Cancer Res Treat.
2021 Jul;53(3):813-818. 10.4143/crt.2020.826.
Cervical Cancer in Women with Normal Papanicolaou Tests: A Korean Nationwide Cohort Study
- Affiliations
-
- 1Department of Obstetrics and Gynecology, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea
- 2Department of Preventive Medicine, Konkuk University School of Medicine, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea
- 4Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2518405
- DOI: http://doi.org/10.4143/crt.2020.826
Abstract
- Purpose
This study aimed to evaluate the risk of cervical cancer diagnosed within 1 year after the last of multiple consecutive normal Papanicolau (Pap) tests.
Materials and Methods
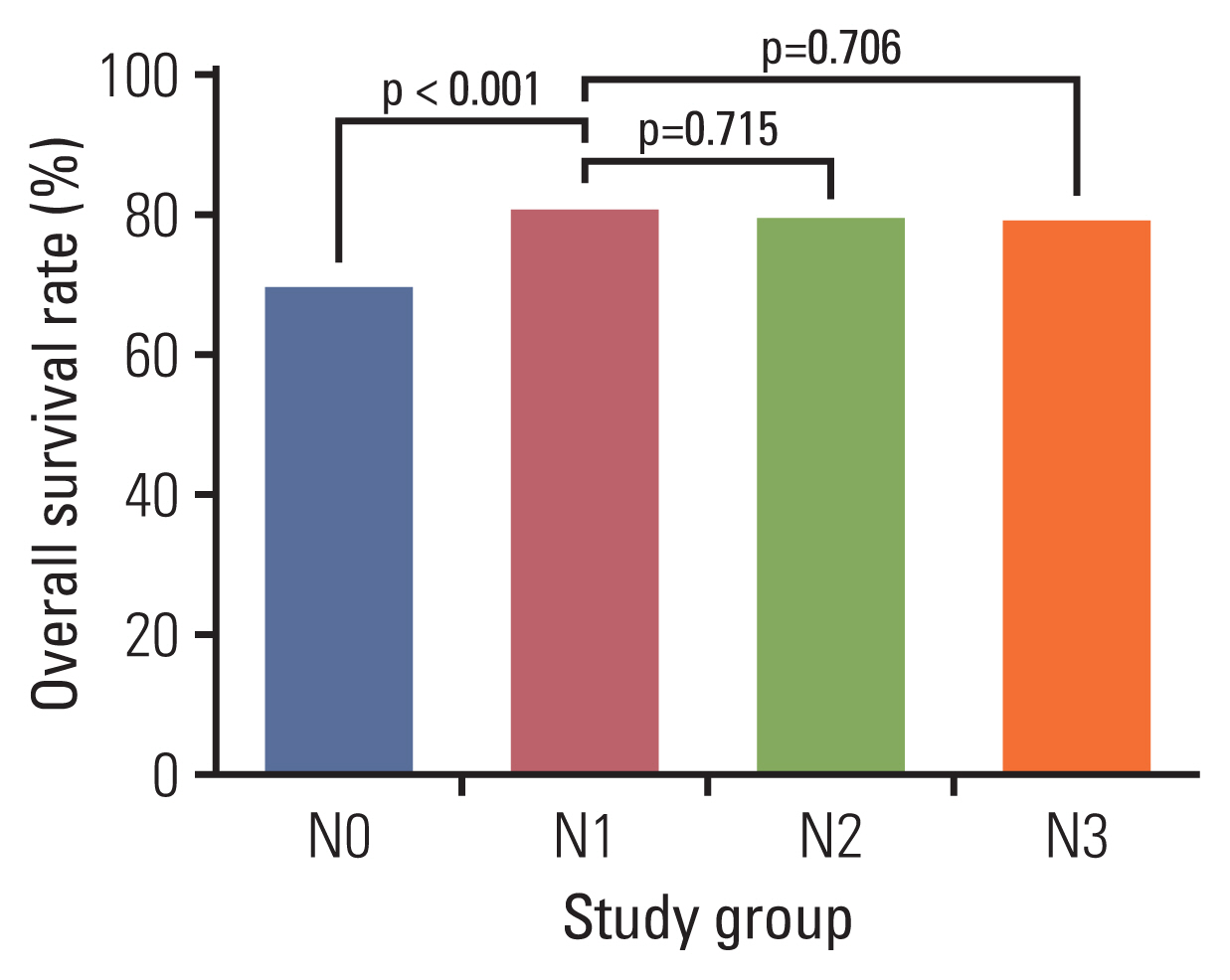
The database of the National Health Insurance Service was used. We obtained Pap test data for 11,052,116 women aged 30-79 between 2007-2012. The cumulative incidence rates and 5-year overall survival rates of cervical cancer diagnosed within 1 year after the last normal Pap test were compared between women with one (N1), two (N2), and three consecutive normal Pap tests (N3). Women who did not receive a Pap test during the study period were assigned in the N0 group.
Results
The 1-year cumulative incidence rates of cervical cancer were 58.9, 24.6, 20.3, and 14.2 per 105 in the N0, N1, N2, and N3 groups, respectively. Compared to the N1 group, the risk of cervical cancer diagnosed within 1 year of the last normal Pap test decreased by 17% (relative risk [RR], 0.825; 95% confidence interval [CI], 0.716 to 0.951) in the N2 group and 42% (RR, 0.578; 95% CI, 0.480 to 0.695) in the N3 group. However, the 5-year survival rate in women diagnosed with cervical cancer within 1 year of the last normal Pap test in the N3 group was not higher than that of the N1 group (79.6% vs. 81.3%, p=0.706).
Conclusion
As normal Pap tests are consecutively repeated, cervical cancer risk significantly decreases. However, previous consecutive normal Pap tests are not associated with improving survival outcomes in women shortly diagnosed with cervical cancer after the last normal Pap test.
Figure
Reference
-
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article2. Arbyn M, Raifu AO, Weiderpass E, Bray F, Anttila A. Trends of cervical cancer mortality in the member states of the European Union. Eur J Cancer. 2009; 45:2640–8.
Article3. Wingo PA, Cardinez CJ, Landis SH, Greenlee RT, Ries LA, Anderson RN, et al. Long-term trends in cancer mortality in the United States, 1930–1998. Cancer. 2003; 97:3133–275.
Article4. Lim MC, Won YJ, Ko MJ, Kim M, Shim SH, Suh DH, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea during 1999–2015. J Gynecol Oncol. 2019; 30:e38.
Article5. Papanicolaou GN, Traut HF. The diagnostic value of vaginal smears in carcinoma of the uterus 1941. Arch Pathol Lab Med. 1997; 121:211–24.6. Kong TW, Kim M, Kim YH, Kim YB, Kim J, Kim JW, et al. High-risk human papillomavirus testing as a primary screening for cervical cancer: position statement by the Korean Society of Obstetrics and Gynecology and the Korean Society of Gynecologic Oncology. J Gynecol Oncol. 2020; 31:e31.
Article7. US Preventive Services Task Force. Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018; 320:674–86.8. Walker EM, Hare MJ, Cooper P. A retrospective review of cervical cytology in women developing invasive squamous cell carcinoma. Br J Obstet Gynaecol. 1983; 90:1087–91.
Article9. Janerich DT, Hadjimichael O, Schwartz PE, Lowell DM, Meigs JW, Merino MJ, et al. The screening histories of women with invasive cervical cancer, Connecticut. Am J Public Health. 1995; 85:791–4.
Article10. Wain GV, Farnsworth A, Hacker NF. The Papanicolaou smear histories of 237 patients with cervical cancer. Med J Aust. 1992; 157:14–6.
Article11. Fahey MT, Irwig L, Macaskill P. Meta-analysis of Pap test accuracy. Am J Epidemiol. 1995; 141:680–9.
Article12. Nanda K, McCrory DC, Myers ER, Bastian LA, Hasselblad V, Hickey JD, et al. Accuracy of the Papanicolaou test in screening for and follow-up of cervical cytologic abnormalities: a systematic review. Ann Intern Med. 2000; 132:810–9.
Article13. Rylander E. Negative smears in women developing invasive cervical cancer. Acta Obstet Gynecol Scand. 1977; 56:115–8.
Article14. Min KJ, Lee YJ, Suh M, Yoo CW, Lim MC, Choi J, et al. The Korean guideline for cervical cancer screening. J Gynecol Oncol. 2015; 26:232–9.
Article15. Solomon D, Davey D, Kurman R, Moriarty A, O’Connor D, Prey M, et al. The 2001 Bethesda system: terminology for reporting results of cervical cytology. JAMA. 2002; 287:2114–9.
Article16. Maruvka YE, Tang M, Michor F. On the validity of using increases in 5-year survival rates to measure success in the fight against cancer. PLoS One. 2014; 9:e83100.
Article17. Rozemeijer K, Naber SK, Penning C, Overbeek LI, Looman CW, de Kok IM, et al. Cervical cancer incidence after normal cytological sample in routine screening using SurePath, ThinPrep, and conventional cytology: population based study. BMJ. 2017; 356:j504.
Article18. Sawaya GF, McConnell KJ, Kulasingam SL, Lawson HW, Kerlikowske K, Melnikow J, et al. Risk of cervical cancer associated with extending the interval between cervical-cancer screenings. N Engl J Med. 2003; 349:1501–9.
Article19. Stenkvist B, Soderstrom J. Reasons for cervical cancer despite extensive screening. J Med Screen. 1996; 3:204–7.
Article20. Philp L, Jembere N, Wang L, Gao J, Maguire B, Kupets R. Pap tests in the diagnosis of cervical cancer: help or hinder? Gynecol Oncol. 2018; 150:61–6.
Article21. DeMay RM. Cytopathology of false negatives preceding cervical carcinoma. Am J Obstet Gynecol. 1996; 175:1110–3.
Article22. Zhao L, Wentzensen N, Zhang RR, Dunn ST, Gold MA, Wang SS, et al. Factors associated with reduced accuracy in Papanicolaou tests for patients with invasive cervical cancer. Cancer Cytopathol. 2014; 122:694–701.
Article23. Krane JF, Granter SR, Trask CE, Hogan CL, Lee KR. Papanicolaou smear sensitivity for the detection of adenocarcinoma of the cervix: a study of 49 cases. Cancer. 2001; 93:8–15.24. Coldman A, Phillips N, Kan L, Matisic J, Benedet L, Towers L. Risk of invasive cervical cancer after three consecutive negative Pap smears. J Med Screen. 2003; 10:196–200.
Article25. Etherington IJ, Luesley DM. Adenocarcinoma in situ of the cervix-controversies in diagnosis and treatment. J Low Genit Tract Dis. 2001; 5:94–8.
Article26. Katki HA, Schiffman M, Castle PE, Fetterman B, Poitras NE, Lorey T, et al. Five-year risks of CIN 3+ and cervical cancer among women who test Pap-negative but are HPV-positive. J Low Genit Tract Dis. 2013; 17(5 Suppl 1):S56–63.27. Hildesheim A, Hadjimichael O, Schwartz PE, Wheeler CM, Barnes W, Lowell DM, et al. Risk factors for rapid-onset cervical cancer. Am J Obstet Gynecol. 1999; 180:571–7.
Article28. Prendiville W, Guillebeaud J, Bamford P, Beilby J, Steele SJ. Carcinoma of cervix with recent normal Papanicolaou tests. Lancet. 1980; 2:853–4.
Article29. Morgan-Jones DV. Misleading exfoliative cytology. Br Med J. 1964; 2:874–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Usefulness of New Cervicography in Screening of Cervical Cancer
- Women's Cancer Screening According to Body Mass Index in a Cohort of Rural Korean Women
- Effect of Pap smears on the long-term survival of cervical cancer patients: a nationwide population-based cohort study in Korea
- Trends in cervical cancer screening rates among Korean women: results of the Korean National Cancer Screening Survey, 2005–2020
- Associations between Smoking, Screening, and Death Caused by Cervical Cancer in Korean Women