J Cerebrovasc Endovasc Neurosurg.
2021 Jun;23(2):136-144. 10.7461/jcen.2021.E2020.10.005.
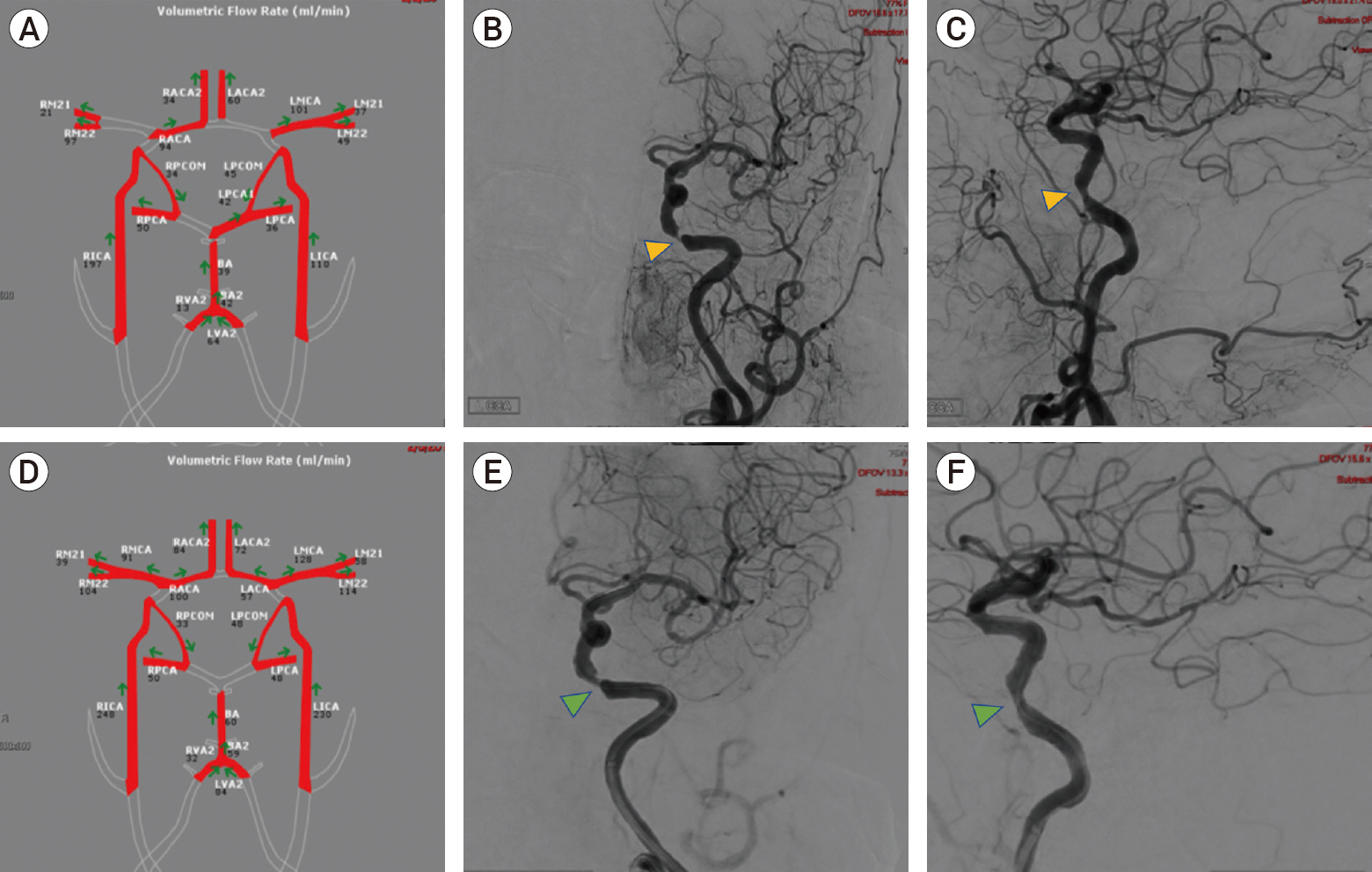
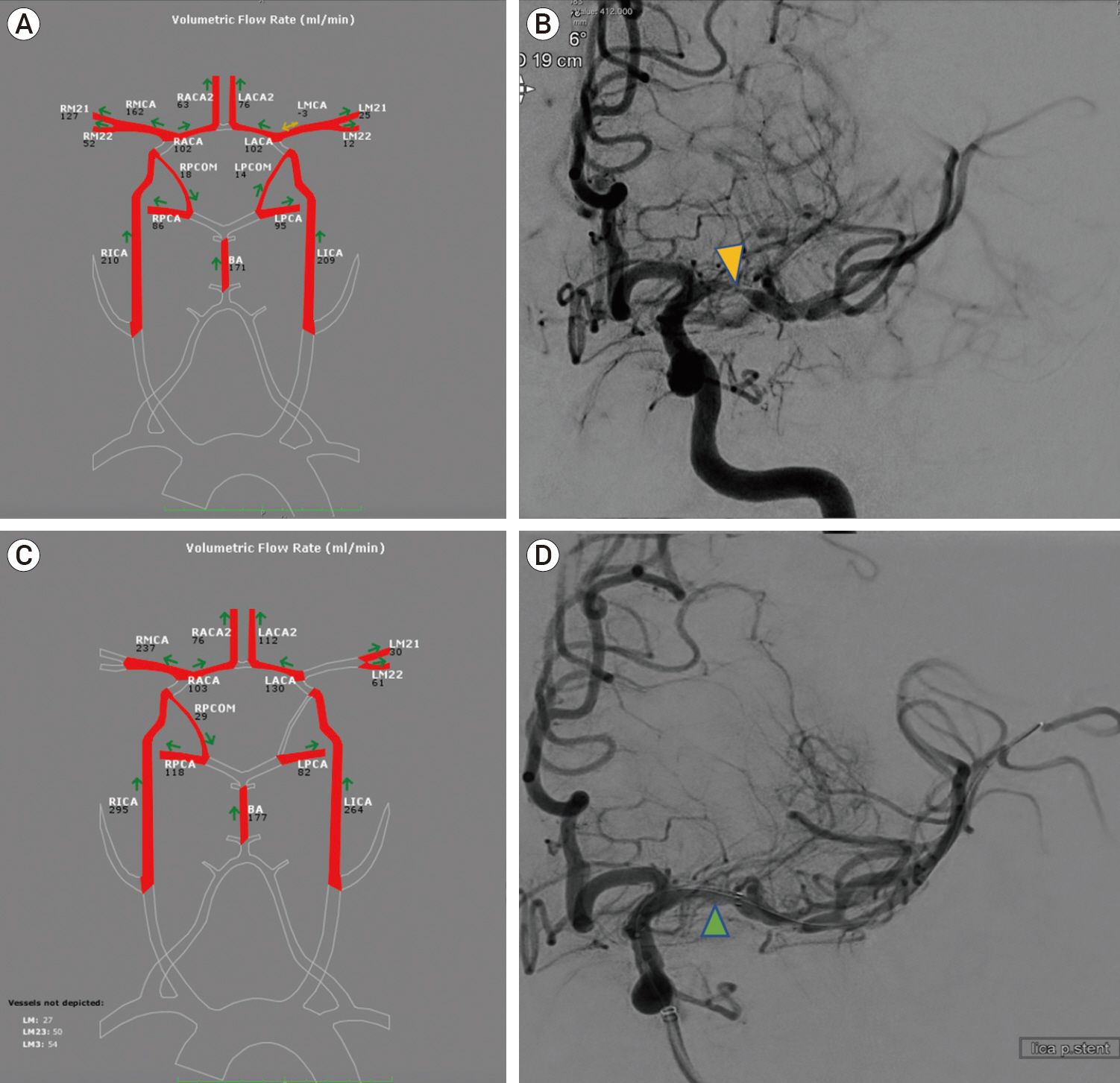
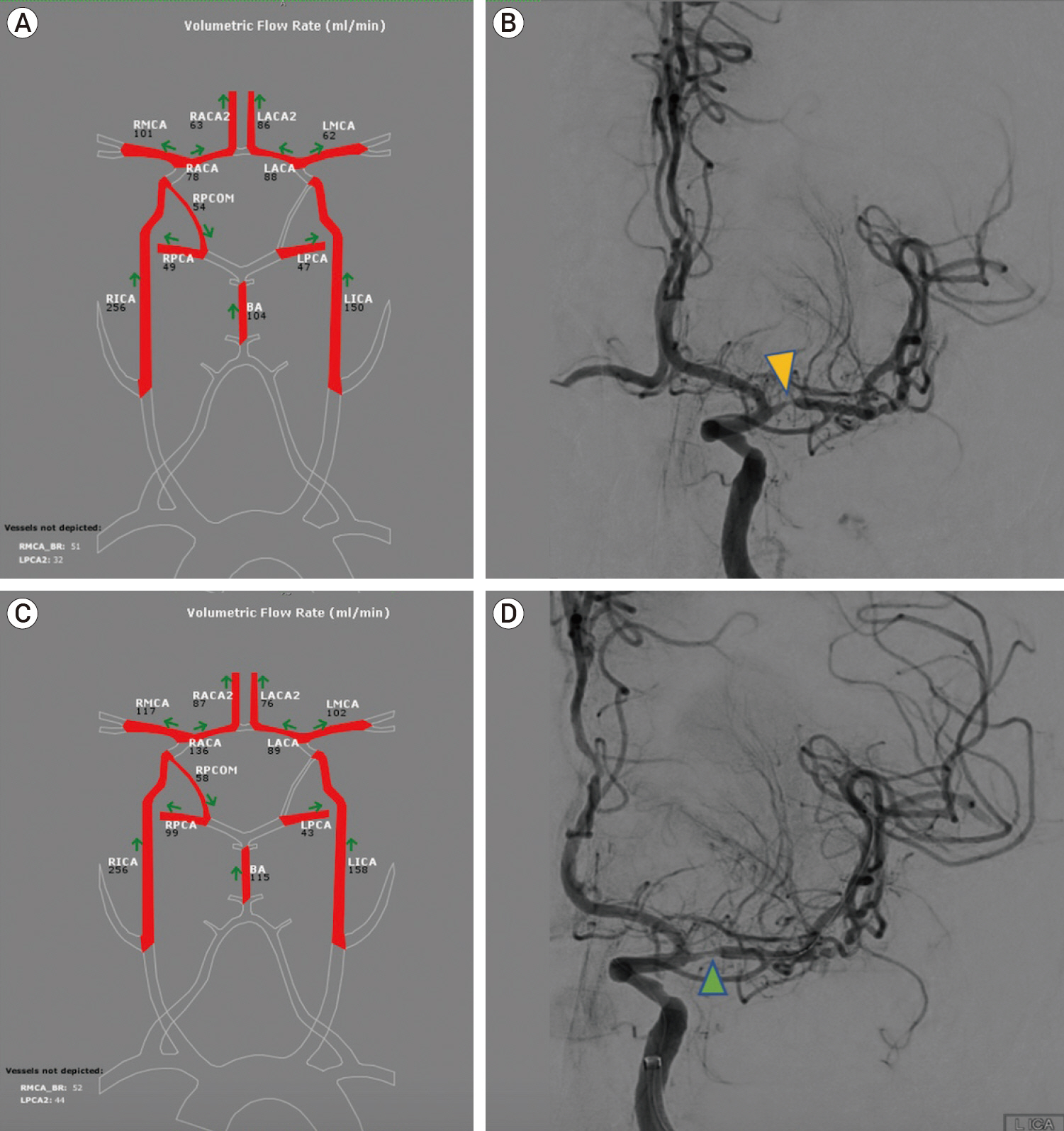
Use of quantitative magnetic resonance angiography in patients with symptomatic intracranial arterial stenosis who undergo stenting: Presentation of three cases
- Affiliations
-
- 1Department of Neurosurgery, Lenox Hill Hospital, New York, NY, USA
- KMID: 2517027
- DOI: http://doi.org/10.7461/jcen.2021.E2020.10.005
Abstract
- Intracranial atherosclerotic disease (ICAD) is an important cause of ischemic stroke. The etiology of stroke in patients with ICAD could be due to several mechanisms including hypoperfusion, artery-to-artery embolism, and plaque extension over small penetrating artery ostia. Management of symptomatic ICAD includes medical and endovascular management. Quantitative magnetic resonance angiography (MRA) is a technique that allows for non-invasive measurement of large vessel blood flow in the head and neck. Here, we describe procedural and clinical outcomes on three patients who presented with symptomatic ICAD and were treated with angioplasty and stenting. Quantitative MRA was used pre- and post- procedurally to assess the effects of stenting on the intracranial blood flow. Quantitative measures of intracranial blood flow may serve as an additional triage tool in the evaluation of patients with symptomatic ICAD.
Figure
Reference
-
1. Amin-Hanjani S, Du X, Pandey DK, Thulborn KR, Charbel FT. Effect of age and vascular anatomy on blood flow in major cerebral vessels. J Cereb Blood Flow Metab. 2015; Feb. 35(2):312–8.
Article2. Amin-Hanjani S, Du X, Zhao M, Walsh K, Malisch TW, Charbel FT. Use of quantitative magnetic resonance angiography to stratify stroke risk in symptomatic vertebrobasilar disease. Stroke. 2005; Jun. 36(6):1140–5.
Article3. Amin-Hanjani S, Pandey DK, Rose-Finnell L, Du X, Richardson D, Thulborn KR, et al. Effect of hemodynamics on stroke risk in symptomatic atherosclerotic vertebrobasilar occlusive disease. JAMA Neurol. 2016; Feb. 73(2):178–85.
Article4. Amin-Hanjani S, Shin JH, Zhao M, Du X, Charbel FT. Evaluation of extracranial-intracranial bypass using quantitative magnetic resonance angiography. J Neurosurg. 2007; Feb. 106(2):291–8.
Article5. Bae YJ, Jung C, Kim JH, Choi BS, Kim E. Quantitative magnetic resonance angiography in internal carotid artery occlusion with primary collateral pathway. J Stroke. 2015; Sep. 17(3):320–6.
Article6. Calderon-Arnulphi M, Amin-Hanjani S, Alaraj A, Zhao M, Du X, Ruland S, et al. In vivo evaluation of quantitative MR angiography in a canine carotid artery stenosis model. AJNR Am J Neuroradiol. 2011; Sep. 32(8):1552–9.
Article7. Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005; Mar. 352(13):1305–16.
Article8. Derdeyn CP, Chimowitz MI, Lynn MJ, Fiorella D, Turan TN, Janis LS, et al. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet. 2014; Jan. 383(9914):333–41.9. Derdeyn CP, Fiorella D, Lynn MJ, Turan TN, Lane BF, Janis LS, et al. Intracranial stenting: SAMMPRIS. Stroke. 2013; Jun. 44(6 Suppl 1):S41–4.10. Durukan A, Tatlisumak T. Acute ischemic stroke: overview of major experimental rodent models, pathophysiology, and therapy of focal cerebral ischemia. Pharmacol Biochem Behav. 2007; May. 87(1):179–97.
Article11. Flusty B, de Havenon A, Prabhakaran S, Liebeskind DS, Yaghi S. Intracranial atherosclerosis treatment: Past, present, and future. Stroke. 2020; Mar. 51(3):e49–53.12. Holmstedt CA, Turan TN, Chimowitz MI. Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment. Lancet Neurol. 2013; Nov. 12(11):1106–14.
Article13. Kasner SE, Lynn MJ, Chimowitz MI, Frankel MR, Howlett-Smith H, Hertzberg VS, et al. Warfarin vs aspirin for symptomatic intracranial stenosis: subgroup analyses from WASID. Neurology. 2006; Oct. 67(7):1275–8.
Article14. Kole M, Amin B, Marin H, Russman A, Sanders W. Intracranial angioplasty and stent placement for direct cerebral revascularization of nonacute intracranial occlusions and near occlusions. Neurosurg Focus. 2009; 26(3):E3.
Article15. Liebeskind DS, Cotsonis GA, Saver JL, Lynn MJ, Turan TN, Cloft HJ, et al. Collaterals dramatically alter stroke risk in intracranial atherosclerosis. Ann Neurol. 2011; Jun. 69(6):963–74.
Article16. Liebeskind DS. Collateral circulation. Stroke. 2003; Sep. 34(9):2279–84.
Article17. Naghavi M; Global Burden of Disease Self-Harm Collaborators. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 2019; Feb. 364:I94.
Article18. Reith W, Berkefeld J, Dietrich P, Fiehler J, Jansen O. Diagnosis and treatment of intracranial stenoses. Clin Neuroradiol. 2015; Oct. 25 Suppl 2:307–16.
Article19. Spilt A, Box FM, van der Geest RJ, Reiber JH, Kunz P, Kamper AM, et al. Reproducibility of total cerebral blood flow measurements using phase contrast magnetic resonance imaging. J Magn Reson Imaging. 2002; Jul. 16(1):1–5.
Article20. Wong KS, Huang YN, Gao S, Lam WW, Chan YL, Kay R. Intracranial stenosis in Chinese patients with acute stroke. Neurology. 1998; Mar. 50(3):812–3.
Article21. Yu W, Jiang WJ. Stenting for intracranial stenosis: potential future for the prevention of disabling or fatal stroke. Stroke Vasc Neurol. 2018; Jun. 3(3):140–6.
Article22. Zhao M, Amin-Hanjani S, Ruland S, Curcio AP, Ostergren L, Charbel FT. Regional cerebral blood flow using quantitative MR angiography. AJNR Am J Neuroradiol. 2007; Sep. 28(8):1470–3.
Article23. Zhao M, Charbel FT, Alperin N, Loth F, Clark ME. Improved phase-contrast flow quantification by three-dimensional vessel localization. Magn Reson Imaging. 2000; Jul. 18(6):697–706.
Article24. Zhao T, Zhu WY, Xiong XY, Li J, Wang L, Ding HY, et al. Safety and efficacy of wingspan stenting for severe symptomatic atherosclerotic stenosis of the middle cerebral artery: Analysis of 278 continuous cases. J Stroke Cerebrovasc Dis. 2016; Oct. 25(10):2368–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wingspan Stenting for Symptomatic Severe In-Stent Stenosis of a Closed-Cell Stent after Stent-Assisted Coiling of a Ruptured Intracranial Aneurysm
- Stenting of Symptomatic Middle Cerebral Artery Stenosis: Case Report
- MR Angiographic Findings in Ischemic Stroke Patients with Extracranial Carotid Artery Stenosis
- Angioplasty, Stenting and Other Potential Treatments of Atherosclerotic Stenosis of the Intracranial Arteries: Past, Present and Future
- Comparison of MR Angiography with Conventional Angiography in Cervical and Intracranial Vascular Diseases