalling pathways: insights into insulin action. Nat Rev Mol Cell Biol. 2006; 7:85–96.
Article35. Saltiel AR. Insulin signaling in health and disease. J Clin Invest. 2021; 131:e142241.
Article36. Boucher J, Kleinridders A, Kahn CR. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb Perspect Biol. 2014; 6:a009191.
Article37. Hirsch IB, Juneja R, Beals JM, Antalis CJ, Wright EE. The evolution of insulin and how it informs therapy and treatment choices. Endocr Rev. 2020; 41:733–55.
Article38. Felig P. Landmark perspective: protamine insulin. Hagedorn’s pioneering contribution to drug delivery in the management of diabetes. JAMA. 1984; 251:393–6.
Article39. Scholtz HE, Pretorius SG, Wessels DH, Becker RH. Pharmacokinetic and glucodynamic variability: assessment of insulin glargine, NPH insulin and insulin ultralente in healthy volunteers using a euglycaemic clamp technique. Diabetologia. 2005; 48:1988–95.
Article40. Lindstrom T, Olsson PO, Arnqvist HJ. The use of human ultralente is limited by great intraindividual variability in overnight plasma insulin profiles. Scand J Clin Lab Invest. 2000; 60:341–7.41. Goeddel DV, Kleid DG, Bolivar F, Heyneker HL, Yansura DG, Crea R, et al. Expression in Escherichia coli of chemically synthesized genes for human insulin. Proc Natl Acad Sci U S A . 1979; 76:106–10.
Article42. Riggs AD. Making, cloning, and the expression of human insulin genes in bacteria: the path to Humulin. Endocr Rev. 2021; 42:374–80.
Article43. Koivisto VA. The human insulin analogue insulin lispro. Ann Med. 1998; 30:260–6.
Article44. Home PD. The pharmacokinetics and pharmacodynamics of rapid-acting insulin analogues and their clinical consequences. Diabetes Obes Metab. 2012; 14:780–8.
Article45. Bolli GB, Owens DR. Insulin glargine. Lancet. 2000; 356:443–5.
Article46. Barnett AH. Insulin glargine in the treatment of type 1 and type 2 diabetes. Vasc Health Risk Manag. 2006; 2:59–67.
Article47. Jonassen I, Havelund S, Hoeg-Jensen T, Steensgaard DB, Wahlund PO, Ribel U. Design of the novel protraction mechanism of insulin degludec, an ultra-long-acting basal insulin. Pharm Res. 2012; 29:2104–14.
Article48. Rosenstock J, Cheng A, Ritzel R, Bosnyak Z, Devisme C, Cali AMG, et al. More similarities than differences testing insulin glargine 300 units/mL versus insulin degludec 100 units/mL in insulin-naive type 2 diabetes: the randomized head-to-head BRIGHT Trial. Diabetes Care. 2018; 41:2147–54.
Article49. Garber AJ, King AB, Del Prato S, Sreenan S, Balci MK, Munoz-Torres M, et al. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 2 diabetes (BEGIN Basal-Bolus Type 2): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012; 379:1498–507.
Article50. Bolli GB, Riddle MC, Bergenstal RM, Ziemen M, Sestakauskas K, Goyeau H, et al. New insulin glargine 300 U/ml compared with glargine 100 U/ml in insulin-naïve people with type 2 diabetes on oral glucose-lowering drugs: a randomized controlled trial (EDITION 3). Diabetes Obes Metab. 2015; 17:386–94.
Article51. Wu T, Betty B, Downie M, Khanolkar M, Kilov G, Orr-Walker B, et al. Practical guidance on the use of premix insulin analogs in initiating, intensifying, or switching insulin regimens in type 2 diabetes. Diabetes Ther. 2015; 6:273–87.
Article52. Ross SA. Breaking down patient and physician barriers to optimize glycemic control in type 2 diabetes. Am J Med. 2013; 126(9 Suppl 1):S38–48.
Article53. Biester T, Kordonouri O, Danne T. Pharmacological properties of faster-acting insulin aspart. Curr Diab Rep. 2017; 17:101.
Article54. Russell-Jones D, Bode BW, De Block C, Franek E, Heller SR, Mathieu C, et al. Fast-acting insulin aspart improves glycemic control in basal-bolus treatment for type 1 diabetes: results of a 26-week multicenter, active-controlled, treat-to-target, randomized, parallel-group trial (onset 1). Diabetes Care. 2017; 40:943–50.
Article55. Bowering K, Case C, Harvey J, Reeves M, Sampson M, Strzinek R, et al. Faster aspart versus insulin aspart as part of a basal-bolus regimen in inadequately controlled type 2 diabetes: the onset 2 trial. Diabetes Care. 2017; 40:951–7.
Article56. Heise T, Linnebjerg H, Coutant D, LaBell E, Zijlstra E, Kapitza C, et al. Ultra rapid lispro lowers postprandial glucose and more closely matches normal physiological glucose response compared to other rapid insulin analogues: a phase 1 randomized, crossover study. Diabetes Obes Metab. 2020; 22:1789–98.
Article57. Blevins T, Zhang Q, Frias JP, Jinnouchi H, Chang AM; PRONTO-T2D Investigators. Randomized double-blind clinical trial comparing ultra rapid lispro with lispro in a basal-bolus regimen in patients with type 2 diabetes: PRONTO-T2D. Diabetes Care. 2020; 43:2991–8.
Article58. Klaff L, Cao D, Dellva MA, Tobian J, Miura J, Dahl D, et al. Ultra rapid lispro improves postprandial glucose control compared with lispro in patients with type 1 diabetes: results from the 26-week PRONTO-T1D study. Diabetes Obes Metab. 2020; 22:1799–807.59. Heise T, Meiffren G, Alluis B, Seroussi C, Ranson A, Arrubla J, et al. BioChaperone Lispro versus faster aspart and insulin aspart in patients with type 1 diabetes using continuous subcutaneous insulin infusion: a randomized euglycemic clamp study. Diabetes Obes Metab. 2019; 21:1066–70.
Article60. Andersen G, Meiffren G, Lamers D, DeVries JH, Ranson A, Seroussi C, et al. Ultra-rapid BioChaperone Lispro improves postprandial blood glucose excursions vs insulin lispro in a 14-day crossover treatment study in people with type 1 diabetes. Diabetes Obes Metab. 2018; 20:2627–32.
Article61. Bajaj HS, Bergenstal RM, Christoffersen A, Davies MJ, Gowda A, Isendahl J, et al. Switching to once-weekly insulin icodec versus once-daily insulin glargine U100 in type 2 diabetes inadequately controlled on daily basal insulin: a phase 2 randomized controlled trial. Diabetes Care. 2021; 44:1586–94.
Article62. Lingvay I, Buse JB, Franek E, Hansen MV, Koefoed MM, Mathieu C, et al. A randomized, open-label comparison of once-weekly insulin icodec titration strategies versus once-daily insulin glargine U100. Diabetes Care. 2021; 44:1595–603.
Article63. Rosenstock J, Bajaj HS, Janez A, Silver R, Begtrup K, Hansen MV, et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020; 383:2107–16.
Article64. Kjeldsen TB, Hubalek F, Hjorringgaard CU, Tagmose TM, Nishimura E, Stidsen CE, et al. Molecular engineering of insulin icodec, the first acylated insulin analog for once-weekly administration in humans. J Med Chem. 2021; 64:8942–50.
Article65. Heise T, Chien J, Beals J, Benson C, Klein O, Moyers JS, et al. Basal insulin Fc (BIF), a novel insulin suited for once weekly dosing for the treatment of patients with diabetes mellitus. J Endocr Soc. 2021; 5(Suppl 1):A329.
Article66. Kazda CM, Chien J, Zhang Q, Chigutsa E, Landschulz W, Wullenweber P, et al. 192-OR: Glycemic control with once-weekly basal insulin Fc (BIF) in persons with type 2 diabetes mellitus (T2DM) using continuous glucose monitoring (CGM) in a phase 2 study. Diabetes. 2021; 70(Suppl 1):192–OR.
Article67. Owens DR, Zinman B, Bolli G. Alternative routes of insulin delivery. Diabet Med. 2003; 20:886–98.
Article68. Heinemann L. The failure of exubera: are we beating a dead horse? J Diabetes Sci Technol. 2008; 2:518–29.
Article69. Mikhail N. Place of technosphere inhaled insulin in treatment of diabetes. World J Diabetes. 2016; 7:599–604.
Article70. Rosenstock J, Lorber DL, Gnudi L, Howard CP, Bilheimer DW, Chang PC, et al. Prandial inhaled insulin plus basal insulin glargine versus twice daily biaspart insulin for type 2 diabetes: a multicentre randomised trial. Lancet. 2010; 375:2244–53.
Article71. McGill JB, Peters A, Buse JB, Steiner S, Tran T, Pompilio FM, et al. Comprehensive pulmonary safety review of inhaled Technosphere® insulin in patients with diabetes mellitus. Clin Drug Investig. 2020; 40:973–83.72. Zijlstra E, Heinemann L, Plum-Morschel L. Oral insulin reloaded: a structured approach. J Diabetes Sci Technol. 2014; 8:458–65.73. Kumar V, Choudhry I, Namdev A, Mishra S, Soni S, Hurkat P, et al. Oral insulin: myth or reality. Curr Diabetes Rev. 2018; 14:497–508.
Article74. Gregory JM, Lautz M, Moore LM, Williams PE, Reddy P, Cherrington AD. Enterically delivered insulin tregopil exhibits rapid absorption characteristics and a pharmacodynamic effect similar to human insulin in conscious dogs. Diabetes Obes Metab. 2019; 21:160–9.
Article75. Eldor R, Arbit E, Corcos A, Kidron M. Glucose-reducing effect of the ORMD-0801 oral insulin preparation in patients with uncontrolled type 1 diabetes: a pilot study. PLoS One. 2013; 8:e59524.
Article76. Halberg IB, Lyby K, Wassermann K, Heise T, Zijlstra E, Plum-Morschel L. Efficacy and safety of oral basal insulin versus subcutaneous insulin glargine in type 2 diabetes: a randomised, double-blind, phase 2 trial. Lancet Diabetes Endocrinol. 2019; 7:179–88.
Article77. Abramson A, Caffarel-Salvador E, Khang M, Dellal D, Silverstein D, Gao Y, et al. An ingestible self-orienting system for oral delivery of macromolecules. Science. 2019; 363:611–5.
Article78. Farmer TD, Jenkins EC, O’Brien TP, McCoy GA, Havlik AE, Nass ER, et al. Comparison of the physiological relevance of systemic vs. portal insulin delivery to evaluate whole body glucose flux during an insulin clamp. Am J Physiol Endocrinol Metab. 2015; 308:E206–22.79. Jacober SJ, Prince MJ, Beals JM, Hartman ML, Qu Y, Linnebjerg H, et al. Basal insulin peglispro: overview of a novel longacting insulin with reduced peripheral effect resulting in a hepato-preferential action. Diabetes Obes Metab. 2016; 18 Suppl 2:3–16.
Article80. Riddle MC. Lessons from peglispro: IMAGINE how to improve drug development and affordability. Diabetes Care. 2016; 39:499–501.
Article81. Geho WB, Geho HC, Lau JR, Gana TJ. Hepatic-directed vesicle insulin: a review of formulation development and preclinical evaluation. J Diabetes Sci Technol. 2009; 3:1451–9.
Article82. Klonoff D, Bode B, Cohen N, Penn M, Geho WB, Muchmore DB. Divergent hypoglycemic effects of hepatic-directed prandial insulin: a 6-month phase 2b study in type 1 diabetes. Diabetes Care. 2019; 42:2154–7.
Article83. Jarosinski MA, Dhayalan B, Rege N, Chatterjee D, Weiss MA. ‘Smart’ insulin-delivery technologies and intrinsic glucose-responsive insulin analogues. Diabetologia. 2021; 64:1016–29.
Article84. Boughton CK, Hovorka R. New closed-loop insulin systems. Diabetologia. 2021; 64:1007–15.
Article85. Brown SA, Kovatchev BP, Raghinaru D, Lum JW, Buckingham BA, Kudva YC, et al. Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med. 2019; 381:1707–17.
Article86. Hoeg-Jensen T. Review: glucose-sensitive insulin. Mol Metab. 2021; 46:101107.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Insulin Sensitivity and Insulin Secretion Determined by Homeostasis Model Assessment and Future Risk of Diabetes Mellitus in Korean Men (Korean Diabetes J 32(6):498-505, 2008)
- Insulin Sensitivity and Insulin Secretion Determined by Homeostasis Model Assessment and Future Risk of Diabetes Mellitus in Korean Men (Korean Diabetes J 32(6):498-505, 2008)
- Intraoperative and Postoperative Glycemic Management in Patients with Diabetes
- Summary of Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
- Insulin Secretion and Insulin Sensitivity in Women with a Previous Gestational Diabetes: Understanding of Pathogenesis of Type 2 Diabetes