Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea
- 2Yonsei University College of Medicine, Seoul, Korea
- 3Department of Biostatics and Data Science, University of Texas Health Science Center at Houston, Houston, TX, USA
- KMID: 2518897
- DOI: http://doi.org/10.4093/dmj.2020.0078
Abstract
- Background
Fetal abdominal obesity (FAO) has been reported to be affected at gestational diabetes mellitus (GDM) diagnosis at 24 to 28 weeks of gestation in older and/or obese women. This study investigated whether the management of GDM improves FAO in GDM subjects near term.
Methods
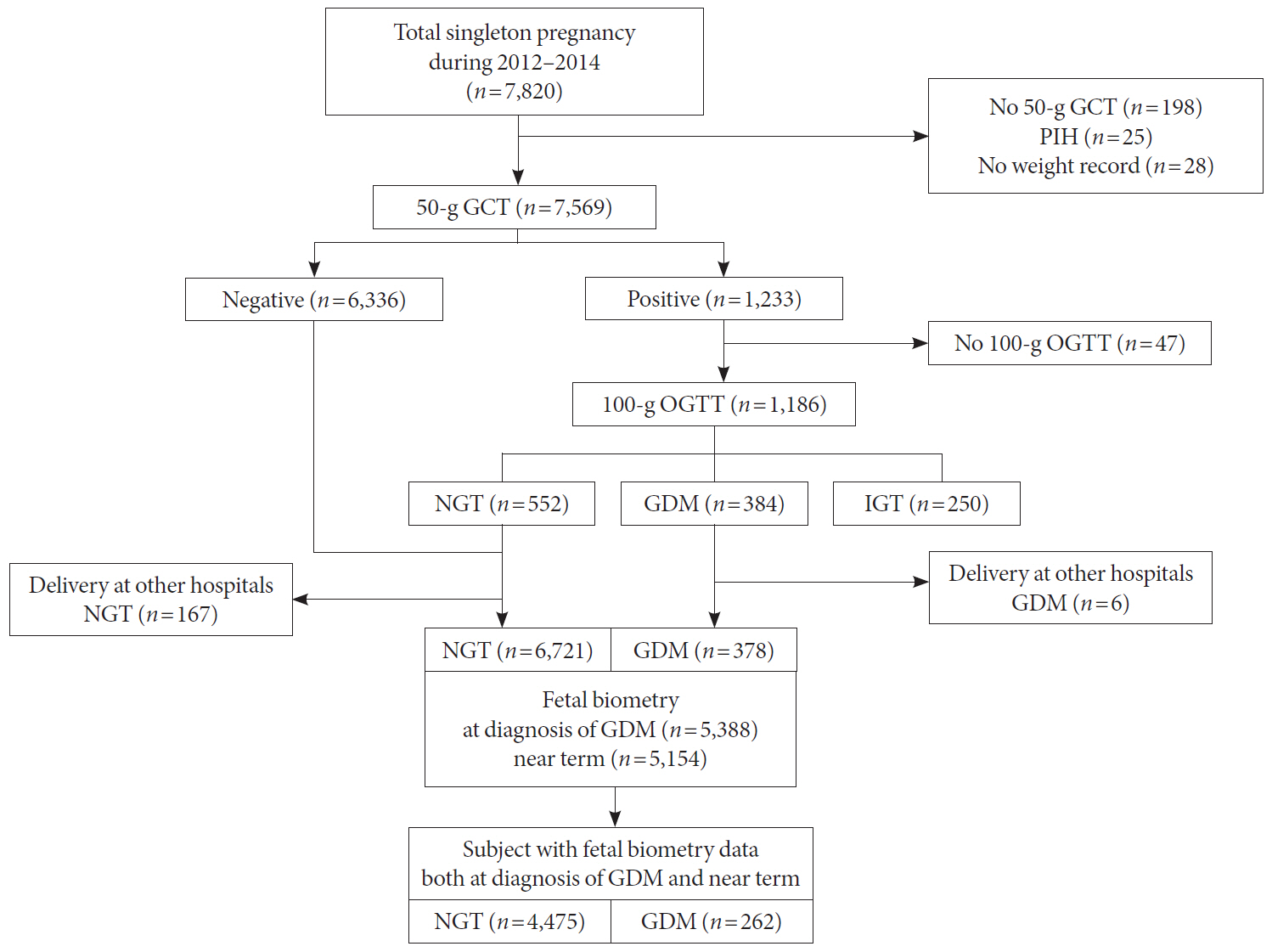
Medical records of 7,099 singleton pregnant women delivering at CHA Gangnam Medical Center were reviewed retrospectively. GDM was diagnosed by 100-g oral glucose tolerance test after 50-g glucose challenge test based on Carpenter–Coustan criteria. GDM subjects were divided into four study groups according to maternal age and obesity. FAO was defined as ≥90th percentile of fetal abdominal overgrowth ratios (FAORs) of the ultrasonographically estimated gestational age (GA) of abdominal circumference per actual GA by the last menstruation period, biparietal diameter, or femur length, respectively.
Results
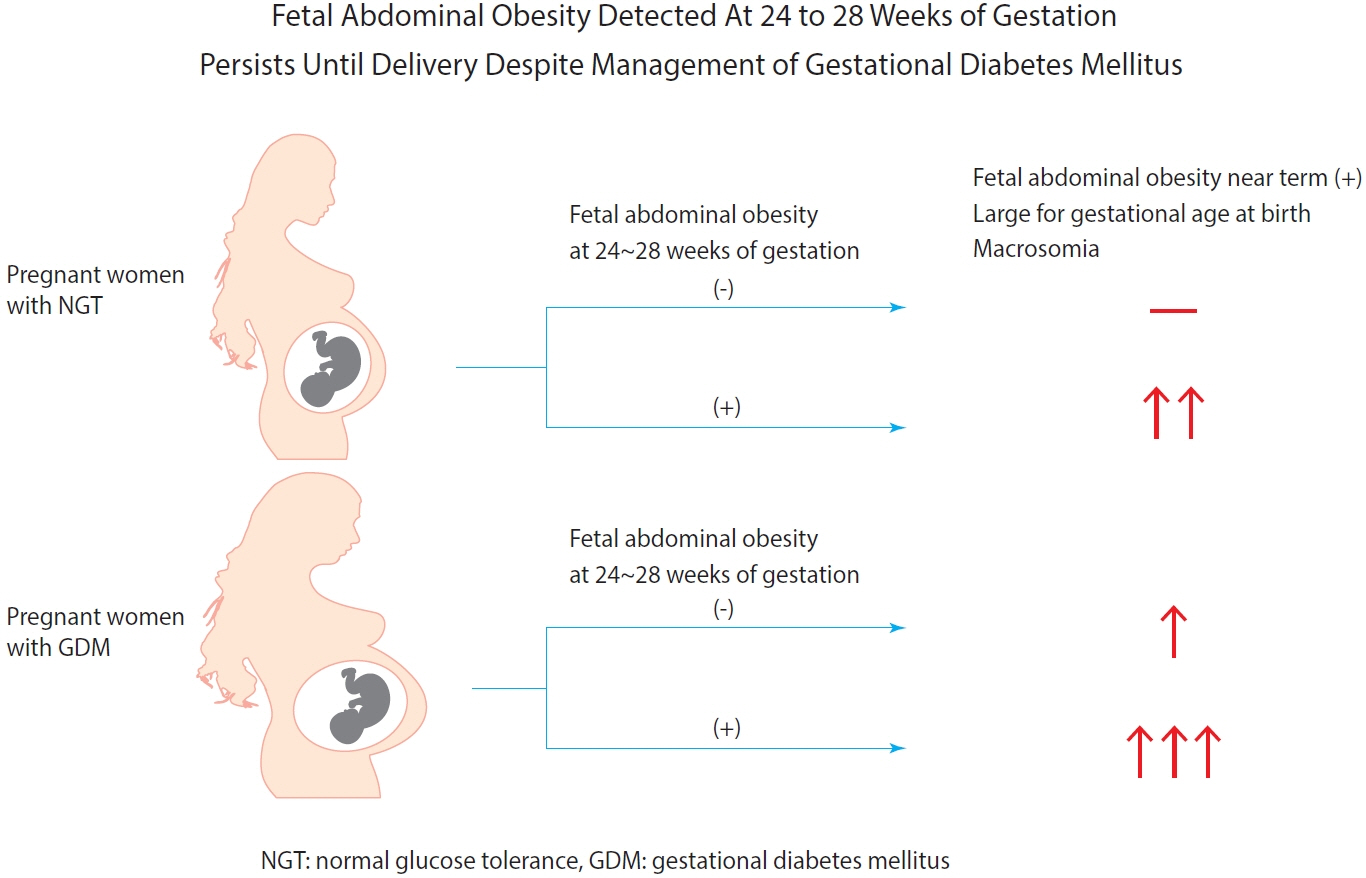
As compared with normal glucose tolerance (NGT) subjects near term, FAORs and odds ratio for FAO were significantly higher in old and/or obese women with GDM but not in young and nonobese women with GDM. For fetuses of GDM subjects with FAO at the time of GDM diagnosis, the odds ratio for exhibiting FAO near term and being large for GA at birth were 7.87 (95% confidence interval [CI], 4.38 to 14.15) and 10.96 (95% CI, 5.58 to 20.53) compared with fetuses of NGT subjects without FAO at GDM diagnosis.
Conclusion
Despite treatment, FAO detected at the time of GDM diagnosis persisted until delivery. Early diagnosis and treatment might be necessary to prevent near term FAO in high-risk older and/or obese women.
Figure
Cited by 4 articles
-
Fetal Abdominal Obesity Detected at 24 to 28 Weeks of Gestation Persists until Delivery Despite Management of Gestational Diabetes Mellitus (
Diabetes Metab J 2021;45:547-57)
Wonjin Kim, Soo Kyung Park, Yoo Lee Kim
Diabetes Metab J. 2021;45(6):970-971. doi: 10.4093/dmj.2021.0253.Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus (
Diabetes Metab J 2021;45:547-57)
Kyung-Soo Kim
Diabetes Metab J. 2021;45(6):966-967. doi: 10.4093/dmj.2021.0252.Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
Joon Ho Moon, Hak Chul Jang
Diabetes Metab J. 2022;46(1):3-14. doi: 10.4093/dmj.2021.0335.Gestational Diabetes Mellitus: Mechanisms Underlying Maternal and Fetal Complications
Jooyeop Lee, Na Keum Lee, Joon Ho Moon
Endocrinol Metab. 2025;40(1):10-25. doi: 10.3803/EnM.2024.2264.
Reference
-
1. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019; 42(Suppl 1):S13–28.2. Zhu Y, Zhang C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr Diab Rep. 2016; 16:7.
Article3. Kim W, Park SK, Kim YL. Gestational diabetes mellitus diagnosed at 24 to 28 weeks of gestation in older and obese women: is it too late? PLoS One. 2019; 14:e0225955.
Article4. Catalano PM, McIntyre HD, Cruickshank JK, McCance DR, Dyer AR, Metzger BE, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012; 35:780–6.
Article5. Pettitt DJ, Baird HR, Aleck KA, Bennett PH, Knowler WC. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N Engl J Med. 1983; 308:242–5.
Article6. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005; 352:2477–86.
Article7. Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009; 361:1339–48.
Article8. Tantanasis T, Daniilidis A, Giannoulis C, Tzafettas M, Dinas K, Loufopoulos A, et al. Sonographic assessment of fetal subcutaneous fat tissue thickness as an indicator of gestational diabetes. Eur J Obstet Gynecol Reprod Biol. 2010; 152:157–62.
Article9. De Santis MS, Taricco E, Radaelli T, Spada E, Rigano S, Ferrazzi E, et al. Growth of fetal lean mass and fetal fat mass in gestational diabetes. Ultrasound Obstet Gynecol. 2010; 36:328–37.
Article10. Larciprete G, Valensise H, Vasapollo B, Novelli GP, Parretti E, Altomare F, et al. Fetal subcutaneous tissue thickness (SCTT) in healthy and gestational diabetic pregnancies. Ultrasound Obstet Gynecol. 2003; 22:591–7.
Article11. Aksoy H, Aksoy U, Yucel B, Saygi Ozyurt S, Aydın T, et al. Fetal anterior abdominal wall thickness may be an early ultrasonographic sign of gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2016; 29:2028–32.
Article12. Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol. 2003; 189:1698–704.
Article13. Enzi G, Inelmen EM, Caretta F, Villani F, Zanardo V, DeBiasi F. Development of adipose tissue in newborns of gestational-diabetic and insulin-dependent diabetic mothers. Diabetes. 1980; 29:100–4.
Article14. Nasrat H, Abalkhail B, Fageeh W, Shabat A, el Zahrany F. Anthropometric measurement of newborns of gestational diabetic mothers: does it indicate disproportionate fetal growth? J Matern Fetal Med. 1997; 6:291–5.15. Palatnik A, Mele L, Landon MB, Reddy UM, Ramin SM, Carpenter MW, et al. Timing of treatment initiation for mild gestational diabetes mellitus and perinatal outcomes. Am J Obstet Gynecol. 2015; 213:560.16. Sovio U, Murphy HR, Smith GC. Accelerated fetal growth prior to diagnosis of gestational diabetes mellitus: a prospective cohort study of nulliparous women. Diabetes Care. 2016; 39:982–7.
Article17. Shinozuka N, Masuda H, Kagawa H, Taketani Y. Standard values of ultrasonographic fetal biometry. Jpn J Med Ultrason. 1996; 23:877–88.18. Shinozuka N, Akamatsu N, Sato S, Kanzaki T, Takeuch H, Natori M, Chiba Y, et al. Ellipse tracing fetal growth assessment using abdominal circumference. J Med Ultrasound. 2000; 8:87–94.19. Ryan DK, Haddow L, Ramaesh A, Kelly R, Johns EC, Denison FC, et al. Early screening and treatment of gestational diabetes in high-risk women improves maternal and neonatal outcomes: a retrospective clinical audit. Diabetes Res Clin Pract. 2018; 144:294–301.
Article20. Lee JJ, Kim MH, Ko KO, Kim KA, Kim SM, Kim ER, et al. The study of growth measurements at different gestatioal ages of Korean newborn the survey and statistics. J Korean Soc Neonatol. 2006; 13:47–57.21. Venkataraman H, Ram U, Craik S, Arungunasekaran A, Seshadri S, Saravanan P. Increased fetal adiposity prior to diagnosis of gestational diabetes in South Asians: more evidence for the ‘thin-fat’ baby. Diabetologia. 2017; 60:399–405.
Article22. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–9.23. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–63.24. Low S, Chin MC, Ma S, Heng D, Deurenberg-Yap M. Rationale for redefining obesity in Asians. Ann Acad Med Singap. 2009; 38:66–9.25. Durnwald C. Gestational diabetes mellitus: glycemic control and maternal prognosis. Available from:https://www.uptodate.com/contents/gestational-diabetes-mellitus-glycemic-control-and-maternal-prognosis/print (cited 2021 Jan 15).26. Kim MH, Kwak SH, Kim SH, Hong JS, Chung HR, Choi SH, et al. Pregnancy outcomes of women additionally diagnosed as gestational diabetes by the International Association of the Diabetes and Pregnancy study groups criteria. Diabetes Metab J. 2019; 43:766–75.
Article27. Poissonnet CM, Burdi AR, Bookstein FL. Growth and development of human adipose tissue during early gestation. Early Hum Dev. 1983; 8:1–11.
Article28. Riskin-Mashiah S, Younes G, Damti A, Auslender R. First-trimester fasting hyperglycemia and adverse pregnancy outcomes. Diabetes Care. 2009; 32:1639–43.
Article29. Colstrup M, Mathiesen ER, Damm P, Jensen DM, Ringholm L. Pregnancy in women with type 1 diabetes: have the goals of St. Vincent declaration been met concerning foetal and neonatal complications? J Matern Fetal Neonatal Med. 2013; 26:1682–6.
Article30. Seshiah V, Cynthia A, Balaji V, Balaji MS, Ashalata S, Sheela R, et al. Detection and care of women with gestational diabetes mellitus from early weeks of pregnancy results in birth weight of newborn babies appropriate for gestational age. Diabetes Res Clin Pract. 2008; 80:199–202.
Article31. Feghali MN, Abebe KZ, Comer DM, Caritis S, Catov JM, Scifres CM. Pregnancy outcomes in women with an early diagnosis of gestational diabetes mellitus. Diabetes Res Clin Pract. 2018; 138:177–86.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus (Diabetes Metab J 2021;45:547-57)
- Fetal Abdominal Obesity Detected at 24 to 28 Weeks of Gestation Persists until Delivery Despite Management of Gestational Diabetes Mellitus (Diabetes Metab J 2021;45:547-57)
- Perinatal Outcomes according to Screening Timing in Gestational Diabetic Women with Family History of Diabetes
- Obstetrical Management of Gestational Diabetes Mellitus
- The Importance of Early Diagnosis for Gestational Diabetes Mellitus