Diabetes Metab J.
2021 Jul;45(4):505-514. 10.4093/dmj.2020.0057.
Cardiovascular Safety of Sodium Glucose Cotransporter 2 Inhibitors as Add-on to Metformin Monotherapy in Patients with Type 2 Diabetes Mellitus
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea
- KMID: 2518893
- DOI: http://doi.org/10.4093/dmj.2020.0057
Abstract
- Background
Using real-world data, cardiovascular safety was investigated in metformin users newly starting sodium glucose cotransporter 2 (SGLT2) inhibitors compared with other glucose-lowering drugs in Korea.
Methods
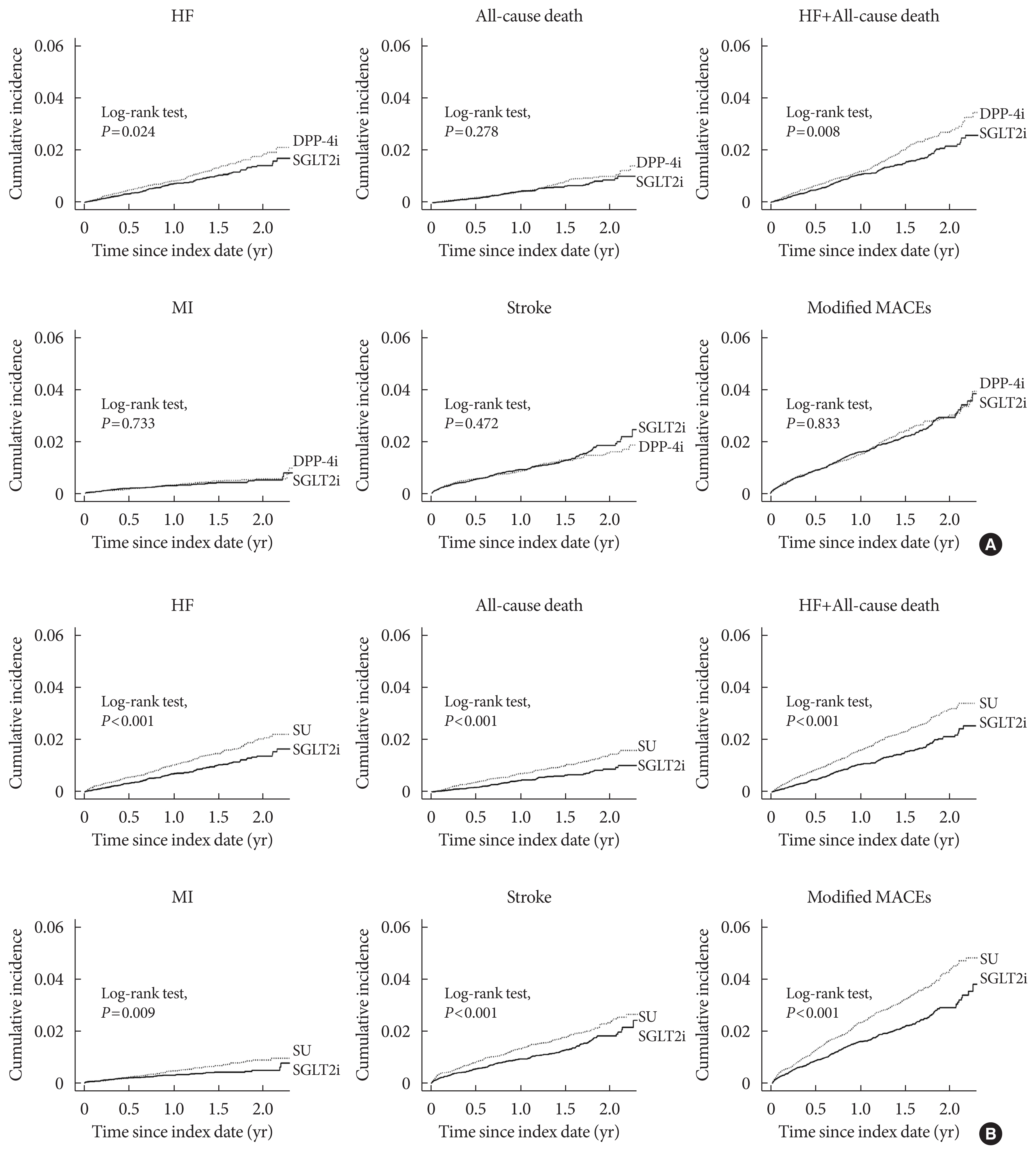
This was a retrospective observational study using the National Health Insurance Service claims database in Korea. The study period was from September 2014 to December 2016. The study included subjects who were newly prescribed SGLT2 inhibitors or other glucose-lowering drugs while on metformin monotherapy; cohort 1 was composed of new users of SGLT2 inhibitors versus dipeptidyl peptidase-4 (DPP-4) inhibitors and cohort 2 included new users of SGLT2 inhibitors versus sulfonylureas. To balance the patient characteristics, propensity score matching was performed at a 1:1 ratio. Cardiovascular outcomes included hospitalization for heart failure (HHF), all-cause mortality, HHF plus all-cause mortality, myocardial infarction (MI), stroke, and modified major adverse cardiovascular events (MACEs).
Results
After propensity score matching, each cohort group was well balanced at baseline (21,688 pairs in cohort 1 and 20,120 pairs in cohort 2). As the second-line treatment, use of SGLT2 inhibitors was associated with a lower risk of HHF and HHF plus all-cause mortality compared with DPP-4 inhibitors. In addition, use of SGLT2 inhibitors versus sulfonylurea as add-on therapy to metformin was associated with decreased risks of HHF, all-cause mortality, HHF plus all-cause mortality, MI, stroke, and modified MACEs.
Conclusion
SGLT2 inhibitors can be a good second-line drug to reduce the incidence of cardiovascular diseases compared with DPP-4 inhibitors or sulfonylureas in people with type 2 diabetes mellitus.
Keyword
Figure
Cited by 2 articles
-
Cardiovascular Safety of SGLT2 Inhibitors Compared to DPP4 Inhibitors and Sulfonylureas as the Second-Line of Therapy in T2DM Using Large, Real-World Clinical Data in Korea
Kyuho Kim, Sung Hee Choi
Diabetes Metab J. 2021;45(4):502-504. doi: 10.4093/dmj.2021.0158.Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes Metab J. 2023;47(1):10-26. doi: 10.4093/dmj.2022.0420.
Reference
-
1. Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV, et al. Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation. 1999; 100:1134–46.2. Kannel WB, Hjortland M, Castelli WP. Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol. 1974; 34:29–34.
Article3. Ko SH, Han K, Lee YH, Noh J, Park CY, Kim DJ, et al. Past and current status of adult type 2 diabetes mellitus management in Korea: a National Health Insurance Service database analysis. Diabetes Metab J. 2018; 42:93–100.
Article4. International Diabetes Federation. Diabetes and cardiovascular disease report. Brussels: IDF;2016.5. American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes. 2019. Diabetes Care. 2019; 42(Suppl 1):S103–23.6. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008; 358:2560–72.
Article7. Gerstein HC, Riddle MC, Kendall DM, Cohen RM, Goland R, Feinglos MN, et al. Glycemia treatment strategies in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol. 2007; 99:34i–43i.
Article8. Scirica BM, Braunwald E, Raz I, Cavender MA, Morrow DA, Jarolim P, et al. Heart failure, saxagliptin, and diabetes mellitus: observations from the SAVOR-TIMI 53 randomized trial. Circulation. 2014; 130:1579–88.
Article9. Nassif M, Kosiborod M. Effect of glucose-lowering therapies on heart failure. Nat Rev Cardiol. 2018; 15:282–91.
Article10. Jung CH, Jang JE, Park JY. A novel therapeutic agent for type 2 diabetes mellitus: SGLT2 inhibitor. Diabetes Metab J. 2014; 38:261–73.
Article11. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–28.
Article12. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017; 377:644–57.
Article13. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019; 380:347–57.
Article14. Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019; 393:31–9.
Article15. Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018; 41:2669–701.
Article16. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article17. Kosiborod M, Lam CSP, Kohsaka S, Kim DJ, Karasik A, Shaw J, et al. Cardiovascular events associated with SGLT-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL 2 study. J Am Coll Cardiol. 2018; 71:2628–39.18. Persson F, Nystrom T, Jorgensen ME, Carstensen B, Gulseth HL, Thuresson M, et al. Dapagliflozin is associated with lower risk of cardiovascular events and all-cause mortality in people with type 2 diabetes (CVD-REAL Nordic) when compared with dipeptidyl peptidase-4 inhibitor therapy: a multinational observational study. Diabetes Obes Metab. 2018; 20:344–51.19. Birkeland KI, Jorgensen ME, Carstensen B, Persson F, Gulseth HL, Thuresson M, et al. Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. Lancet Diabetes Endocrinol. 2017; 5:709–17.
Article20. Kosiborod M, Cavender MA, Fu AZ, Wilding JP, Khunti K, Holl RW, et al. Lower risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL Study (comparative effectiveness of cardiovascular outcomes in new users of sodium-glucose cotransporter-2 inhibitors). Circulation. 2017; 136:249–59.21. Jensen MH, Kjolby M, Hejlesen O, Jakobsen PE, Vestergaard P. Risk of major adverse cardiovascular events, severe hypoglycemia, and all-cause mortality for widely used antihyperglycemic dual and triple therapies for type 2 diabetes management: a cohort study of all Danish users. Diabetes Care. 2020; 43:1209–18.
Article22. Goto A, Arah OA, Goto M, Terauchi Y, Noda M. Severe hypoglycaemia and cardiovascular disease: systematic review and meta-analysis with bias analysis. BMJ. 2013; 347:f4533.
Article23. McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012; 35:1897–901.
Article24. Kashiwagi A, Maegawa H. Metabolic and hemodynamic effects of sodium-dependent glucose cotransporter 2 inhibitors on cardio-renal protection in the treatment of patients with type 2 diabetes mellitus. J Diabetes Investig. 2017; 8:416–27.
Article25. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998; 352:854–65.26. Rosenstock J, Kahn SE, Johansen OE, Zinman B, Espeland MA, Woerle HJ, et al. Effect of linagliptin vs glimepiride on major adverse cardiovascular outcomes in patients with type 2 diabetes: the CAROLINA randomized clinical trial. JAMA. 2019; 322:1155–66.27. Fonseca VA. Defining and characterizing the progression of type 2 diabetes. Diabetes Care. 2009; 32(Suppl 2):S151–6.
Article28. Gamble JM, Simpson SH, Eurich DT, Majumdar SR, Johnson JA. Insulin use and increased risk of mortality in type 2 diabetes: a cohort study. Diabetes Obes Metab. 2010; 12:47–53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Emerging Safety Issues of Dipeptidyl Peptidase-4 Inhibitors and Sodium Glucose Cotransporter 2 Inhibitors: How to Interpret and Apply in Clinical Practice
- Sodium-Glucose Cotransporter 2 Inhibitors for People with Type 1 Diabetes
- Prevention of Major Adverse Cardiovascular and Renal Outcomes with Sodium-Glucose Cotransporter 2 Inhibitors
- Glucose Lowering Effect of SGLT2 Inhibitors: A Review of Clinical Studies
- The Side Effects of Sodium Glucose Cotransporter 2 (SGLT2) Inhibitor