Korean J Physiol Pharmacol.
2021 Sep;25(5):459-466. 10.4196/kjpp.2021.25.5.459.
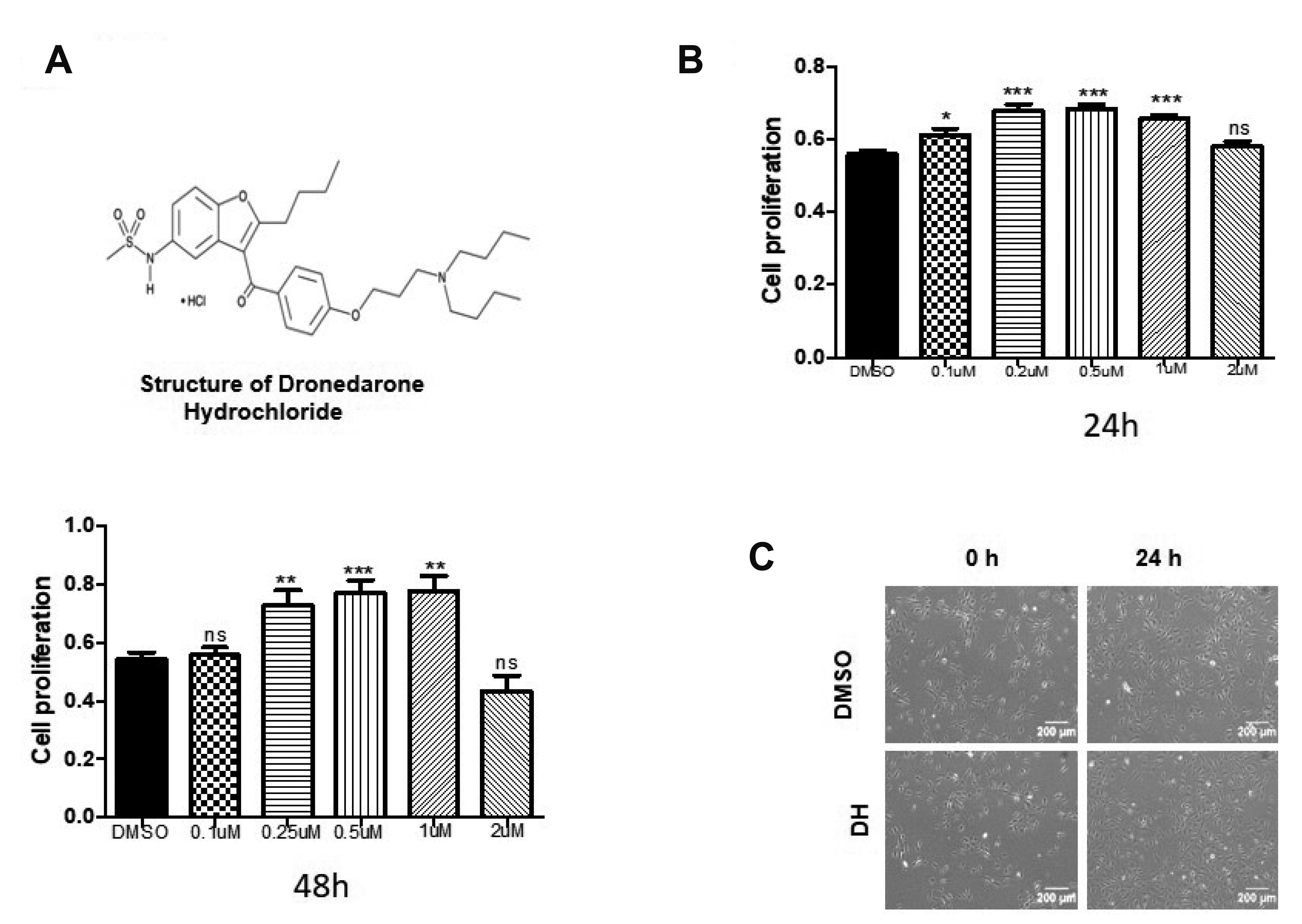
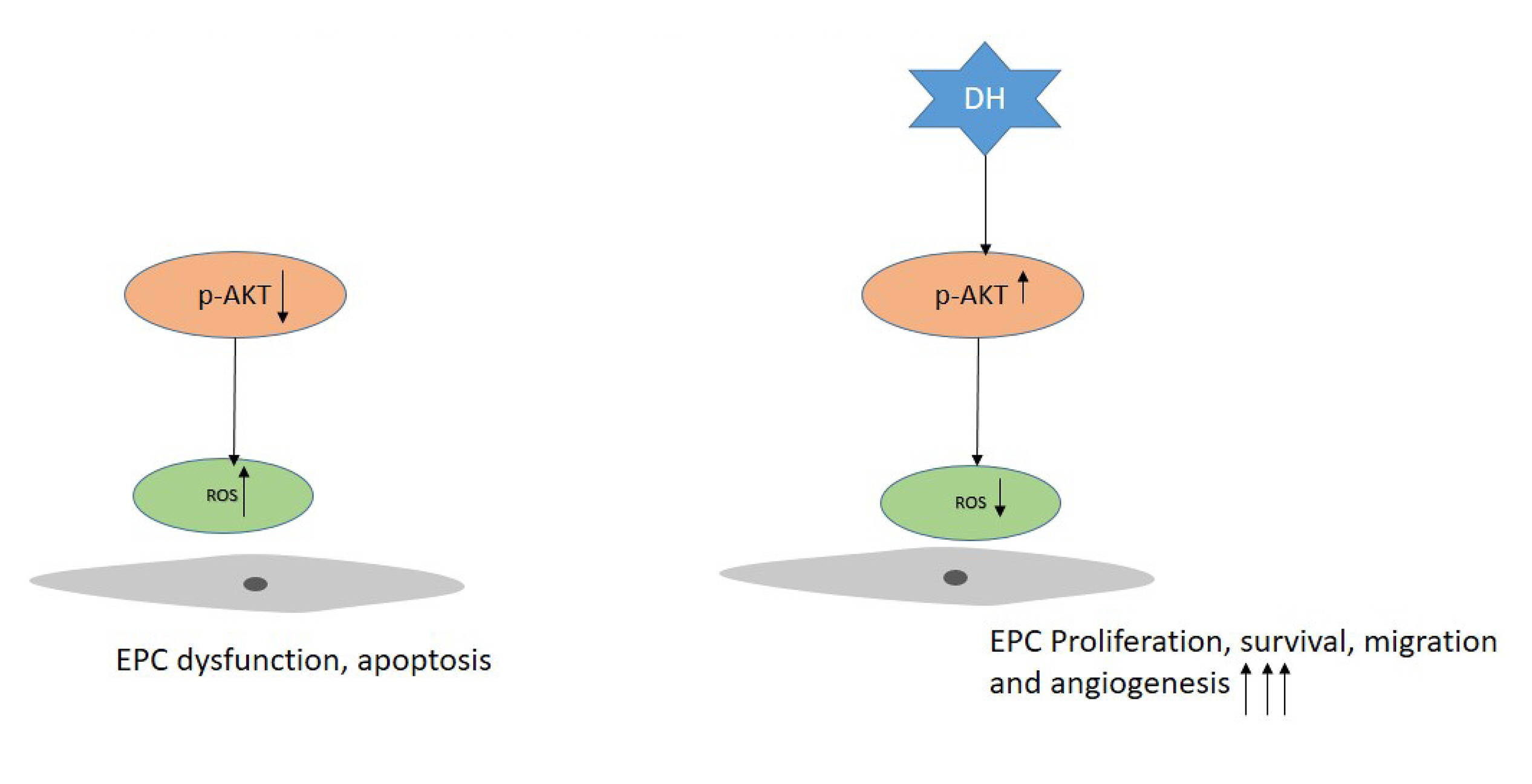
Dronedarone hydrochloride enhances the bioactivity of endothelial progenitor cells via regulation of the AKT signaling pathway
- Affiliations
-
- 1Laboratory for Vascular Medicine and Stem Cell Biology, Research Institute of Convergence Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan 50612, Korea.
- 2Department of Molecular Biology, Pusan National University, Busan 46241, Korea.
- 3Department of Physiology, School of Medicine, Pusan National University, Yangsan 50612, Korea.
- KMID: 2519408
- DOI: http://doi.org/10.4196/kjpp.2021.25.5.459
Abstract
- Cardiovascular disease (CVD) and its complications are the leading cause of morbidity and mortality in the world. Because of the side effects and incomplete recovery from current therapy, stem cell therapy emerges as a potential therapy for CVD treatment, and endothelial progenitor cell (EPC) is one of the key stem cells used for therapeutic applications. The effect of this therapy required the expansion of EPC function. To enhance the EPC activation, proliferation, and angiogenesis using dronedarone hydrochloride (DH) is the purpose of this study. DH received approval for atrial fibrillation treatment and its cardiovascular protective effects were already reported. In this study, DH significantly increased EPC proliferation, tube formation, migration, and maintained EPCs surface marker expression. In addition, DH treatment up-regulated the phosphorylation of AKT and reduced the reactive oxygen species production. In summary, the cell priming by DH considerably improved the functional activity of EPCs, and the use of which might be a novel strategy for CVD treatment.
Figure
Reference
-
1. Cully M. 2017; Cardiovascular disease: BET inhibitor attenuates heart failure. Nat Rev Drug Discov. 16:453. DOI: 10.1038/nrd.2017.125. PMID: 28660902.2. Dimmeler S. 2011; Cardiovascular disease review series. EMBO Mol Med. 3:697. DOI: 10.1002/emmm.201100182. PMID: 22113984. PMCID: PMC3377116.
Article3. Kuehn BM. 2019; Sleep duration linked to cardiovascular disease. Circulation. 139:2483–2484. DOI: 10.1161/CIRCULATIONAHA.119.041278. PMID: 31107620.
Article4. Yoshida Y, Yamanaka S. 2010; Recent stem cell advances: induced pluripotent stem cells for disease modeling and stem cell-based regeneration. Circulation. 122:80–87. DOI: 10.1161/CIRCULATIONAHA.109.881433. PMID: 20606130.
Article5. Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. 1997; Isolation of putative progenitor endothelial cells for angiogenesis. Science. 275:964–967. DOI: 10.1126/science.275.5302.964. PMID: 9020076.
Article6. Sen S, McDonald SP, Coates PT, Bonder CS. 2011; Endothelial progenitor cells: novel biomarker and promising cell therapy for cardiovascular disease. Clin Sci (Lond). 120:263–283. DOI: 10.1042/CS20100429. PMID: 21143202.
Article7. Zhao T, Li J, Chen AF. 2010; MicroRNA-34a induces endothelial progenitor cell senescence and impedes its angiogenesis via suppressing silent information regulator 1. Am J Physiol Endocrinol Metab. 299:E110–E116. DOI: 10.1152/ajpendo.00192.2010. PMID: 20424141. PMCID: PMC2904051.
Article8. Dimmeler S, Burchfield J, Zeiher AM. 2008; Cell-based therapy of myocardial infarction. Arterioscler Thromb Vasc Biol. 28:208–216. DOI: 10.1161/ATVBAHA.107.155317. PMID: 17951319.
Article9. Shintani S, Murohara T, Ikeda H, Ueno T, Honma T, Katoh A, Sasaki K, Shimada T, Oike Y, Imaizumi T. 2001; Mobilization of endothelial progenitor cells in patients with acute myocardial infarction. Circulation. 103:2776–2779. DOI: 10.1161/hc2301.092122. PMID: 11401930.
Article10. Lee JH, Lee SH, Choi SH, Asahara T, Kwon SM. 2015; The sulfated polysaccharide fucoidan rescues senescence of endothelial colony-forming cells for ischemic repair. Stem Cells. 33:1939–1951. DOI: 10.1002/stem.1973. PMID: 25693733.
Article11. Naccarelli GV, Wolbrette DL, Levin V, Samii S, Banchs JE, Penny-Peterson E, Gonzalez MD. 2011; Safety and efficacy of dronedarone in the treatment of atrial fibrillation/flutter. Clin Med Insights Cardiol. 5:103–119. DOI: 10.4137/CMC.S6677. PMID: 22084608. PMCID: PMC3201110.
Article12. Sun W, Sarma JS, Singh BN. 1999; Electrophysiological effects of dronedarone (SR33589), a noniodinated benzofuran derivative, in the rabbit heart: comparison with amiodarone. Circulation. 100:2276–2281. DOI: 10.1161/01.CIR.100.22.2276. PMID: 10578003.13. Sun W, Sarma JS, Singh BN. 2002; Chronic and acute effects of dronedarone on the action potential of rabbit atrial muscle preparations: comparison with amiodarone. J Cardiovasc Pharmacol. 39:677–684. DOI: 10.1097/00005344-200205000-00008. PMID: 11973411.
Article14. Pisters R, Hohnloser SH, Connolly SJ, Torp-Pedersen C, Naditch-Brûlé L, Page RL, Crijns HJ. 2014; Effect of dronedarone on clinical end points in patients with atrial fibrillation and coronary heart disease: insights from the ATHENA trial. Europace. 16:174–181. DOI: 10.1093/europace/eut293. PMID: 24072451. PMCID: PMC3905706.
Article15. Hohnloser SH, Crijns HJ, van Eickels M, Gaudin C, Page RL, Torp-Pedersen C, Connolly SJ. 2009; Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med. 360:668–678. DOI: 10.1056/NEJMoa0803778. PMID: 19213680.
Article16. Hur J, Yoon CH, Lee CS, Kim TY, Oh IY, Park KW, Kim JH, Lee HS, Kang HJ, Chae IH, Oh BH, Park YB, Kim HS. 2007; Akt is a key modulator of endothelial progenitor cell trafficking in ischemic muscle. Stem Cells. 25:1769–1778. DOI: 10.1634/stemcells.2006-0385. PMID: 17412896.
Article17. Kim YJ, Ji ST, Kim DY, Jung SY, Kang S, Park JH, Jang WB, Yun J, Ha J, Lee DH, Kwon SM. 2018; Long-term priming by three small molecules is a promising strategy for enhancing late endothelial progenitor cell bioactivities. Mol Cells. 41:582–590. DOI: 10.14348/molcells.2018.0011. PMID: 29890822. PMCID: PMC6030238.18. Laplante M, Sabatini DM. 2012; mTOR signaling in growth control and disease. Cell. 149:274–293. DOI: 10.1016/j.cell.2012.03.017. PMID: 22500797. PMCID: PMC3331679.
Article19. Rethineswaran VK, Kim YJ, Jang WB, Ji ST, Kang S, Kim DY, Park JH, Van LTH, Giang LTT, Ha JS, Yun J, Lee DH, Yu SN, Park SG, Ahn SC, Kwon SM. 2019; Enzyme-aided extraction of fucoidan by AMG augments the functionality of EPCs through regulation of the AKT/Rheb signaling pathway. Mar Drugs. 17:392. DOI: 10.3390/md17070392. PMID: 31277207. PMCID: PMC6669526.
Article20. Adler V, Yin Z, Tew KD, Ronai Z. 1999; Role of redox potential and reactive oxygen species in stress signaling. Oncogene. 18:6104–6111. DOI: 10.1038/sj.onc.1203128. PMID: 10557101.
Article21. Lander HM, Milbank AJ, Tauras JM, Hajjar DP, Hempstead BL, Schwartz GD, Kraemer RT, Mirza UA, Chait BT, Burk SC, Quilliam LA. 1996; Redox regulation of cell signalling. Nature. 381:380–381. DOI: 10.1038/381380a0. PMID: 8632794.
Article22. Fleissner F, Thum T. 2011; Critical role of the nitric oxide/reactive oxygen species balance in endothelial progenitor dysfunction. Antioxid Redox Signal. 15:933–948. DOI: 10.1089/ars.2010.3502. PMID: 20712407. PMCID: PMC3135185.
Article23. Kawamoto A, Asahara T, Losordo DW. 2002; Transplantation of endothelial progenitor cells for therapeutic neovascularization. Cardiovasc Radiat Med. 3:221–225. DOI: 10.1016/S1522-1865(03)00082-9. PMID: 12974378.
Article24. Alev C, Ii M, Asahara T. 2011; Endothelial progenitor cells: a novel tool for the therapy of ischemic diseases. Antioxid Redox Signal. 15:949–965. DOI: 10.1089/ars.2010.3872. PMID: 21254837.
Article25. Kawamoto A, Asahara T. 2007; Role of progenitor endothelial cells in cardiovascular disease and upcoming therapies. Catheter Cardiovasc Interv. 70:477–484. DOI: 10.1002/ccd.21292. PMID: 17894361.
Article26. Lamichane S, Baek SH, Kim YJ, Park JH, Dahal Lamichane B, Jang WB, Ji S, Lee NK, Dehua L, Kim DY, Kang S, Seong HJ, Yun J, Lee DH, Moon HR, Chung HY, Kwon SM. 2019; MHY2233 attenuates replicative cellular senescence in human endothelial progenitor cells via SIRT1 signaling. Oxid Med Cell Longev. 2019:6492029. DOI: 10.1155/2019/6492029. PMID: 31223423. PMCID: PMC6556284.
Article27. Incalza MA, D'Oria R, Natalicchio A, Perrini S, Laviola L, Giorgino F. 2018; Oxidative stress and reactive oxygen species in endothelial dysfunction associated with cardiovascular and metabolic diseases. Vascul Pharmacol. 100:1–19. DOI: 10.1016/j.vph.2017.05.005. PMID: 28579545.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- miR-450a-5p Eliminates MGO-Induced Insulin Resistance via Targeting CREB
- Inhibition of the interaction between Hippo/YAP and Akt signaling with ursolic acid and 3′3-diindolylmethane suppresses esophageal cancer tumorigenesis
- Neuroprotection Signaling of Nuclear Akt in Neuronal Cells
- IGF-I Exerts an Anti-inflammatory Effect on Skeletal Muscle Cells through Down-regulation of TLR4 Signaling
- Hsp20 Promotes Endothelial Progenitor Cell Angiogenesis via Activation of PI3K/Akt Signaling Pathway under Hypoxia