Clin Exp Otorhinolaryngol.
2021 Aug;14(3):347-354. 10.21053/ceo.2020.02257.
Type 2 Diabetes Mellitus Increases Peritonsillar Abscess Susceptibility: Real-World Evidence
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 2Department of Otolaryngology-Head and Neck Surgery, Chang Gung Memorial Hospital, Chiayi, Taiwan
- 3Health Information and Epidemiology Laboratory of Chang Gung Memorial Hospital, Chiayi, Taiwan
- 4Graduate Institute of Clinical Medical Sciences, College of Medicine, Chang Gung University, Taoyuan, Taiwan
- 5Faculty of Medicine, College of Medicine, Chang Gung University, Taoyuan, Taiwan
- 6Department of Traditional Chinese Medicine, Chang Gung Memorial Hospital, Chiayi, Taiwan
- 7School of Traditional Chinese Medicine, College of Medicine, Chang Gung University, Taoyuan, Taiwan
- KMID: 2519190
- DOI: http://doi.org/10.21053/ceo.2020.02257
Abstract
Objectives
. Type 2 diabetes mellitus (T2DM) is a risk factor for deep neck infection (DNI) and leads to complications and poor outcomes. Our study aimed to investigate the risk, prognosis, and complications of peritonsillar abscess (PTA) in patients with T2DM.
Methods
. We extracted data of patients newly diagnosed as having T2DM between January 2000 and December 2011 from Taiwan’s National Health Insurance Research Database. These patients were matched with patients without T2DM, and PTA incidence was compared between both cohorts.
Results
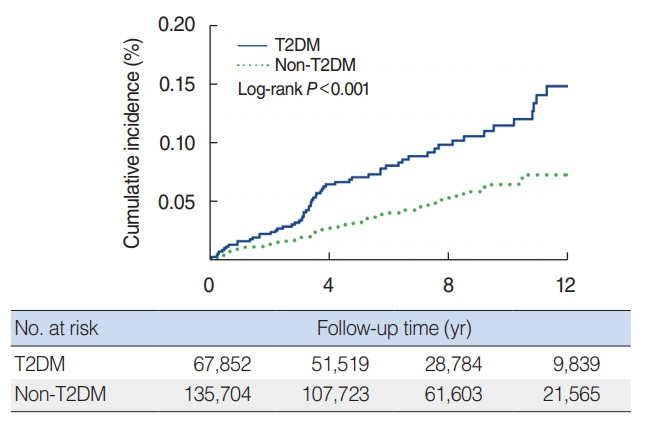
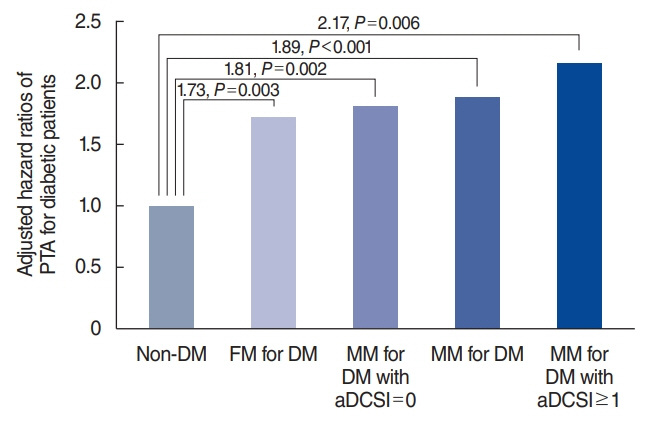
. In total, 67,852 patients with and 135,704 patients without T2DM were enrolled. PTA incidence was significantly higher in patients with T2DM (incidence rate ratio, 1.91; P<0.001); moreover, PTA incidence was higher at 1 to 5 years after T2DM diagnosis than at <1 and >5 years after T2DM diagnosis. Cox regression analysis showed that patients with T2DM had an approximately 2-fold higher PTA risk (adjusted hazard ratio [aHR]: 1.89, P<0.001). Patients with a higher adapted Diabetes Complications Severity Index (aDCSI) had higher PTA risk than those with a lower aDCSI (aHRs: 2.17 for aDCSI ≥1, P=0.006 and 1.81 for aDCSI=0, P=0.002). T2DM patients with a high aDCSI (≥1) had a nonsignificantly longer hospitalization duration and a higher rate of DNI complications than did those with a low aDCSI (=0).
Conclusion
. In patients with T2DM, PTA incidence was relatively high, and it increased with T2DM severity. Moreover, T2DM patients should be particularly careful about PTA within 1 to 5 years after the diagnosis, and physicians should keep in mind that the prognosis of PTA was correlated with T2DM severity.
Keyword
Figure
Reference
-
1. Klug TE, Rusan M, Fuursted K, Ovesen T. Peritonsillar abscess: complication of acute tonsillitis or Weber’s glands infection. Otolaryngol Head Neck Surg. 2016; Aug. 155(2):199–207.2. Galioto NJ. Peritonsillar abscess. Am Fam Physician. 2017; Apr. 95(8):501–6.3. Powell J, Wilson JA. An evidence-based review of peritonsillar abscess. Clin Otolaryngol. 2012; Apr. 37(2):136–45.
Article4. Chang GH, Ding MC, Chen YC, Yang YH, Liu CY, Chang PJ, et al. Real-world evidence for increased deep neck infection risk in patients with rheumatoid arthritis. Laryngoscope. 2020; Jun. 130(6):1402–7.
Article5. Tsai MS, Chang GH, Chen WM, Liu CY, Lin MH, Chang PJ, et al. The association between decompensated liver cirrhosis and deep neck infection: real-world evidence. Int J Environ Res Public Health. 2019; Oct. 16(20):3863.
Article6. Ridder GJ, Technau-Ihling K, Sander A, Boedeker CC. Spectrum and management of deep neck space infections: an 8-year experience of 234 cases. Otolaryngol Head Neck Surg. 2005; Nov. 133(5):709–14.7. Huang TT, Liu TC, Chen PR, Tseng FY, Yeh TH, Chen YS. Deep neck infection: analysis of 185 cases. Head Neck. 2004; Oct. 26(10):854–60.
Article8. Huang TT, Tseng FY, Liu TC, Hsu CJ, Chen YS. Deep neck infection in diabetic patients: comparison of clinical picture and outcomes with nondiabetic patients. Otolaryngol Head Neck Surg. 2005; Jun. 132(6):943–7.
Article9. Chang GH, Ding MC, Yang YH, Lin YH, Liu CY, Lin MH, et al. High risk of deep neck infection in patients with type 1 diabetes mellitus: a nationwide population-based cohort study. J Clin Med. 2018; Oct. 7(11):385.
Article10. Chang GH, Chen YC, Lin KM, Yang YH, Liu CY, Lin MH, et al. Realworld database examining the association between Sjogren’s syndrome and chronic rhinosinusitis. J Clin Med. 2019; Jan. 8(2):155.11. Tsai YT, Huang EI, Chang GH, Tsai MS, Hsu CM, Yang YH, et al. Risk of acute epiglottitis in patients with preexisting diabetes mellitus: a population-based case-control study. PLoS One. 2018; Jun. 13(6):e0199036.
Article12. Chang GH, Su YC, Lin KM, Liu CY, Yang YH, Chang PJ, et al. Deep neck infection in systemic lupus erythematosus patients: real-world evidence. Sci Rep. 2020; Mar. 10(1):4133.
Article13. Chang GH, Tsai MS, Liu CY, Lin MH, Tsai YT, Hsu CM, et al. End-stage renal disease: a risk factor of deep neck infection: a nationwide follow-up study in Taiwan. BMC Infect Dis. 2017; Jun. 17(1):424.
Article14. Tsai MS, Li HY, Huang CG, Wang RY, Chuang LP, Chen NH, et al. Risk of Alzheimer’s disease in obstructive sleep apnea patients with or without treatment: real-world evidence. Laryngoscope. 2020; Sep. 130(9):2292–8.
Article15. Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted Diabetes Complications Severity Index in claims data. Am J Manag Care. 2012; Nov. 18(11):721–6.16. Chen HL, Hsiao FY. Risk of hospitalization and healthcare cost associated with Diabetes Complication Severity Index in Taiwan’s National Health Insurance Research Database. J Diabetes Complications. 2014; Sep-Oct. 28(5):612–6.
Article17. Ministry of Health. 2017 Annual report or health promotion administration. Taipei City: Taiwan Ministry of Health and Welfare;2017.18. Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol. 1999; Dec. 26(3-4):259–65.
Article19. Zhou T, Hu Z, Yang S, Sun L, Yu Z, Wang G. Role of adaptive and innate immunity in type 2 diabetes mellitus. J Diabetes Res. 2018; Nov. 2018:7457269.
Article20. Ostergaard L, Mogensen UM, Bundgaard JS, Dahl A, Wang A, TorpPedersen C, et al. Duration and complications of diabetes mellitus and the associated risk of infective endocarditis. Int J Cardiol. 2019; Mar. 278:280–4.21. Ito H, Ishida H, Takeuchi Y, Antoku S, Abe M, Mifune M, et al. Longterm effect of metformin on blood glucose control in non-obese patients with type 2 diabetes mellitus. Nutr Metab (Lond). 2010; Nov. 7:83.
Article22. Doggrell SA, Warot S. The association between the measurement of adherence to anti-diabetes medicine and the HbA1c. Int J Clin Pharm. 2014; Jun. 36(3):488–97.
Article23. Dandona P. Minimizing glycemic fluctuations in patients with type 2 diabetes: approaches and importance. Diabetes Technol Ther. 2017; Sep. 19(9):498–506.
Article24. Herzon FS. Harris P. Mosher Award thesis. Peritonsillar abscess: incidence, current management practices, and a proposal for treatment guidelines. Laryngoscope. 1995; Aug. 105(8 Pt 3 Suppl 74):1–17.25. Sowerby LJ, Hussain Z, Husein M. The epidemiology, antibiotic resistance and post-discharge course of peritonsillar abscesses in London, Ontario. J Otolaryngol Head Neck Surg. 2013; Jan. 42(1):5.
Article26. Hanna BC, McMullan R, Gallagher G, Hedderwick S. The epidemiology of peritonsillar abscess disease in Northern Ireland. J Infect. 2006; Apr. 52(4):247–53.
Article27. Marom T, Cinamon U, Itskoviz D, Roth Y. Changing trends of peritonsillar abscess. Am J Otolaryngol. 2010; May-Jun. 31(3):162–7.
Article28. Qureshi HA, Ference EH, Tan BK, Chandra RK, Kern RC, Smith SS. National trends in retropharyngeal abscess among adult inpatients with peritonsillar abscess. Otolaryngol Head Neck Surg. 2015; Apr. 152(4):661–6.
Article29. Wang YP, Wang MC, Lin HC, Chou P. The impact of prior tonsillitis and treatment modality on the recurrence of peritonsillar abscess: a nationwide cohort study. PLoS One. 2014; Oct. 9(10):e109887.
Article30. Chung JH, Lee YC, Shin SY, Eun YG. Risk factors for recurrence of peritonsillar abscess. J Laryngol Otol. 2014; Dec. 128(12):1084–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Microbiology of Peritonsillar Abscess
- Two Cases of Peritonsillar Abscess Following Tonsillectomy
- Initial Factors Influencing Duration of Hospital Stay in Adult Patients With Peritonsillar Abscess
- Peritonsillar Abscess in a 40-Day-Old Infant
- Diagnosis of Peritonsillar Abscess Using Gray Scale Image and Color DopplerImage of Intraoral Ultrasonography