J Korean Neurosurg Soc.
2021 Sep;64(5):837-842. 10.3340/jkns.2020.0293.
A Concomitant Occurrence of the Atlantoaxial Subluxation with Rare Vertebral Formation and Segmentation Defects
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea
- KMID: 2519711
- DOI: http://doi.org/10.3340/jkns.2020.0293
Abstract
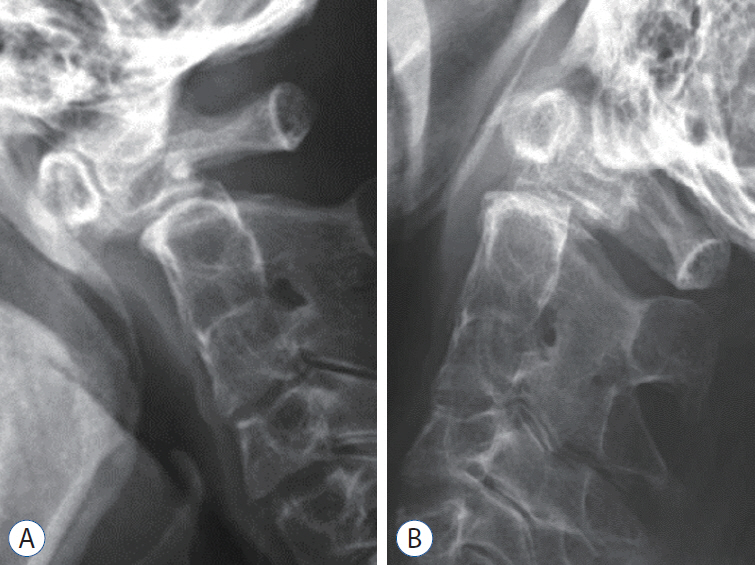
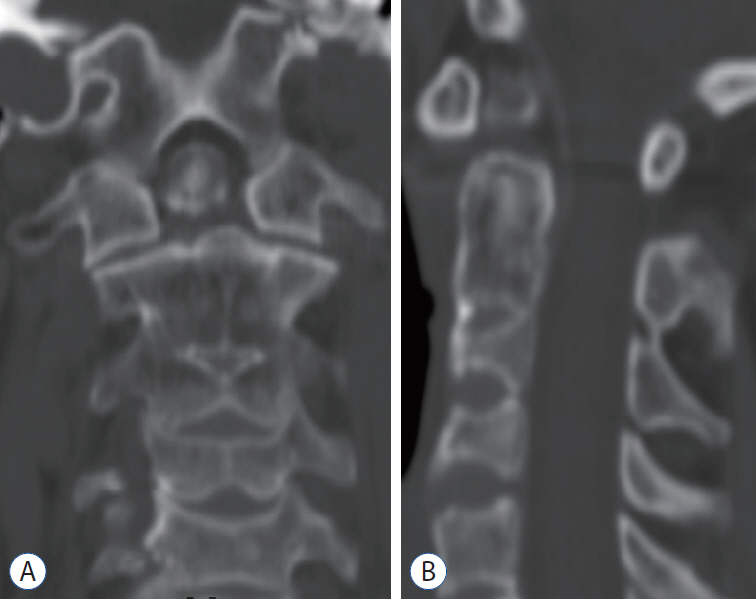
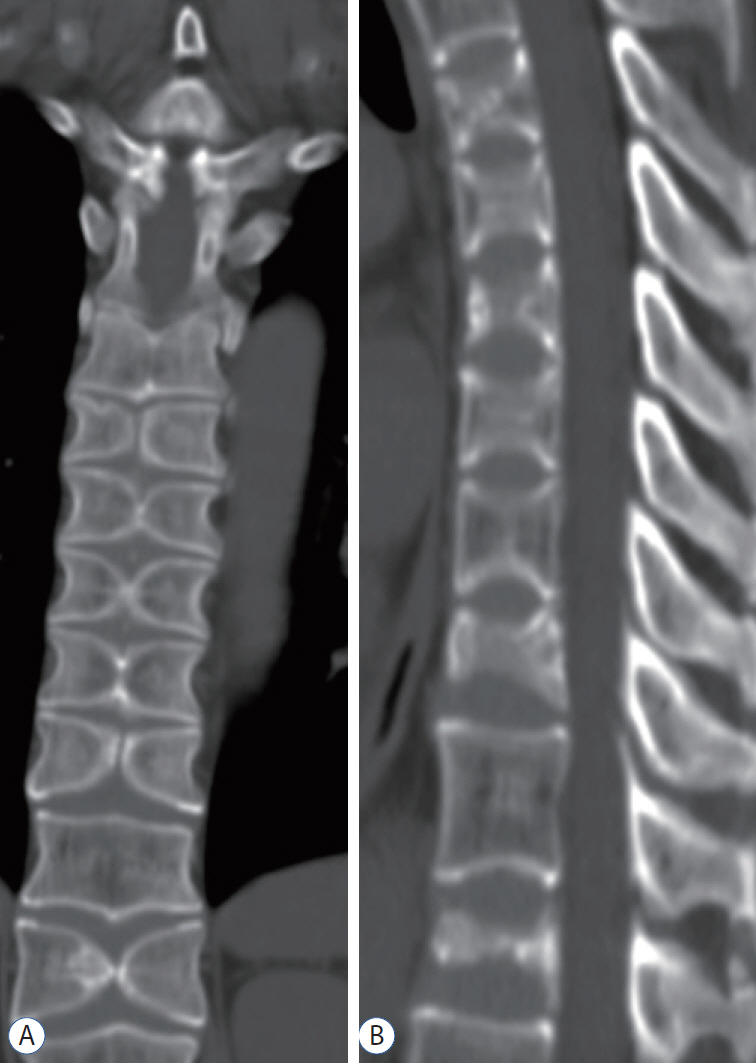
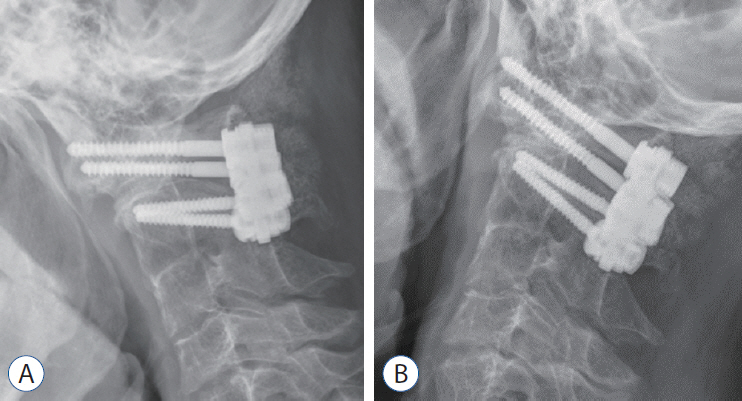
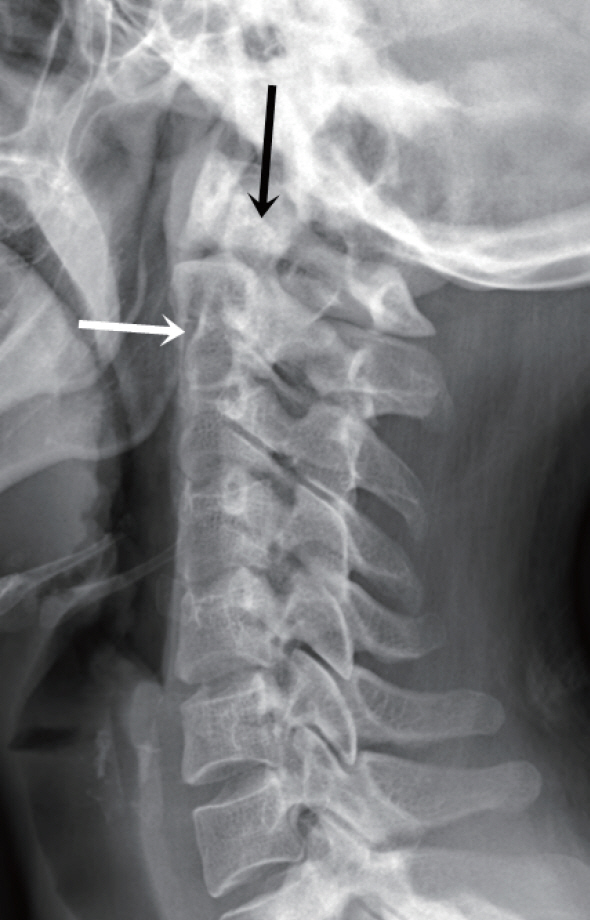
- An atlantoaxial subluxation from the unstable Os odontoideum by the failure of proper integrations between the embryological somites might be a commonly reported pathology. However, its suspicious origin or paralleled occurrence with other congenital anomalies of vertebral body might be a relatively rare phenomenon. The authors present two cases, who simply presented with clinical signs of prolonged, intractable cervicalgia without any neurological deficits, revealed this rare feature of C1–2 subluxation from the unstable, orthotropic type of Os odontoideum that coincide with congenitally fused cervical vertebral bodies between C2–3. Surprisingly, in one case, when traced from the lower cervical down to the thoracic-lumbar levels during the preoperative work-up process, was also compromised with multi-level butterfly vertebrae formations. Presented cases highlight the association of various congenital vertebrae anomalies and the rationale to fuse only affected joints.
Figure
Reference
-
References
1. Cave P. Butterfly vertebra. Br J Radiol. 31:503–506. 1958.
Article2. Colquhoun J. Butterfly vertebra or sagittal cleft vertebra. Am J Orthop Surg. 10:44–50. 1968.3. Deepak AN, Salunke P, Kamble RP. Case of atlantoaxial dislocation with assimilated C1, absent posterior C2, butterfly C3, and fused subaxial cervical spine: management dilemma with multiple segmentation and formation defects. J Pediatr Neurosci. 12:72–74. 2017.
Article4. Gray SW, Romaine CB, Skandalakis JE. Congenital fusion of the cervical vertebrae. Surg Gynecol Obstet. 118:373–385. 1964.5. Jain N, Verma R, Garga UC, Baruah BP, Jain SK, Bhaskar SN. CT and MR imaging of odontoid abnormalities: a pictorial review. Indian J Radiol Imaging. 26:108–119. 2016.
Article6. Katsuura Y, Kim HJ. Butterfly vertebrae: a systematic review of the literature and analysis. Global Spine J. 9:666–679. 2019.
Article7. McRae DL, Barnum AS. Occipitalization of the atlas. Am J Roentgenol Radium Ther Nucl Med. 70:23–46. 1953.8. Müller F, O’Rahilly R, Benson DR. The early origin of vertebral anomalies, as illustrated by a ‘butterfly vertebra’. J Anat. 149:157–169. 1986.9. Pang D, Thompson DN. Embryology and bony malformations of the craniovertebral junction. Childs Nerv Syst. 27:523–564. 2011.
Article10. Patcas R, Tausch D, Pandis N, Manestar M, Ullrich O, Karlo CA, et al. Illusions of fusions: assessing cervical vertebral fusion on lateral cephalograms, multidetector computed tomographs, and cone-beam computed tomographs. Am J Orthod Dentofacial Orthop. 143:213–220. 2013.
Article11. Patinharayil G, Han CW, Marthya A, Meethall KC, Surendran S, Rudrappa GH. Butterfly vertebra: an uncommon congenital spinal anomaly. Spine (Phila Pa 1976). 33:E926–E928. 2008.12. Patra DP, Salunke P, Pramanick G. Butterfly C2 vertebra: an unusual finding in a case of os odontoideum. Pediatr Neurosurg. 49:320–323. 2013.
Article13. Salunke P, Behari S, Kirankumar MV, Sharma MS, Jaiswal AK, Jain VK. Pediatric congenital atlantoaxial dislocation: differences between the irreducible and reducible varieties. J Neurosurg. 104(2 Suppl):115–122. 2006.
Article14. Salunke P, Sharma M, Sodhi HB, Mukherjee KK, Khandelwal NK. Congenital atlantoaxial dislocation: a dynamic process and role of facets in irreducibility. J Neurosurg Spine. 15:678–685. 2011.
Article15. Shah A, Kaswa A, Jain S, Goel A. Atlantoaxial instability associated with pan cervical vertebral fusion: report on management of 4 cases. Neurol India. 66:147–150. 2018.
Article16. Smoker WR. Congenital anomalies of the cervical spine. Neuroimaging Clin N Am. 5:427–449. 1995.17. Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 4:197–210. 2014.
Article18. Yin HF, Yang KQ, Lou SQ. Clinical significance of congenital fusion of cervical vertebrae: a report of 87 cases. Zhonghua Wai Ke Za Zhi. 27:75–124. 75-77, 124. 1989.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atlantoaxial Fixation using Rod and Screw for Bilateral High-riding Vertebral Artery
- Old Atlantoaxial Rotary Subluxation Associated with High-riding Vertebral Arteries: Arthrodesis Using C1 Lateral Mass Screws and C2 Laminar Screws: A Case Report
- Congenital Anomaly of the Atlas Misdiagnosed as Posterior Arch Fracture of the Atlas and Atlantoaxial Subluxation
- Atlantoaxial Subluxation due to Psoriatic Arthritis
- C1-2 Instability associated with Duplicated Vertebral Artery: A Case Report