Yeungnam Univ J Med.
2021 Jul;38(3):258-263. 10.12701/yujm.2021.00983.
Sciatic nerve neurolymphomatosis as the initial presentation of primary diffuse large B-cell lymphoma: a rare cause of leg weakness
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Rehabilitation Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 3Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 4Department of Pathology, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2518670
- DOI: http://doi.org/10.12701/yujm.2021.00983
Abstract
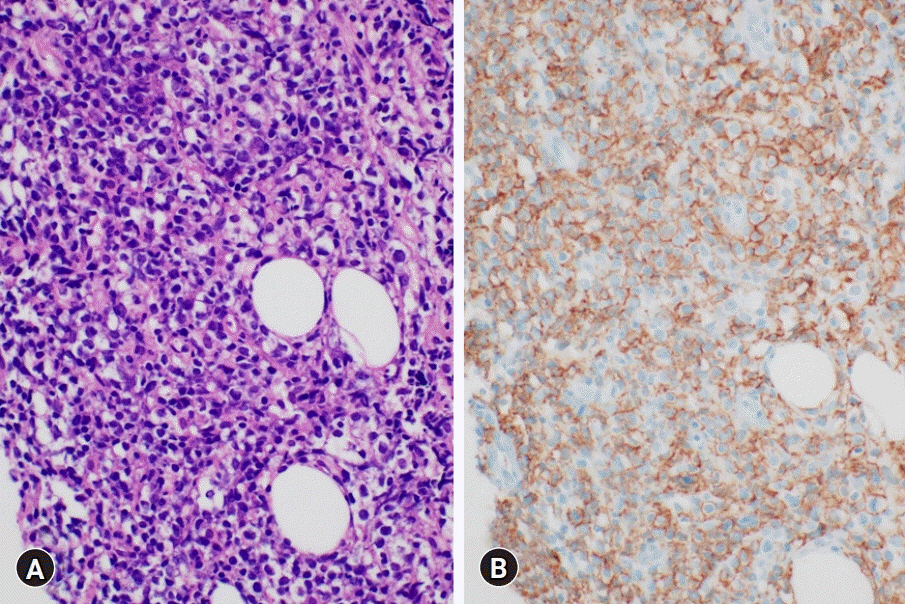
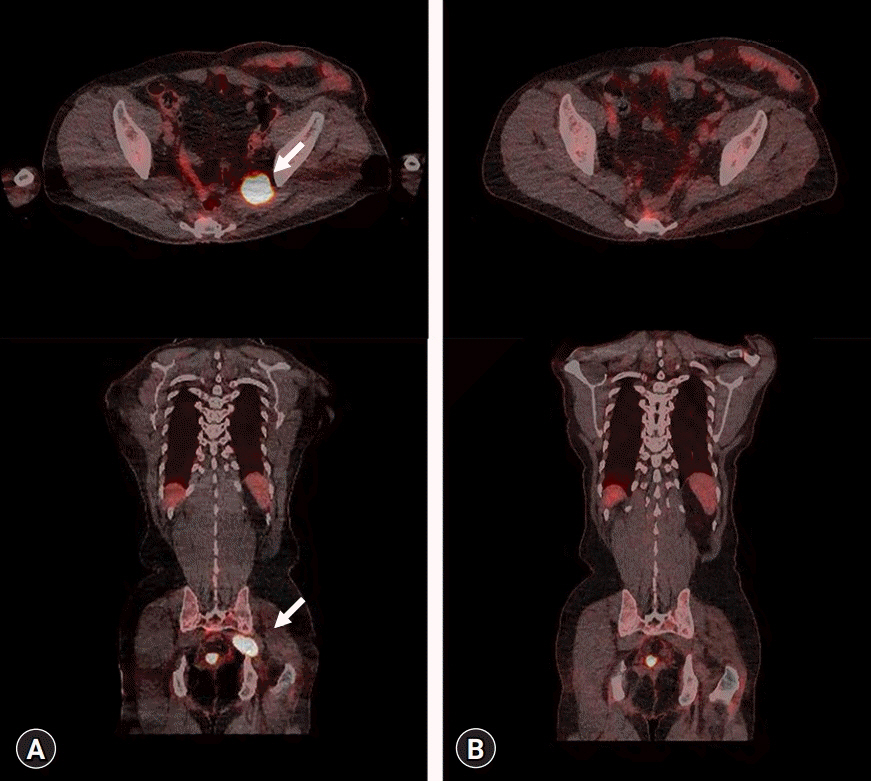
- Neurolymphomatosis (NL) is defined as the involvement of the peripheral nervous system in lymphocytic invasion. It is a very rare form of lymphoma that may occur as an initial presentation or recurrence. It affects various peripheral nervous structures and can therefore mimic disc-related nerve root pathology or compressive mononeuropathy. NL often occurs in malignant B-cell non-Hodgkin lymphomas. Notwithstanding its aggressiveness or intractability, NL should be discriminated from other neurologic complications of lymphoma. Herein, we present a case of primary NL as the initial presentation of diffuse large B-cell lymphoma (DLBCL) of the sciatic nerve. The patient presented with weakness and pain in his left leg but had no obvious lesion explaining the neurologic deficit on initial lumbosacral and knee magnetic resonance imaging (MRI). NL of the left sciatic nerve at the greater sciatic foramen was diagnosed based on subsequent hip MRI, electrodiagnostic test, positron emission tomography/computed tomography, and nerve biopsy findings. Leg weakness slightly improved after chemotherapy and radiotherapy. We report a case wherein NL, a rare cause of leg weakness, manifested as the initial presentation of primary DLBCL involving the sciatic nerve at the greater sciatic foramen.
Figure
Reference
-
References
1. Gan HK, Azad A, Cher L, Mitchell PL. Neurolymphomatosis: diagnosis, management, and outcomes in patients treated with rituximab. Neuro Oncol. 2010; 12:212–5.
Article2. Viala K, Béhin A, Maisonobe T, Léger JM, Stojkovic T, Davi F, et al. Neuropathy in lymphoma: a relationship between the pattern of neuropathy, type of lymphoma and prognosis? J Neurol Neurosurg Psychiatry. 2008; 79:778–82.
Article3. Roncaroli F, Poppi M, Riccioni L, Frank F. Primary non-Hodgkin’s lymphoma of the sciatic nerve followed by localization in the central nervous system: case report and review of the literature. Neurosurgery. 1997; 40:618–22.
Article4. Jeong J, Kim SW, Sung DH. Neurolymphomatosis: a single-center experience of neuromuscular manifestations, treatments, and outcomes. J Neurol. 2021; 268:851–9.
Article5. Advani P, Paulus A, Murray P, Jiang L, Goff R, Pooley R, et al. A rare case of primary high-grade large B-cell lymphoma of the sciatic nerve. Clin Lymphoma Myeloma Leuk. 2015; 15:e117–20.
Article6. Kahraman S, Sabuncuoglu H, Gunhan O, Gurses MA, Sirin S. A rare reason of foot drop caused by primary diffuse large b-cell lymphoma of the sciatic nerve: case report. Acta Neurochir (Wien). 2010; 152:125–8.
Article7. Priori A, Magno S, Campiglio L, Lovati E, Tagliabue L. Imaging of sciatic lymphoma. Muscle Nerve. 2017; 56:E22–3.
Article8. Lhermitte J, Trelles J. Neurolymphomatosis péripherique humaine. Presse Med. 1934; 42:289–92.9. Grisariu S, Avni B, Batchelor TT, van den Bent MJ, Bokstein F, Schiff D, et al. Neurolymphomatosis: an International Primary CNS Lymphoma Collaborative Group report. Blood. 2010; 115:5005–11.
Article10. Descamps MJ, Barrett L, Groves M, Yung L, Birch R, Murray NM, et al. Primary sciatic nerve lymphoma: a case report and review of the literature. J Neurol Neurosurg Psychiatry. 2006; 77:1087–9.
Article11. Facchinelli D, Ciliberti E, Stüssi G, Ceriani L, Zucca E. Sciatic pain by neurolymphomatosis as initial presentation of disseminated diffuse large B cell lymphoma involving the testis and the CNS. Hematol Oncol. 2020; 38:197–200.
Article12. Baehring JM, Damek D, Martin EC, Betensky RA, Hochberg FH. Neurolymphomatosis. Neuro Oncol. 2003; 5:104–15.
Article13. Quiñones-Hinojosa A, Friedlander RM, Boyer PJ, Batchelor TT, Chiocca EA. Solitary sciatic nerve lymphoma as an initial manifestation of diffuse neurolymphomatosis: case report and review of the literature. J Neurosurg. 2000; 92:165–9.14. Shree R, Goyal MK, Modi M, Gaspar BL, Radotra BD, Ahuja CK, et al. The diagnostic dilemma of neurolymphomatosis. J Clin Neurol. 2016; 12:274–81.
Article15. Shah HJ, Lele VR, Keraliya AR, Aland PS. Peripheral nerves and muscles involvement by non-Hodgkin’s lymphoma seen on FDG PET/CT scan. Neurol India. 2014; 62:83–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurolymphomatosis Involving Antebrachial Cutaneous Nerve
- Neurolymphomatosis Involving Sciatic Nerve: A Case Report
- When We Consider Neurolymphomatosis in Patient with Lumbosacral Plexopathy with an Extreme Leg Pain?
- Diffuse Large B-Cell Lymphoma Mimicking Schwannoma of Lumbar Spine
- Neurolymphomatosis on F-18 FDG PET/CT and MRI Findings: A Case Report