J Korean Acad Oral Health.
2021 Jun;45(2):87-91. 10.11149/jkaoh.2021.45.2.87.
Antibacterial effect of mouthwash containing CPC against dental caries caused bacteria
- Affiliations
-
- 1Department of Preventive Dentistry, College of Dentistry, Dankook University, Cheonan, Korea
- 2Aekyung Industrial Co., Ltd. R&D Division Dental Care Team, Daejeon, Korea
- KMID: 2517234
- DOI: http://doi.org/10.11149/jkaoh.2021.45.2.87
Abstract
Objectives
The purpose of this study was to evaluate and report the antibacterial efficacy in relation to oral disease-causing bacteria using a mouthwash containing 0.05% CPC in an in vitro test.
Methods
The sterilization test and susceptibility assay of mouthwash containing 0.05% CPC were investigated against Streptococcus mutans, Streptococcus sobrinus, and Lactobacillus acidophilus; Streptococcus sanguinis as oral bacteria related to dental caries; Enterococcus faecalis as apical periodontitis-related bacteria; and Actinomyces israelii, Aggregatibacter actinomycetemcomitans, Fusobacterium nucleatum, Prevotella intermedia, Prevotella nigrescence, Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola, and Filifactor alocis as periodontal disease-related bacteria.
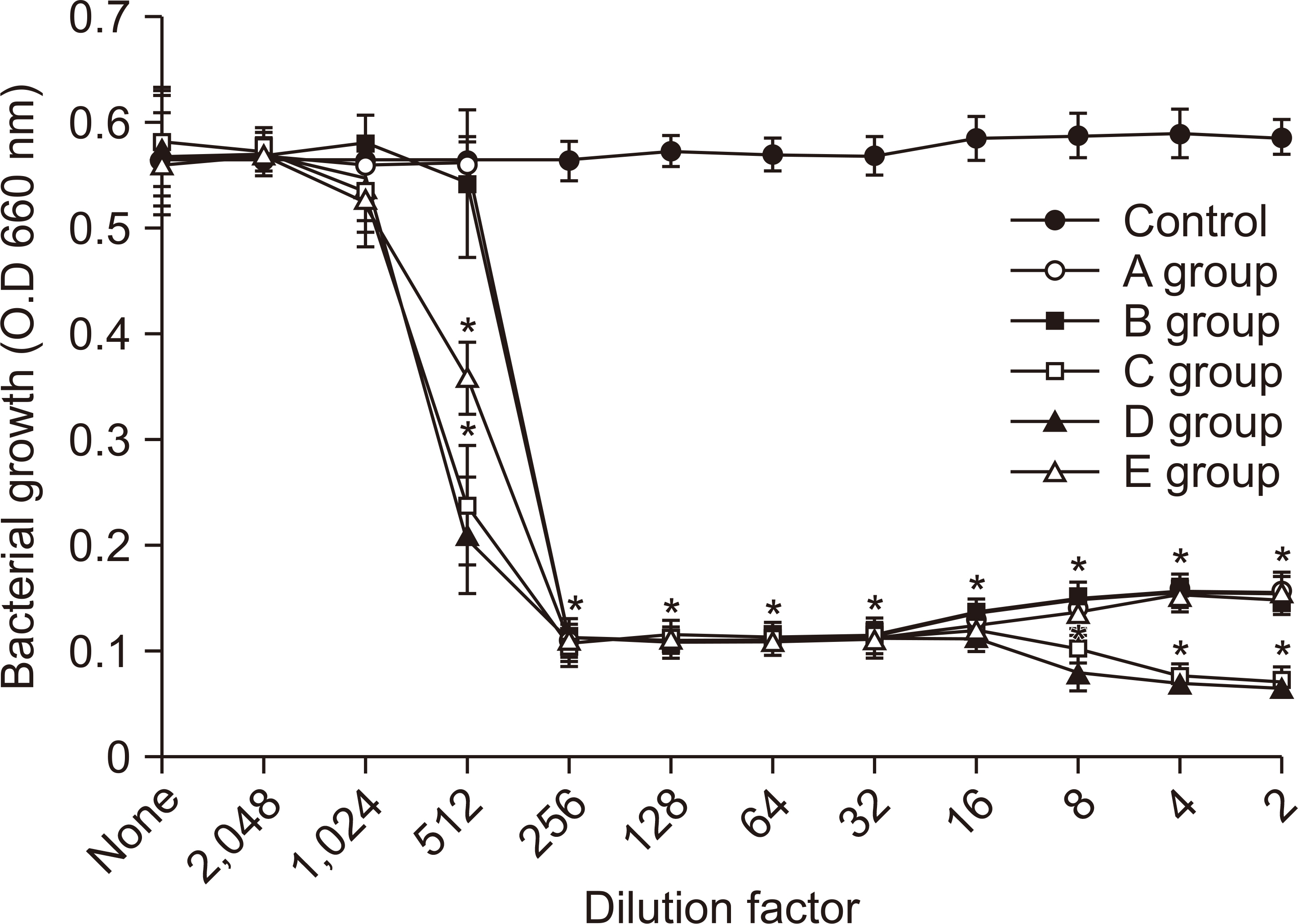
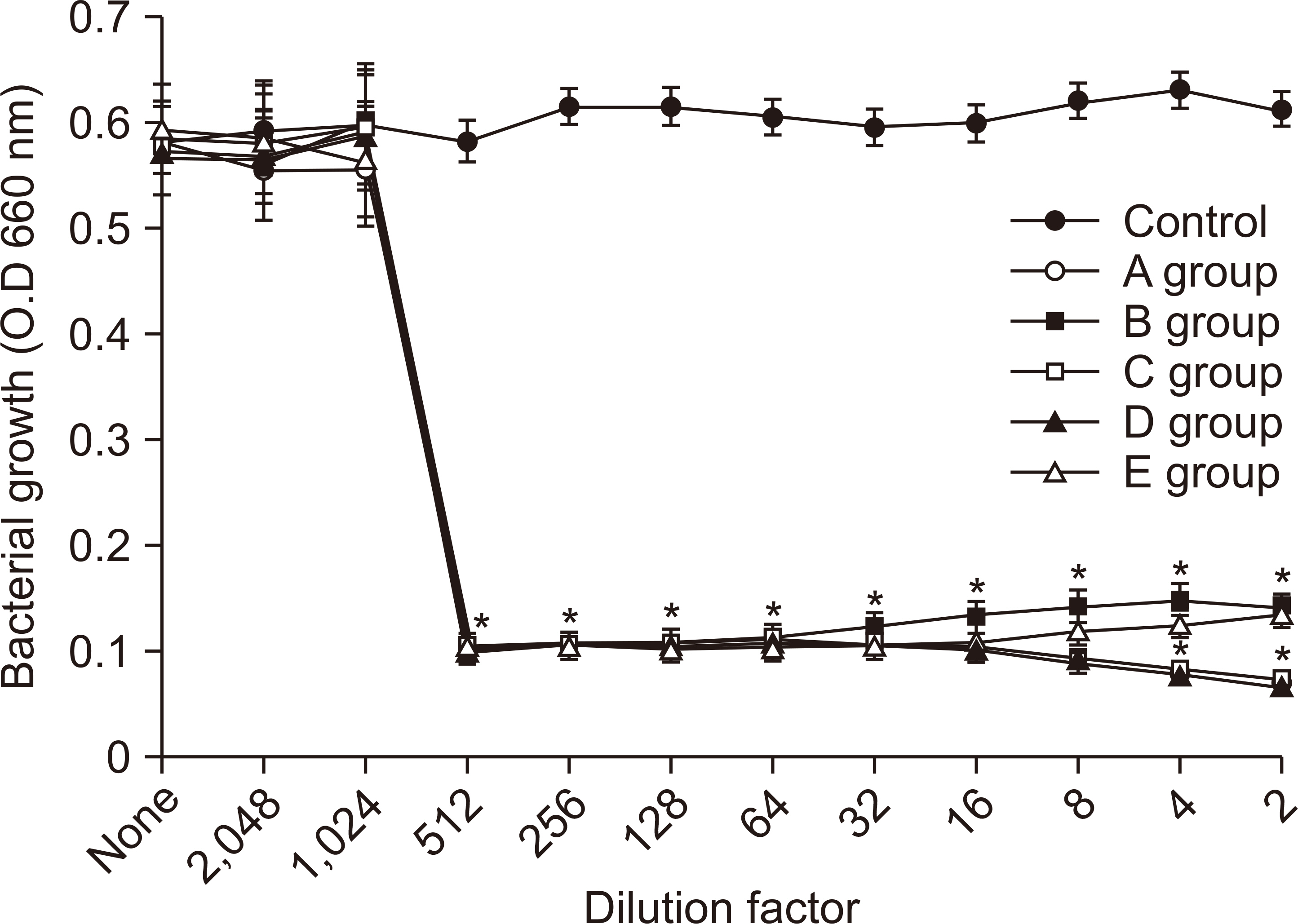
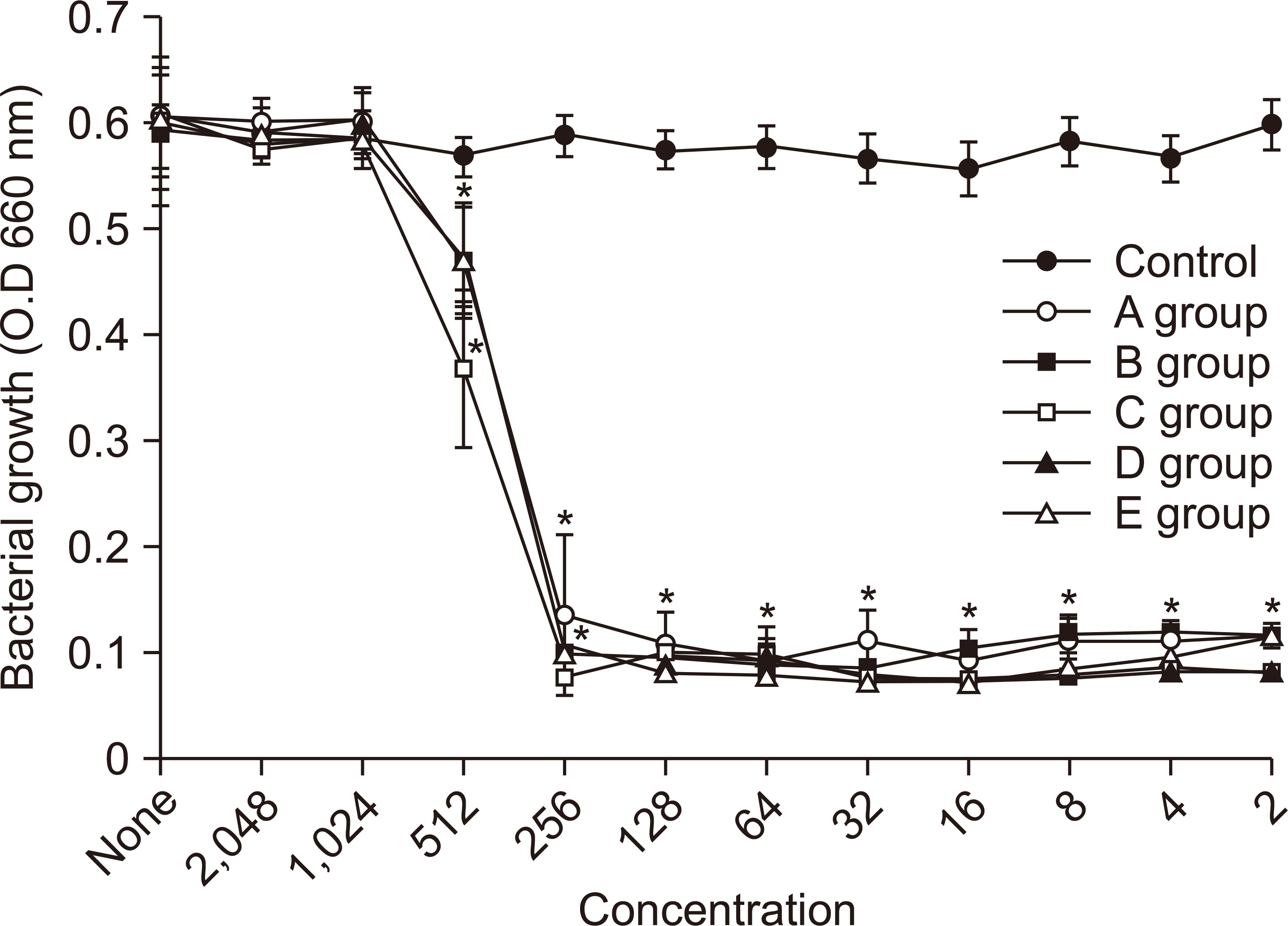
Results
In the sterilization test, most of the bacteria had more than 99.99% sterilizing power for all samples but compared to other bacteria, the sterilizing power of these samples was not successful for L. acidophilus and E. faecalis bacteria. When comparing the sterilization power between the samples, sample 3 (0.05% CPC+20% ethanol) was the strongest.
Conclusions
In the antimicrobial activity test, sample 3 inhibited growth at the lowest concentration overall.
Figure
Reference
-
References
1. ten Cate JM. 2006; Biofilms, a new approach to the microbiology of dental plaque. Odontology. 94:1–9. DOI: 10.1007/s10266-006-0063-3. PMID: 16998612.
Article2. Hamada S, Koga T, Ooshima T. 1984; Virulence factors of Streptococcus mutans and dental caries prevention. J Dent Res. 63:407–411. DOI: 10.1177/00220345840630031001. PMID: 6230378.3. Loesche WJ. 1986; Role of Streptococcus mutans in human dental decay. Microbiol Rev. 50:353–380. DOI: 10.1128/mr.50.4.353-380.1986. PMID: 3540569. PMCID: PMC373078.4. Kim TI, Choi EJ, Chung CP, Han SB, Ku Y. 2002; Antimicorbial effect of Zea Mays L. and Magnoliae cortex extract mixtures on periodontal pathogen and effect on human gingival fibroblast cellular activity. J Korean Acad Periodontol. 32:249–255. DOI: 10.5051/jkape.2002.32.1.249.
Article5. Lee ES. 2011; Inhibitory effects of several commercial oral rinses on Streptococcus mutans biofilm formation. J Korean Acad Dent Health. 35:289–296.6. Shin SC, Lee H. 1998; Clinical study of mouth rinse containing sodium fluoride, cetylpyridinium chloride and urusodesoxycholinic acid on dental plaque and gingivitis. J Korean Acad Dent Health. 22:121–134.7. Gunsolley JC. 2010; Clinical efficacy of antimicrobial mouthrinses. J Dent. 38:6–10. DOI: 10.1016/S0300-5712(10)70004-X. PMID: 20621242.
Article8. Bames GP, Roberts DW, Katz RV, Woolridege ED. 1976; Effects of two cetylpyridinium chloride-containing mouthwashes on bacterial plaque. J Periodontol. 47:419–422. DOI: 10.1902/jop.1976.47.7.419. PMID: 1065740.9. Fardal O, Tumbull RS. 1986; A review of the literature on use of chlorhexidine in dentistry. J Am Dent Assoc. 112:863–869. DOI: 10.14219/jada.archive.1986.0118. PMID: 2940282.10. Garcia-Godoy F, Klukowska MA, Zhang YH, Anastasia K, Cheng R, Gabbard M, et al. 2014; Comparative bioavailability and antimicrobial activity of cetylpyridinium chloride mouthrinses in vitro and in vivo. Am J Dent. 27:185–190. PMID: 25831600.11. Sreenivasan PK, Haraszthy VI, Zambon JJ. 2013; Antimicrobial efficacy of 0.05% cetylpyridinium chloride mouthrinses. Lett Appl Microbiol. 56:14–20. DOI: 10.1111/lam.12008. PMID: 23039819.
Article12. James P, Worthington HV, Parnell C, Harding M, Lamont T, Cheung A, Whelton H, Riley P. 2017; Chlorhexidine mouthrinse as an adjunctive treatment for gingival health. Cochrane Database Syst Rev. 3:CD008676. DOI: 10.1002/14651858.CD008676.pub2. PMID: 28362061. PMCID: PMC6464488.
Article13. Haps S, Slot DE, Berchier CE, Van der Weijden GA. 2008; The effect of cetylpyridinium chloride-containing mouth rinses as adjuncts to toothbrushing on plaque and parameters of gingival inflammation: a systematic review. Int J Dent Hyg. 6:290–303. DOI: 10.1111/j.1601-5037.2008.00344.x. PMID: 19138180.
Article14. Linka WA, Golenia E, Zgoda MM, Kołodziejczyk MK. 2014; The use of semi-synthetic polymers in the formulation of sucking and chewable tablets containing sage extract and zinc gluconate. Polim Med. 44:237–245. PMID: 25932905.15. Fardal O, Tumbull RS. 1986; A review of the literature on use of chlorhexidine in dentistry. J Am Dent Assoc. 112:863–869. DOI: 10.14219/jada.archive.1986.0118. PMID: 2940282.16. Mandel ID. 1988; Chemotherapeutic agents for controlling plaque and gingivitis. J Clin Periodontol. 15:488. DOI: 10.1111/j.1600-051X.1988.tb01020.x. PMID: 3053790.
Article17. Llewelyn J. 1980; A double-blind crossover trial on the effect of cetylpyridinium chloride 0.05 per cent (Merocet) on plaque accumulation. Br Dent J. 148:103–104. DOI: 10.1038/sj.bdj.4804396. PMID: 6986884.
Article18. Kim CY, Kang MS, Kim HG, Kwon HK. 1995; A study on the effects of cetylpyridinium chloride and bamboo salt containing mouthrinses on the inhibition of gingivitis. J Korean Acad Dent Health. 19:219–228.19. Lim K, Mustapha A. 2007; Inhibition of Escherichia coli O157:H7, Listeria monocytogenes and Staphylococcus aureus on sliced roast beef by cetylpyridinium chloride and acidified sodium chlorite. Food Microbiol. 24:89–94. DOI: 10.1016/j.fm.2006.04.005. PMID: 16943099.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical evaluation of cetylpyridinium chloride-containing mouthwash in halitosis
- Destabilizing effect of glycyrrhetinic acid on pre-formed biofilms of Streptococcus mutans
- Antimicrobial Effect of Low Temperature Atmospheric Plasma against Oral Pathogens
- Antibacterial Activity of Hydrogen-rich Water Against Oral Bacteria
- Antibacterial effect of different concentrations of Galla Chinensis extract on cariogenic bacteria in a biofilm model