J Pathol Transl Med.
2021 Jul;55(4):289-297. 10.4132/jptm.2021.05.24.
Clinicopathologic features of cutaneous metastases from internal malignancies
- Affiliations
-
- 1Department of Dermatology, Yeungnam University College of Medicine, Daegu, Korea
- 2Yeungnam University College of Medicine, Daegu, Korea
- 3Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2518429
- DOI: http://doi.org/10.4132/jptm.2021.05.24
Abstract
- Background
Cutaneous metastasis (CM) is the spread of cancer cells from a primary site to the skin and is rarely the first sign of silent cancer. We investigated the clinicopathological characteristics of CM from internal malignancies in Korean patients treated at our institution over 20 years.
Methods
The clinicopathological findings of 112 patients (62 females, 50 males) with CM diagnosed at Yeungnam University Hospital between 2000 and 2020 were retrospectively reviewed.
Results
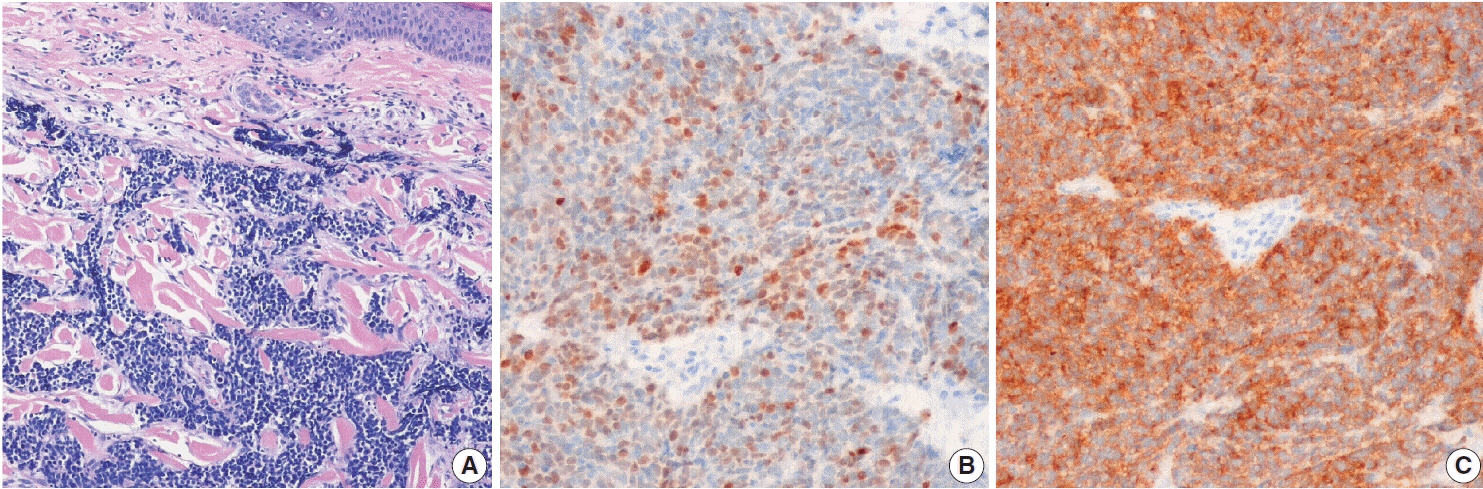
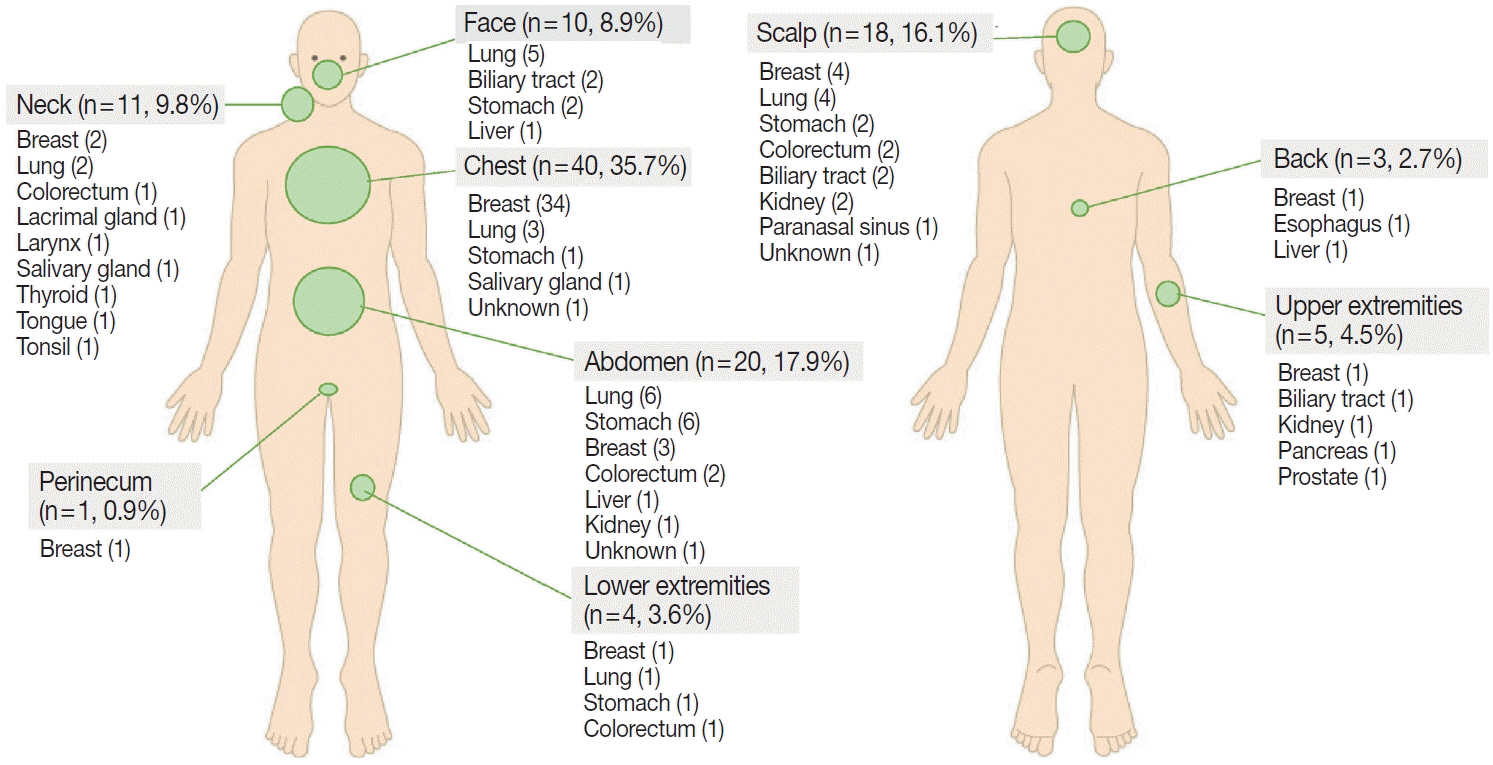
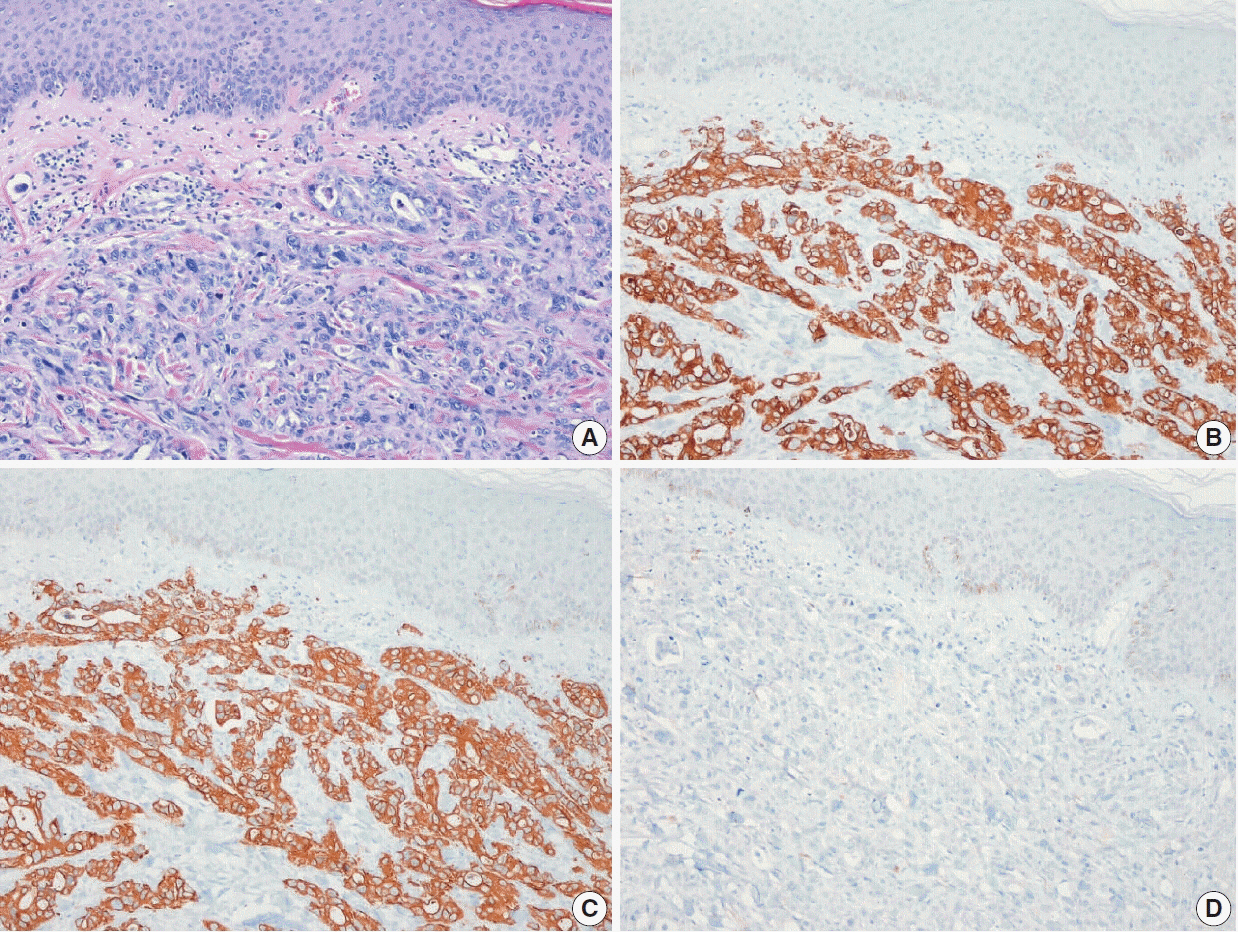
Mean patient age was 58.6 years (range, 26 to 87 years), and the most common primary cancer site was breast (74.2%) in women and lung (36.0%) in men. Ninety-six patients (85.7%) presented with CM after primary tumor diagnosis. CM from the lung or biliary tract usually occurred within 2 years of primary tumor diagnosis, whereas metastases from the breast and kidney occurred several years later. The chest, abdomen, and scalp were common sites of CM. Breast cancer usually metastasized to chest skin, while gastrointestinal tract cancers commonly metastasized to the abdomen. The scalp was a common location for CM from various tumors. The most common dermatologic presentations were nodules and masses. Immunohistochemical studies helped identify underlying malignancies when primary tumors were unknown.
Conclusions
The relative frequency of CM parallels the overall incidence of primary malignant tumors, and CMs usually occur at anatomic sites close to the primary tumor. CM can be diagnosed based on clinical, radiological, and histological features; however, immunohistochemical study is required in some cases.
Keyword
Figure
Reference
-
References
1. Moon JI, Park JY, Jeon TJ, et al. Non-umbilical cutaneous metastasis of pancreatic adenocarcinoma as the first clinical manifestation: a case report. Korean J Gastroenterol. 2016; 68:221–4.
Article2. Kwon MJ, Ryu SH, Jo SY, et al. A case of hepatocellular carcinoma presenting as a gingival mass. Korean J Gastroenterol. 2016; 68:321–5.
Article3. Song YW, Kim WS, Yun GY, et al. A case of early gastric cancer with nodular tumor-like scalp metastasis. Korean J Gastroenterol. 2016; 68:36–9.
Article4. Yang HJ, Kang SY. Cutaneous metastatic renal cell carcinoma to the scalp. Arch Craniofac Surg. 2019; 20:392–6.
Article5. Kim JH, Kim MJ, Sim WY, Lew BL. Alopecia neoplastica due to gastric adenocarcinoma metastasis to the scalp, presenting as alopecia: a case report and literature review. Ann Dermatol. 2014; 26:624–7.
Article6. Kim MK, Kim SH, Lee YY, et al. Metastatic skin lesions on lower extremities in a patient with recurrent serous papillary ovarian carcinoma: a case report and literature review. Cancer Res Treat. 2012; 44:142–5.
Article7. An MK, Park BW, Cho EB, Park EJ, Kim KH, Kim KJ. A case of cutaneous metastasis of nasopharyngeal carcinoma on the face. Korean J Dermatol. 2019; 57:80–3.8. Hong SG, Jo SY, Jeong HH, et al. Cutaneous metastasis originating from esophageal carcinoma: a case report. Korean J Dermatol. 2020; 58:269–72.9. Lee JY, Shin SJ, Yoo CS, Kil MS, Kim CW, Kim SS. A case of zosteriform cutaneous metastasis from lung cancer. Korean J Dermatol. 2013; 51:272–5.10. Choi ME, Jung CJ, Lee WJ, et al. Clinicopathological study of Korean patients with cutaneous metastasis from internal malignancies. Australas J Dermatol. 2020; 61:e139–42.
Article11. Brownstein MH, Helwig EB. Spread of tumors to the skin. Arch Dermatol. 1973; 107:80–6.
Article12. Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma: a retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990; 22:19–26.13. Hu SC, Chen GS, Lu YW, Wu CS, Lan CC. Cutaneous metastases from different internal malignancies: a clinical and prognostic appraisal. J Eur Acad Dermatol Venereol. 2008; 22:735–40.
Article14. Sittart JA, Senise M. Cutaneous metastasis from internal carcinomas: a review of 45 years. An Bras Dermatol. 2013; 88:541–4.
Article15. Handa U, Kundu R, Dimri K. Cutaneous metastasis: a study of 138 cases diagnosed by fine-needle aspiration cytology. Acta Cytol. 2017; 61:47–54.
Article16. Hong S, Won YJ, Park YR, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020; 52:335–50.
Article17. Gul U, Kilic A, Gonul M, Kulcu Cakmak S, Erinckan C. Spectrum of cutaneous metastases in 1287 cases of internal malignancies: a study from Turkey. Acta Derm Venereol. 2007; 87:160–2.
Article18. Mok ZR, Yong AM, Leung AJ, Tan KB, Aw DC. Cutaneous metastasis: experience from a tertiary healthcare institution in Singapore. Int J Dermatol. 2017; 56:1497–8.
Article19. Shah SR, Applebaum DS, Potenziani S, Huttenbach YT, Wolf J, Orengo IF. Cutaneous metastasis to the scalp as the primary presentation of colorectal adenocarcinoma. Dermatol Online J. 2017. Nov. 15. [Epub]. http://dx.doi.org/10.5070/D32311037274.
Article20. Habermehl G, Ko J. Cutaneous metastases: a review and diagnostic approach to tumors of unknown origin. Arch Pathol Lab Med. 2019; 143:943–57.
Article21. Hussein MR. Skin metastasis: a pathologist's perspective. J Cutan Pathol. 2010; 37:e1–20.
Article22. Yang DT, Holden JA, Florell SR. CD117, CK20, TTF-1, and DNA topoisomerase II-alpha antigen expression in small cell tumors. J Cutan Pathol. 2004; 31:254–61.23. Kervarrec T, Tallet A, Miquelestorena-Standley E, et al. Diagnostic accuracy of a panel of immunohistochemical and molecular markers to distinguish Merkel cell carcinoma from other neuroendocrine carcinomas. Mod Pathol. 2019; 32:499–510.
Article24. Green AR, Young P, Krivinskas S, et al. The expression of ERalpha, ERbeta and PR in lobular carcinoma in situ of the breast determined using laser microdissection and real-time PCR. Histopathology. 2009; 54:419–27.25. Matsuoka K, Ohsumi S, Takashima S, Saeki T, Aogi K, Mandai K. Occult breast carcinoma presenting with axillary lymph node metastases: follow-up of eleven patients. Breast Cancer. 2003; 10:330–4.
Article26. Gomez-Fernandez C, Daneshbod Y, Nassiri M, Milikowski C, Alvarez C, Nadji M. Immunohistochemically determined estrogen receptor phenotype remains stable in recurrent and metastatic breast cancer. Am J Clin Pathol. 2008; 130:879–82.
Article27. Liu H. Application of immunohistochemistry in breast pathology: a review and update. Arch Pathol Lab Med. 2014; 138:1629–42.
Article28. Monaco SE, Wu Y, Teot LA, Cai G. Assessment of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) status in the fine needle aspirates of metastatic breast carcinomas. Diagn Cytopathol. 2013; 41:308–15.
Article29. Werling RW, Yaziji H, Bacchi CE, Gown AM. CDX2, a highly sensitive and specific marker of adenocarcinomas of intestinal origin: an immunohistochemical survey of 476 primary and metastatic carcinomas. Am J Surg Pathol. 2003; 27:303–10.30. Kandalaft PL, Gown AM. Practical applications in immunohistochemistry: carcinomas of unknown primary site. Arch Pathol Lab Med. 2016; 140:508–23.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Four Cases of Cutaneous Metastasis to the Scalp from Internal Malignancies
- Cutaneous Metastasis from Prostatic Cancer
- A case of zosteriform metastasis in breast origin
- A Case of Esophageal Adenocarcinoma Metastasized to the Scalp
- Cutaneous Metastasis from Cholangiocarcinoma as the First Clinical Sign: A Report of Two Cases