Ann Pediatr Endocrinol Metab.
2021 Sep;26(3):178-184. 10.6065/apem.2040208.104.
Single random measurement of urinary gonadotropin concentration for screening and monitoring girls with central precocious puberty
- Affiliations
-
- 1Department of Pediatrics, Chungnam National University Hospital, Daejeon, Korea
- 2Department of Laboratory Medicine, Chungnam National University College of Medicine, Daejeon, Korea
- 3Department of Pediatrics, Chungnam National University College of Medicine, Daejeon, Korea
- KMID: 2520510
- DOI: http://doi.org/10.6065/apem.2040208.104
Abstract
- Purpose
The gold standard for assessing pubertal activation is the gonadotropinreleasing hormone (GnRH) stimulation test (GnRHST), which is invasive, timeconsuming, and inconvenient. This study evaluated whether a single random measurement of urinary luteinizing hormone (LH) concentration could substitute for the GnRHST in diagnosing and monitoring central precocious puberty (CPP) in girls.
Methods
Fifty-five girls with breast buds before 8 years of age were assessed by both the GnRHST and urinary gonadotropin assays. Based on the GnRHST results, 29 girls were assigned to the CPP group (peak LH≥5 IU/L), and 26 were placed in the premature thelarche (PT) group (peak LH<5 IU/L). Auxological data and urine and serum samples were collected at baseline and after treatment with a GnRH agonist for 12 and 24 weeks.
Results
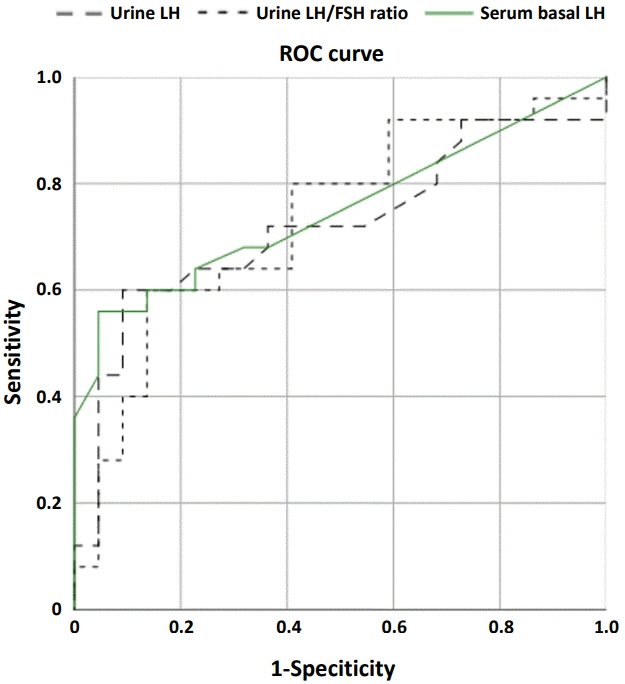
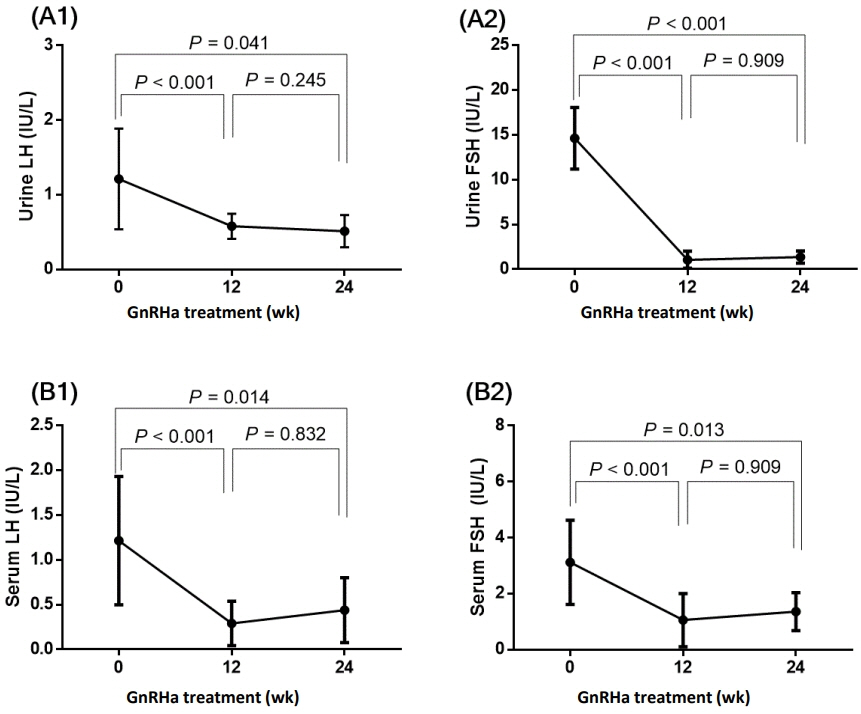
Although the auxological data did not differ between the 2 groups, the serum levels of insulin-like growth factor-1, basal LH, follicle-stimulating hormone (FSH), estradiol, and peak LH; urinary LH; and peak serum LH/FSH and urinary LH/FSH ratios were higher in the CPP group than in the PT group. Pearson correlation analysis showed a positive correlation between the urinary and serum LH concentrations (r=0.660, P<0.001). Receiver-operating characteristic curve analyses showed that a urinary LH concentration of 0.725 IU/L was a cutoff that significantly predicted positivity on the GnRHST. Urinary LH and FSH concentrations declined significantly during GnRH agonist treatment.
Conclusion
A single, random measurement of urinary gonadotropin concentration could be a reliable tool for initial screening and therapeutic monitoring of CPP in girls.
Figure
Cited by 1 articles
-
Commentary on "Single random measurement of urinary gonadotropin concentration for screening and monitoring girls with central precocious puberty"
Ahreum Kwon
Ann Pediatr Endocrinol Metab. 2021;26(3):136-137. doi: 10.6065/apem.2120104edi01.
Reference
-
References
1. Leka-Emiri S, Chrousos GP, Kanaka-Gantenbein C. The mystery of puberty initiation: genetics and epigenetics of idiopathic central precocious puberty (ICPP). J Endocrinol Invest. 2017; 40:789–802.
Article2. Cantas-Orsdemir S, Eugster EA. Update on central precocious puberty: from etiologies to outcomes. Expert Rev Endocrinol Metab. 2019; 14:123–30.
Article3. Juul A, Hagen CP, Aksglaede L, Sørensen K, Mouritsen A, Frederiksen H, et al. Endocrine evaluation of reproductive function in girls during infancy, childhood and adolescence. Endocr Dev. 2012; 22:24–39.
Article4. Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev. 2003; 24:668–93.
Article5. Demir A, Voutilainen R, Stenman UH, Dunkel L, Albertsson-Wikland K, Norjavaara E. First Morning Voided Urinary Gonadotropin Measurements as an Alternative to the GnRH Test. Horm Res Paediatr. 2016; 85:301–8.
Article6. Kletter GB, Klein KO, Wong YY. A pediatrician's guide to central precocious puberty. Clin Pediatr (Phila). 2015; 54:414–24.
Article7. Witchel SF, Baens-Bailon RG, Lee PA. Treatment of central precocious puberty: comparison of urinary gonadotropin excretion and gonadotropin-releasing hormone (GnRH) stimulation tests in monitoring GnRH analog therapy. J Clin Endocrinol Metab. 1996; 81:1353–6.
Article8. Kim HK, Kee SJ, Seo JY, Yang EM, Chae HJ, Kim CJ. Gonadotropin-releasing hormone stimulation test for precocious puberty. Korean J Lab Med. 2011; 31:244–9.
Article9. Houk CP, Kunselman AR, Lee PA. The diagnostic value of a brief GnRH analogue stimulation test in girls with central precocious puberty: a single 30-minute post-stimulation LH sample is adequate. J Pediatr Endocrinol Metab. 2008; 21:1113–8.
Article10. McNeilly JD, Mason A, Khanna S, Galloway PJ, Ahmed SF. Urinary gonadotrophins: a useful non-invasive marker of activation of the hypothalamic pituitary-gonadal axis. Int J Pediatr Endocrinol. 2012; 2012:10.
Article11. Buckler JM, Clayton BE. Output of luteinizing hormone in the urine of normal children and those with advanced sexual development. Arch Dis Child. 1970; 45:478–84.
Article12. Zung A, Burundukov E, Ulman M, Glaser T, Rosenberg M, Chen M, et al. The diagnostic value of first-voided urinary LH compared with GNRH-stimulated gonadotropins in differentiating slowly progressive from rapidly progressive precocious puberty in girls. Eur J Endocrinol. 2014; 170:749–58.
Article13. Korea Centers for Disease Control and Prevention, Division of Health and Nutrition Survey; Korean Pediatric Society, Committee for School Health and Public Health Statistics; Committee for the Development of Growth Standards for Korean Children and Adolescents. 2017 Korean National Growth Charts for children and adolescents. Cheongju (Korea): Korea Centers for Disease Control and Prevention;2017.14. Houk CP, Kunselman AR, Lee PA. Adequacy of a single unstimulated luteinizing hormone level to diagnose central precocious puberty in girls. Pediatrics. 2009; 123:e1059–63.
Article15. Resende EA, Lara BH, Reis JD, Ferreira BP, Pereira GA, Borges MF. Assessment of basal and gonadotropinreleasing hormone-stimulated gonadotropins by immunochemiluminometric and immunofluorometric assays in normal children. J Clin Endocrinol Metab. 2007; 92:1424–9.
Article16. Kandemir N, Demirbilek H, Özön ZA, Gönç N, Alikaşifoğlu A. GnRH stimulation test in precocious puberty: single sample is adequate for diagnosis and dose adjustment. J Clin Res Pediatr Endocrinol. 2011; 3:12–7.
Article17. Cavallo A, Richards GE, Busey S, Michaels SE. A simplified gonadotrophin-releasing hormone test for precocious puberty. Clin Endocrinol (Oxf). 1995; 42:641–6.
Article18. Kim MS, Hwang PH, Lee DY. A gonadotropin-releasing hormone (GnRH) stimulation test before and after GnRH analogue treatment for central precocious puberty: has the GnRH test been adequately simplified? Indian J Pediatr. 2015; 82:996–1000.
Article19. Becker KL, Albert A. Urinary excretion of follicle-stimulating and luteinizing hormones. J Clin Endocrinol Metab. 1965; 25:962–74.
Article20. Andersen RN, Albert A. S eparable urinar y LH by carboxymethylcellulose chromatography. Endocrinology. 1965; 77:1085–90.
Article21. Courant F, Aksglaede L, Antignac JP, Monteau F, Sorensen K, Andersson AM, et al. Assessment of circulating sex steroid levels in prepubertal and pubertal boys and girls by a novel ultrasensitive gas chromatography-tandem mass spectrometry method. J Clin Endocrinol Metab. 2010; 95:82–92.
Article22. Singh GK, Balzer BW, Kelly PJ, Paxton K, Hawke CI, Handelsman DJ, et al. Urinary sex steroids and anthropometric markers of pub er ty - a novel approach to characterising within-person changes of puberty hormones. PLoS One. 2015; 10:e0143555.23. Fitschen W, Clayton BE. Urinary excretion of gonadotrophins with particular reference to children. Arch Dis Child. 1965; 40:16–26.
Article24. Maesaka H, Tachibana K, Adachi M, Okada T. Monthly urinary gonadotropin and ovarian hormone excretory patterns in normal girls and female patients with idiopathic precocious puberty. Pediatr Res. 1996; 40:853–60.
Article25. Lucaccioni L, McNeilly J, Mason A, Giacomozzi C, Kyriakou A, Shaikh MG, et al. The measurement of urinary gonadotropins for assessment and management of pubertal disorder. Hormones (Athens). 2016; 15:377–84.
Article26. Singh GK, Balzer BW, Desai R, Jimenez M, Steinbeck KS, Handelsman DJ. Requirement for specific gravity and creatinine adjustments for urinary steroids and luteinizing hormone concentrations in adolescents. Ann Clin Biochem. 2015; 52:665–71.
Article27. Demir A, Dunkel L, Stenman UH, Voutilainen R. Agerelated course of urinary gonadotropins in children. J Clin Endocrinol Metab. 1995; 80:1457–60.
Article28. Ye X, Wong LY, Bishop AM, Calafat AM. Variability of urinary concentrations of bisphenol A in spot samples, first morning voids, and 24-hour collections. Environ Health Perspect. 2011; 119:983–8.
Article29. Yüce Ö, Bideci A, Ç elik N, Ç amurdan O, Cinaz P. Diagnostic value of urinary luteinizing hormone levels in the monitoring of precocious puberty treatment. Arch Endocrinol Metab. 2020; 64:121–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Commentary on "Single random measurement of urinary gonadotropin concentration for screening and monitoring girls with central precocious puberty"
- Diagnosis and Treatment of Central Precocious Puberty
- Etiology and Age Incidence of Precocious Puberty
- Indication of Gonadotropin-Releasing Hormone Agonist: Precocious Puberty or Advanced Puberty?
- Two Cases of Secondary Central Precocious Puberty in Boys with Congenital Adrenal Hyperplasia - before and after Treatment with Corticosteroid