Neurointervention.
2021 Jul;16(2):141-148. 10.5469/neuroint.2021.00150.
Impact of Intravenous Aspirin Administration on Ventriculostomy-Associated Hemorrhage in Coiled Acute Subarachnoid Hemorrhage Patients
- Affiliations
-
- 1Department of Neuroradiology, North Bristol NHS Trust, Bristol, UK
- 2Department of Neurosurgery, North Bristol NHS Trust, Bristol, UK
- KMID: 2517739
- DOI: http://doi.org/10.5469/neuroint.2021.00150
Abstract
- Purpose
Aspirin has beneficial effects on coiling, even in acute subarachnoid hemorrhage, but there is also a perceived risk of increased bleeding and, importantly, a concern regarding ventriculostomy-associated hemorrhage (VAH) in those with complicating hydrocephalus. We aimed to assess the rate and extent of VAH in patients specifically treated with procedural intravenous aspirin during endovascular coiling of ruptured intracranial aneurysms.
Materials and Methods
This was a single neurovascular center retrospective observational study of consecutive patients treated over a three-year period. The rate of VAH assessed using computed tomography and clinical outcomes were compared in patients receiving intraprocedural intravenous aspirin loading (n=90) versus those that did not receive the drug (n=40).
Results
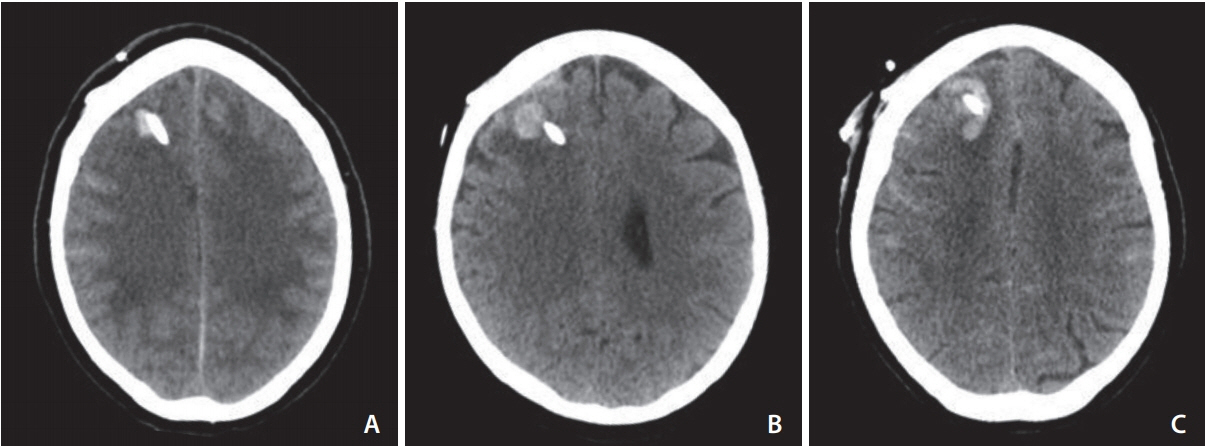
There was a significantly elevated rate of VAH in patients receiving intravenous aspirin (30% vs. 2.5%, odds ratio 16.7 [95% confidence interval: 2.2–128.0], P<0.0001). The majority of VAH was <10 mm in size (70%) with the largest bleed measuring 20 mm. No hematoma required surgical evacuation. No difference in favorable outcome at discharge was demonstrated. There was no difference in mortality between the 2 groups.
Conclusion
Loading with intravenous aspirin during endovascular treatment of ruptured intracranial aneurysms significantly increases the risk of VAH, but most are small with minimal impact on clinical outcome at discharge. Intravenous aspirin should probably be reserved for selected cases but should not be withheld based on risk of VAH.
Keyword
Figure
Reference
-
1. Edwards NJ, Jones WH, Sanzgiri A, Corona J, Dannenbaum M, Chen PR. Antiplatelet therapy for the prevention of peri-coiling thromboembolism in high-risk patients with ruptured intracranial aneurysms. J Neurosurg. 2017; 127:1326–1332.
Article2. Ries T, Buhk JH, Kucinski T, Goebell E, Grzyska U, Zeumer H, et al. Intravenous administration of acetylsalicylic acid during endovascular treatment of cerebral aneurysms reduces the rate of thromboembolic events. Stroke. 2006; 37:1816–1821.
Article3. van den Bergh WM; MASH Study Group, Algra A, Dorhout Mees SM, van Kooten F, Dirven CM, van Gijn J, et al. Randomized controlled trial of acetylsalicylic acid in aneurysmal subarachnoid hemorrhage: the MASH study. Stroke. 2006; 37:2326–2330.4. Cagnazzo F, Derraz I, Lefevre PH, Gascou G, Dargazanli C, Riquelme C, et al. Antiplatelet therapy in patients with aneurysmal SAH: impact on delayed cerebral ischemia and clinical outcome. A meta-analysis. AJNR Am J Neuroradiol. 2019; 40:1201–1206.
Article5. Ditz C, Machner B, Schacht H, Neumann A, Schramm P, Tronnier VM, et al. Effects of post-interventional antiplatelet therapy on angiographic vasospasm, delayed cerebral ischemia, and clinical outcome after aneurysmal subarachnoid hemorrhage: a single-center experience. [published online ahead of print Jan 25, 2021] Neurosurg Rev 2021.6. Parkhutik V, Lago A, Tembl JI, Rubio C, Fuset MP, Vallés J, et al. Influence of COX-inhibiting analgesics on the platelet function of patients with subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2012; 21:755–759.
Article7. Meves SH, Neubauer H, Overbeck U, Endres HG. Is there an ideal way to initiate antiplatelet therapy with aspirin? A crossover study on healthy volunteers evaluating different dosing schemes with whole blood aggregometry. BMC Res Notes. 2011; 4:106.
Article8. Bechan RS, Sprengers ME, Majoie CB, Peluso JP, Sluzewski M, van Rooij WJ. Stent-assisted coil embolization of intracranial aneurysms: complications in acutely ruptured versus unruptured aneurysms. AJNR Am J Neuroradiol. 2016; 37:502–507.
Article9. Cagnazzo F, Di Carlo DT, Petrella G, Perrini P. Ventriculostomy-related hemorrhage in patients on antiplatelet therapy for endovascular treatment of acutely ruptured intracranial aneurysms. A meta-analysis. Neurosurg Rev. 2020; 43:397–406.
Article10. Gardner PA, Engh J, Atteberry D, Moossy JJ. Hemorrhage rates after external ventricular drain placement. J Neurosurg. 2009; 110:1021–1025.
Article11. Maniker AH, Vaynman AY, Karimi RJ, Sabit AO, Holland B. Hemorrhagic complications of external ventricular drainage. Neurosurgery. 2006; 59(4 Suppl 2):ONS41–424; discussion ONS424-425.
Article12. Sussman ES, Kellner CP, Nelson E, McDowell MM, Bruce SS, Bruce RA, et al. Hemorrhagic complications of ventriculostomy: incidence and predictors in patients with intracerebral hemorrhage. J Neurosurg. 2014; 120:931–936.
Article13. Müller A, Mould WA, Freeman WD, McBee N, Lane K, Dlugash R, CLEAR investigators, et al. The incidence of catheter tract hemorrhage and catheter placement accuracy in the clear III trial. Neurocrit Care. 2018; 29:23–32.
Article14. Hudson JS, Prout BS, Nagahama Y, Nakagawa D, Guerrero WR, Zanaty M, et al. External ventricular drain and hemorrhage in aneurysmal subarachnoid hemorrhage patients on dual antiplatelet therapy: a retrospective cohort study. Neurosurgery. 2019; 84:479–484.
Article15. Qin G, Pang G, Zhong S, Chen H, Tang X, Lan S. Increased risk of ventriculostomy-associated hemorrhage in patients treated with antiplatelet agents for stent-assisted coiling of ruptured intracranial aneurysms. Br J Neurosurg. 2021; 35:270–274.
Article16. Bruder M, Schuss P, Konczalla J, El-Fiki A, Lescher S, Vatter H, et al. Ventriculostomy-related hemorrhage after treatment of acutely ruptured aneurysms: the influence of anticoagulation and antiplatelet treatment. World Neurosurg. 2015; 84:1653–1659.
Article17. Majmundar N, Sarris C, Shastri D, Doran J, Gandhi C, Assina R. Hemorrhagic complications of external ventriculostomy in the aspirin and P2Y12 response assay era. World Neurosurg. 2019; 122:e961–e968.
Article18. van den Bergh WM, Algra A, Rinkel GJ; MASH Study Group. Magnesium and aspirin treatment in patients with subarachnoid haemorrhage. Comparison of effects after endovascular and neurosurgical aneurysm occlusion. J Neurol. 2009; 256:213–216.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Intravenous Administration of Nimodipine on Cerebral Pial Vessels after Experimental Subarachnoid Hemorrhage in Rabbits
- Efficacy and Rebleeding Risk of Preoperative Ventriculostomy in Aneurysmal Subarachnoid Hemorrhage
- Brain Injuries during Intraoperative Ventriculostomy in the Aneurysmal Subarachnoid Hemorrhage Patients
- Influence of Intraoperative Ventriculostomy on the Occurrence of Shunt-Dependent Hydrocephalus in Aneurysmal Subarachnoid Hemorrhage
- External Ventricular Drainage System with Long Subcutaneous Tunnel