Neurointervention.
2021 Jul;16(2):149-157. 10.5469/neuroint.2021.00192.
Long Vascular Sheaths for Transfemoral Neuroendovascular Procedures in Children
- Affiliations
-
- 1Neuroradiology and Image Guided Therapy, Hospital for Sick Children, Toronto, ON, Canada
- 2Department of Neurosurgery, Hospital for Sick Children, Toronto, ON, Canada
- KMID: 2517740
- DOI: http://doi.org/10.5469/neuroint.2021.00192
Abstract
- Purpose
To evaluate the safety and efficacy of long vascular sheaths for transfemoral neuroendovascular procedures in children.
Materials and Methods
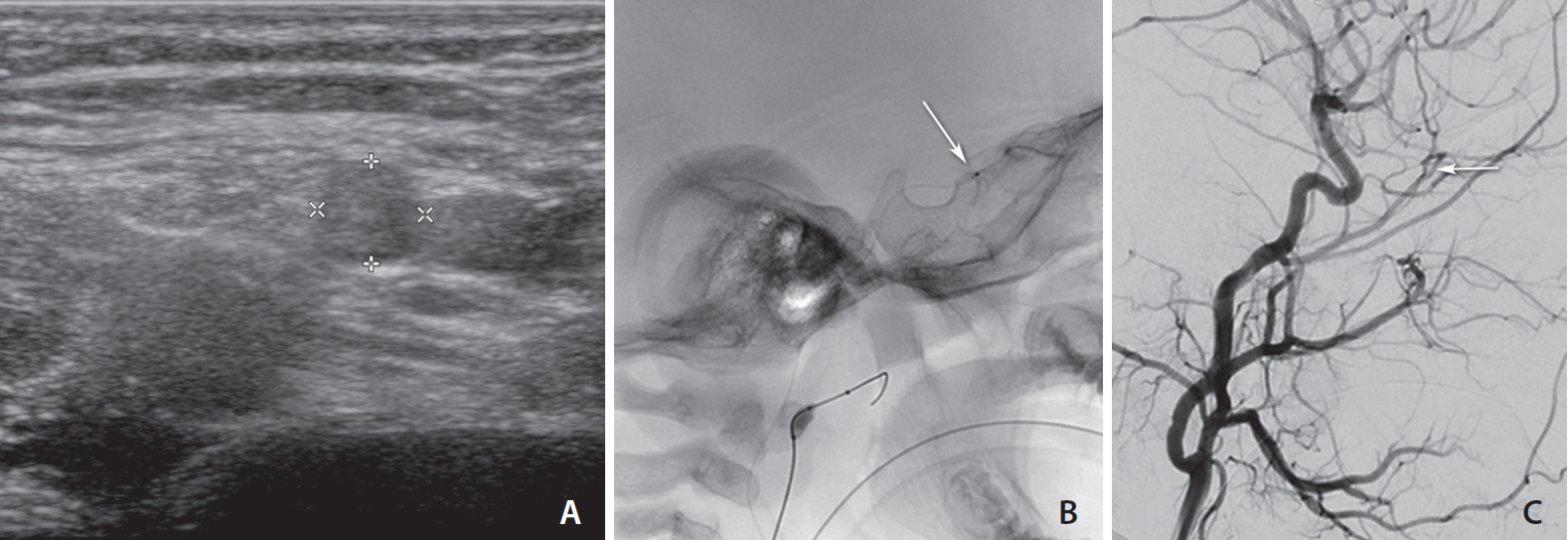
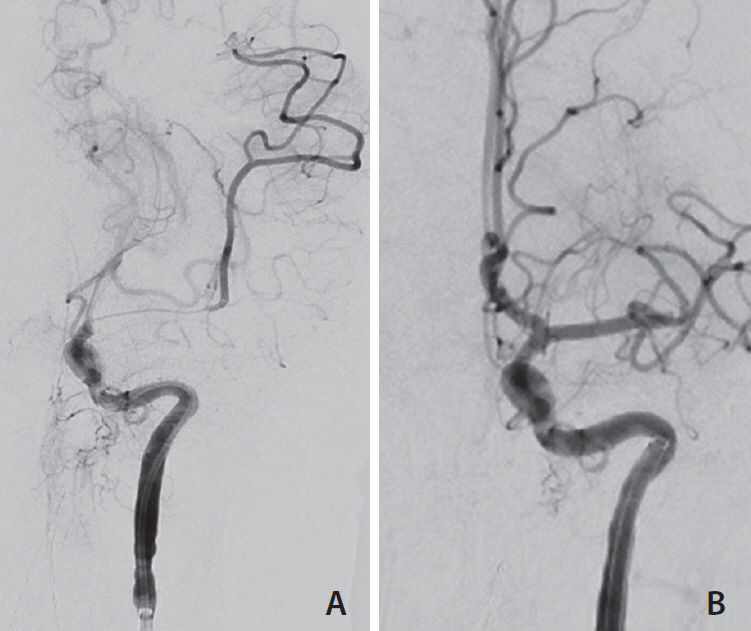
A retrospective evaluation of transfemoral neuroendovascular procedures in children <18 years, using long sheaths was undertaken analyzing procedure type, fluoroscopic times, technical success, access site and systemic complications. Twenty-seven consecutive procedures were included over a two-year period. Mean age was 8.4 years (standard deviation [SD] 6.3) (range 17.0 months–16.3 years).
Results
Patients were 44% female and mean weight was 35.0 kg (SD 22.8) (range 9.8–72.2 kg). A third of the procedures were performed in ≤15 kg children. The most common procedure was for embolization (n=13, 48.1%) and the most common indication was dual microcatheter technique (52%). The most common device used was the 5 Fr Cook Shuttle sheath. Mean fluoroscopy time was 61.9 minutes (SD 43.1). Of these procedures, 93% were technically successful. Femoral vasospasm, when present, was self-limiting. Complications (3/27, 11.1%) included groin hematoma (n=1), neck vessel spasm that resolved with verapamil (n=1), and intracranial thromboembolism (n=1), with no significant difference between the ≤15 kg and >15 kg subcohorts. There were no aorto-femoro-iliac or limb-ischemic complications.
Conclusion
Long vascular sheaths without short femoral sheaths can be safely used for pediatric neuroendovascular procedures as they effectively increase inner diameter access without increasing the outer sheath diameter. This property increases the range of devices used and intracranial techniques that can be safely performed without arterial compromise, thus increasing the repertoire of the neurointerventionist.
Keyword
Figure
Reference
-
1. Chewning R, Wyse G, Murphy K. Neurointervention for the peripheral radiologist: tips and tricks. Semin Intervent Radiol. 2008; 25:42–47.
Article2. Daehnert I, Rotzsch C, Wiener M, Schneider P. Rapid right ventricular pacing is an alternative to adenosine in catheter interventional procedures for congenital heart disease. Heart. 2004; 90:1047–1050.
Article3. Ding L, Pockett C, Moore J, El-Said H. Long sheath use in femoral artery catheterizations in infants <15 kg is associated with a higher thrombosis rate: proposed protocol for detection and management. Catheter Cardiovasc Interv. 2016; 88:1108–1112.4. Alaraj A, Wallace A, Dashti R, Patel P, Aletich V. Balloons in endovascular neurosurgery: history and current applications. Neurosurgery. 2014; 74 Suppl 1:S163–S190.5. Varadharajan S, Ramalingaiah AH, Saini J, Gupta AK, Devi BI, Acharya UV. Precipitating hydrophobic injectable liquid embolization of intracranial vascular shunts: initial experience and technical note. J Neurosurg. 2018; 129:1217–1222.
Article6. Szajner M, Roman T, Markowicz J, Szczerbo-Trojanowska M. Onyx® in endovascular treatment of cerebral arteriovenous malformations - a review. Pol J Radiol. 2013; 78:35–41.
Article7. Chapot R, Stracke P, Velasco A, Nordmeyer H, Heddier M, Stauder M, et al. The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol. 2014; 41:87–91.
Article8. Ashour R, Aziz-Sultan MA, Soltanolkotabi M, Schoeneman SE, Alden TD, Hurley MC, et al. Safety and efficacy of onyx embolization for pediatric cranial and spinal vascular lesions and tumors. Neurosurgery. 2012; 71:773–784.
Article9. Vollherbst DF, Sommer CM, Ulfert C, Pfaff J, Bendszus M, Möhlenbruch MA. Liquid embolic agents for endovascular embolization: evaluation of an established (Onyx) and a novel (PHIL) embolic agent in an in vitro AVM model. AJNR Am J Neuroradiol. 2017; 38:1377–1382.
Article10. Gross BA, Du R. Diagnosis and treatment of vascular malformations of the brain. Curr Treat Options Neurol. 2014; 16:279.
Article11. Paramasivam S, Toma N, Niimi Y, Berenstein A. Development, clinical presentation and endovascular management of congenital intracranial pial arteriovenous fistulas. J Neurointerv Surg. 2013; 5:184–190.
Article12. Rosen RJ, Contractor S. The use of cyanoacrylate adhesives in the management of congenital vascular malformations. Semin Intervent Radiol. 2004; 21:59–66.
Article13. Ishikawa M, Horikawa M, Yamagami T, Uchida BT, Awai K, Kaufman JA. Embolization of arteriovenous malformations: effect of flow control and composition of n-butyl-2 cyanoacrylate and iodized oil mixtures with and without ethanol in an in vitro model. Radiology. 2016; 279:910–916.14. ApSimon HT, Hartley DE. Embolization of small vessels with a double-lumen microballoon catheter. Part I: design and construction. Radiology. 1984; 151:55–57.
Article15. Lopera JE. Embolization in trauma: principles and techniques. Semin Intervent Radiol. 2010; 27:14–28.
Article16. Kim DJ, Suh DC, Kim BM, Kim DI. Adjuvant coil assisted glue embolization of vein of galen aneurysmal malformation in pediatric patients. Neurointervention. 2018; 13:41–47.
Article17. Kwon OK, Kim SH, Kwon BJ, Kang HS, Kim JH, Oh CW, et al. Endovascular treatment of wide-necked aneurysms by using two microcatheters: techniques and outcomes in 25 patients. AJNR Am J Neuroradiol. 2005; 26:894–900.18. Chueh JY, Kühn AL, Puri AS, Wilson SD, Wakhloo AK, Gounis MJ. Reduction in distal emboli with proximal flow control during mechanical thrombectomy: a quantitative in vitro study. Stroke. 2013; 44:1396–1401.19. Mokin M, Setlur Nagesh SV, Ionita CN, Levy EI, Siddiqui AH. Comparison of modern stroke thrombectomy approaches using an in vitro cerebrovascular occlusion model. AJNR Am J Neuroradiol. 2015; 36:547–551.
Article20. Chueh JY, Puri AS, Wakhloo AK, Gounis MJ. Risk of distal embolization with stent retriever thrombectomy and ADAPT. J Neurointerv Surg. 2016; 8:197–202.
Article21. Hoffman CE, Santillan A, Rotman L, Gobin YP, Souweidane MM. Complications of cerebral angiography in children younger than 3 years of age. J Neurosurg Pediatr. 2014; 13:414–419.
Article22. Lin N, Smith ER, Scott RM, Orbach DB. Safety of neuroangiography and embolization in children: complication analysis of 697 consecutive procedures in 394 patients. J Neurosurg Pediatr. 2015; 16:432–438.
Article23. Alexander J, Yohannan T, Abutineh I, Agrawal V, Lloyd H, Zurakowski D, et al. Ultrasound-guided femoral arterial access in pediatric cardiac catheterizations: a prospective evaluation of the prevalence, risk factors, and mechanism for acute loss of arterial pulse. Catheter Cardiovasc Interv. 2016; 88:1098–1107.
Article24. Glatz AC, Shah SS, McCarthy AL, Geisser D, Daniels K, Xie D, et al. Prevalence of and risk factors for acute occlusive arterial injury following pediatric cardiac catheterization: a large single-center cohort study. Catheter Cardiovasc Interv. 2013; 82:454–462.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Protocols and Results of Resident Neurosurgeon's Transfemoral Catheter Angiography Training Supervised by Neuroendovascular Specialists
- Ultrasonographic evaluation of complications related to transfemoral arterial procedures
- Anatomical Aspect of the Transfemoral Neuroendovascular Approach
- Surgical Management of Arterial Restenosis
- Transradial Interventions in Coronary Artery Disease: Comparison with Transfemoral Interventions