J Korean Neurosurg Soc.
2013 Aug;54(2):81-85. 10.3340/jkns.2013.54.2.81.
Protocols and Results of Resident Neurosurgeon's Transfemoral Catheter Angiography Training Supervised by Neuroendovascular Specialists
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Soonchunhyang University, Bucheon Hospital, Bucheon, Korea. bumtkim@schmc.ac.kr
- 2Department of Neurosurgery, College of Medicine, Soonchunhyang University, Seoul, Korea.
- KMID: 1814242
- DOI: http://doi.org/10.3340/jkns.2013.54.2.81
Abstract
OBJECTIVE
Transfemoral catheter angiography (TFCA) is a basic procedure in neurovascular surgery with increasing importance in surgical and non-invasive treatments. Unfortunately, resident neurosurgeons have relatively few opportunities to perform TFCA in most institutions. We report a method developed in our hospital for training resident neurosurgeons to perform TFCA and evaluate the efficacy of this training.
METHODS
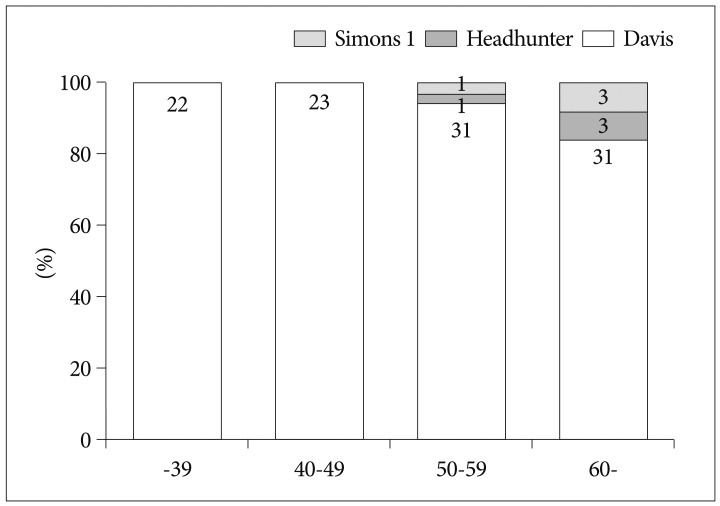
From May 2011 to September 2011, a total of 112 consecutive patients underwent TFCA by one resident neurosurgeon supervised by two neuroendovascular specialists. Patients who underwent elective diagnostic procedures were included in this study. Patients who underwent endovascular treatment were excluded. Demographic data, indications for TFCA, side of approach, number of selected arteries, and complications were analyzed.
RESULTS
This study included 64 males and 48 females with a mean age of 51.6 (12-81) years. All procedures were performed in the angiography suite. Common indications for procedures were as follows: stroke-induced symptoms in 61 patients (54.5%), Moyamoya disease and arteriovenous malformation in 13 patients (11.6%), and unruptured intracranial aneurysm in eight patients (7.1%). Right and left femoral puncture was performed in 98.2% and 1.8% of patients, respectively. A total of 465 selective angiographies were performed without complications. Angiographic examination was performed on 4.15 vessels per patient.
CONCLUSION
TFCA can be performed safely by resident neurosurgeons based on anatomical study and a meticulous protocol under the careful supervision of neuroendovascular specialists.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Cerebral Angiography: The First Small Step for the Neurointerventionist
Jae Ho Shin
Neurointervention. 2020;15(2):101-103. doi: 10.5469/neuroint.2020.00101.
Reference
-
1. American Society of Interventional and Therapeutic Neuroradiology. General considerations for endovascular surgical neuroradiologic procedures. AJNR Am J Neuroradiol. 2001; 22(8 Suppl):S1–S3. PMID: 11686064.2. Barr JD, Connors JJ 3rd, Sacks D, Wojak JC, Becker GJ, Cardella JF, et al. Quality improvement guidelines for the performance of cervical carotid angioplasty and stent placement. AJNR Am J Neuroradiol. 2003; 24:2020–2034. PMID: 14625227.
Article3. Cerebral arteriography. A report for health professionals by the Executive Committee of the Stroke Council, American Heart Association. Circulation. 1989; 79:474. PMID: 2914360.4. Connors JJ 3rd, Sacks D, Furlan AJ, Selman WR, Russell EJ, Stieg PE, et al. Training, competency, and credentialing standards for diagnostic cervicocerebral angiography, carotid stenting, and cerebrovascular intervention. AJNR Am J Neuroradiol. 2004; 25:1732–1741. PMID: 15569739.
Article5. Crawley F, Stygall J, Lunn S, Harrison M, Brown MM, Newman S. Comparison of microembolism detected by transcranial Doppler and neuropsychological sequelae of carotid surgery and percutaneous transluminal angioplasty. Stroke. 2000; 31:1329–1334. PMID: 10835452.
Article6. Harbaugh RE, Agarwal A. Training residents in endovascular neurosurgery. Neurosurgery. 2006; 59(5 Suppl 3):S277–S281. discussion S3-S13. PMID: 17053613.
Article7. Heiserman JE, Dean BL, Hodak JA, Flom RA, Bird CR, Drayer BP, et al. Neurologic complications of cerebral angiography. AJNR Am J Neuroradiol. 1994; 15:1401–1407. discussion 1408-1411. PMID: 7985557.8. Higashida RT, Hopkins LN, Berenstein A, Halbach VV, Kerber C. Program requirements for residency/fellowship education in neuroendovascular surgery/interventional neuroradiology: a special report on graduate medical education. AJNR Am J Neuroradiol. 2000; 21:1153–1159. PMID: 10871032.9. Howington JU, Hopkins LN, Piepgras DG, Harbaugh RE. Training standards in endovascular neurosurgery. Neurosurg Clin N Am. 2005; 16:445–449. xiPMID: 15694173.
Article10. Johnston DC, Chapman KM, Goldstein LB. Low rate of complications of cerebral angiography in routine clinical practice. Neurology. 2001; 57:2012–2014. PMID: 11739818.11. Kim BT, Shin DS. Anatomical aspect of the transfemoral neuroendovascular approach. Neurointervention. 2010; 5:79–84.
Article12. Mani RL, Eisenberg RL. Complications of catheter cerebral arteriography: analysis of 5,000 procedures. II. Relation of complication rates to clinical and arteriographic diagnoses. AJR Am J Roentgenol. 1978; 131:867–869. PMID: 101046.
Article13. Mani RL, Eisenberg RL. Complications of catheter cerebral arteriography: analysis of 5,000 procedures. III. Assessment of arteries injected, contrast medium used, duration of procedure, and age of patient. AJR Am J Roentgenol. 1978; 131:871–874. PMID: 101047.
Article14. Mani RL, Eisenberg RL, McDonald EJ Jr, Pollock JA, Mani JR. Complications of catheter cerebral arteriography: analysis of 5,000 procedures. I. Criteria and incidence. AJR Am J Roentgenol. 1978; 131:861–865. PMID: 101045.
Article15. Moran CJ, Milburn JM, Cross DT 3rd, Derdeyn CP, Dobbie TK, Littenberg B. Randomized controlled trial of sheaths in diagnostic neuroangiography. Radiology. 2001; 218:183–187. PMID: 11152799.
Article16. Picard L, Negoro M, Ter Brugge K, Mawad M, Lasjaunias P, Viñuela F, et al. 1998 world Federation of interventional and therapeutic neuroradiology. Guidelines for fellowship training programmes in interventional neuroradiology. Interv Neuroradiol. 1998; 4:195–197. PMID: 20673410.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Educational Status of Internal Medicine Residency Program in Korea
- Suggestions for the Development of Education Guideline for Abdominal US Education Specialists
- Long Vascular Sheaths for Transfemoral Neuroendovascular Procedures in Children
- Efficient utilization of the limited number of emergency medicine specialists and statistics related to clinical outcomes in the emergency department
- Preoperative Transfemoral Catheter Embolization in a Torcular Meningioma