Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):242-250. 10.14701/ahbps.2021.25.2.242.
Lymphopenia following pancreaticoduodenectomy is associated with pancreatic fistula formation
- Affiliations
-
- 1Department of Surgery, Rhode Island Hospital, Warren Alpert Medical School of Brown University, Providence, RI, USA
- KMID: 2516245
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.242
Abstract
- Backgrounds/Aims
Post-operative pancreatic fistulas (POPF) are a major source of morbidity following pancreaticoduodenectomy (PD). This study aims to investigate if persistent lymphopenia, a known marker of sepsis, can act as an additional marker of POPF with clinical implications that could help direct drain management.
Methods
A retrospective chart review of all patients who underwent PD in a single hospital network from 2008 to 2018. Persistent lymphopenia was defined as lymphopenia beyond post-operative day #3.
Results
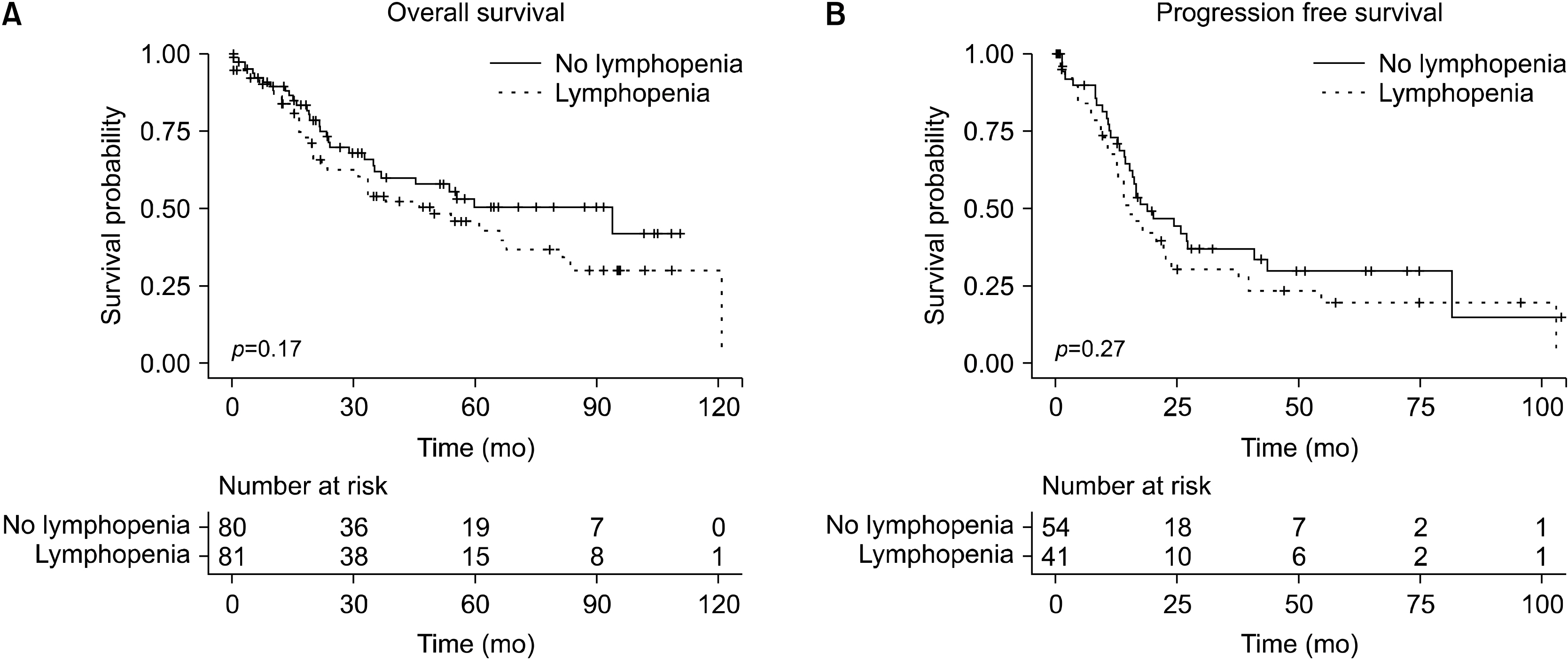
Of the 201 patients who underwent PD during the study period 161 patients had relevant laboratory data, 81 of whom had persistent lymphopenia. 17 patients with persistent lymphopenia went on to develop a POPF, compared to 7 patients without. Persistent lymphopenia had a negative predictive value of 91.3%. Multivariate analysis revealed only persistent lymphopenia as being independently associated with POPF (HR 2.57, 95% CI 1.07-6.643, p=0.039). Patients with persistent lymphopenia were more likely to have a complication requiring intervention (56.8% vs 35.0%, p<0.001).
Conclusions
Persistent lymphopenia is a readily available early marker of POPF that holds the potential to identify clinically relevant POPF in patients where no surgical drain is present, and to act as an adjunct of drain amylase helping to guide drain management.
Figure
Reference
-
1. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.2. Serene TEL, G SV, Padmakumar JS, Terence HCW, Keem LJ, Bei W, et al. 2018; Predictive value of post-operative drain amylase levels for post-operative pancreatic fistula. Ann Hepatobiliary Pancreat Surg. 22:397–404. DOI: 10.14701/ahbps.2018.22.4.397. PMID: 30588532. PMCID: PMC6295369.
Article3. Pedrazzoli S. 2017; Pancreatoduodenectomy (PD) and postoperative pancreatic fistula (POPF): a systematic review and analysis of the POPF-related mortality rate in 60,739 patients retrieved from the English literature published between 1990 and 2015. Medicine (Baltimore). 96:e6858. DOI: 10.1097/MD.0000000000006858. PMID: 28489778. PMCID: PMC5428612.4. Schäfer M, Müllhaupt B, Clavien PA. 2002; Evidence-based pancreatic head resection for pancreatic cancer and chronic pancreatitis. Ann Surg. 236:137–148. DOI: 10.1097/00000658-200208000-00001. PMID: 12170018. PMCID: PMC1422559.
Article5. Van Buren G 2nd, Bloomston M, Hughes SJ, Winter J, Behrman SW, Zyromski NJ, et al. 2014; A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Ann Surg. 259:605–612. DOI: 10.1097/SLA.0000000000000460. PMID: 24374513.
Article6. Witzigmann H, Diener MK, Kienkötter S, Rossion I, Bruckner T, Werner B, et al. 2016; No need for routine drainage after pancreatic head resection: the dual-center, randomized, controlled PANDRA trial (ISRCTN04937707). Ann Surg. 264:528–537. DOI: 10.1097/SLA.0000000000001859. PMID: 27513157.7. McMillan MT, Malleo G, Bassi C, Butturini G, Salvia R, Roses RE, et al. 2015; Drain management after pancreatoduodenectomy: reappraisal of a prospective randomized trial using risk stratification. J Am Coll Surg. 221:798–809. DOI: 10.1016/j.jamcollsurg.2015.07.005. PMID: 26278037.
Article8. Lee SR, Kim HO, Shin JH. 2019; Significance of drain fluid amylase check on day 3 after pancreatectomy. ANZ J Surg. 89:497–502. DOI: 10.1111/ans.15025. PMID: 30706662.
Article9. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. 2013; A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 216:1–14. DOI: 10.1016/j.jamcollsurg.2012.09.002. PMID: 23122535.
Article10. Miller BC, Christein JD, Behrman SW, Drebin JA, Pratt WB, Callery MP, et al. 2014; A multi-institutional external validation of the fistula risk score for pancreatoduodenectomy. J Gastrointest Surg. 18:172–179. discussion 179–180. DOI: 10.1007/s11605-013-2337-8. PMID: 24002771.
Article11. Seykora TF, Maggino L, Malleo G, Lee MK 4th, Roses R, Salvia R, et al. 2019; Evolving the paradigm of early drain removal following pancreatoduodenectomy. J Gastrointest Surg. 23:135–144. DOI: 10.1007/s11605-018-3959-7. PMID: 30406578.
Article12. Wang Q, Jiang YJ, Li J, Yang F, Di Y, Yao L, et al. 2014; Is routine drainage necessary after pancreaticoduodenectomy? World J Gastroenterol. 20:8110–8118. DOI: 10.3748/wjg.v20.i25.8110. PMID: 25009383. PMCID: PMC4081682.
Article13. Kawai M, Tani M, Terasawa H, Ina S, Hirono S, Nishioka R, et al. 2006; Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection: prospective study for 104 consecutive patients. Ann Surg. 244:1–7. DOI: 10.1097/01.sla.0000218077.14035.a6. PMID: 16794381. PMCID: PMC1570595.14. Venet F, Davin F, Guignant C, Larue A, Cazalis MA, Darbon R, et al. 2010; Early assessment of leukocyte alterations at diagnosis of septic shock. Shock. 34:358–363. DOI: 10.1097/SHK.0b013e3181dc0977. PMID: 20220566.
Article15. Munford RS, Pugin J. 2001; Normal responses to injury prevent systemic inflammation and can be immunosuppressive. Am J Respir Crit Care Med. 163:316–321. DOI: 10.1164/ajrccm.163.2.2007102. PMID: 11179099.
Article16. Heffernan DS, Monaghan SF, Thakkar RK, Machan JT, Cioffi WG, Ayala A. 2012; Failure to normalize lymphopenia following trauma is associated with increased mortality, independent of the leukocytosis pattern. Crit Care. 16:R12. DOI: 10.1186/cc11157. PMID: 22264310. PMCID: PMC3396248.
Article17. Drewry AM, Samra N, Skrupky LP, Fuller BM, Compton SM, Hotchkiss RS. 2014; Persistent lymphopenia after diagnosis of sepsis predicts mortality. Shock. 42:383–391. DOI: 10.1097/SHK.0000000000000234. PMID: 25051284. PMCID: PMC4362626.
Article18. Hotchkiss RS, Tinsley KW, Swanson PE, Schmieg RE Jr, Hui JJ, Chang KC, et al. 2001; Sepsis-induced apoptosis causes progressive profound depletion of B and CD4+ T lymphocytes in humans. J Immunol. 166:6952–6963. DOI: 10.4049/jimmunol.166.11.6952. PMID: 11359857.19. Le Tulzo Y, Pangault C, Gacouin A, Guilloux V, Tribut O, Amiot L, et al. 2002; Early circulating lymphocyte apoptosis in human septic shock is associated with poor outcome. Shock. 18:487–494. DOI: 10.1097/00024382-200212000-00001. PMID: 12462554.
Article20. Girardot T, Rimmelé T, Venet F, Monneret G. 2017; Apoptosis-induced lymphopenia in sepsis and other severe injuries. Apoptosis. 22:295–305. DOI: 10.1007/s10495-016-1325-3. PMID: 27812767.
Article21. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.22. Venet F, Rimmelé T, Monneret G. 2018; Management of sepsis-induced immunosuppression. Crit Care Clin. 34:97–106. DOI: 10.1016/j.ccc.2017.08.007. PMID: 29149944.
Article23. Hotchkiss RS, Karl IE. 2003; The pathophysiology and treatment of sepsis. N Engl J Med. 348:138–150. DOI: 10.1056/NEJMra021333. PMID: 12519925.
Article24. Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. 2014; Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 106:dju124. DOI: 10.1093/jnci/dju124.
Article25. Park JE, Barbul A. 2004; Understanding the role of immune regulation in wound healing. Am J Surg. 187:11S–16S. DOI: 10.1016/S0002-9610(03)00296-4.
Article26. You Y, Han IW, Choi DW, Heo JS, Ryu Y, Park DJ, et al. 2019; Nomogram for predicting postoperative pancreatic fistula. HPB (Oxford). 21:1436–1445. DOI: 10.1016/j.hpb.2019.03.351. PMID: 30982739.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy of the Prophylactic Use of Octreotide after a Pancreaticoduodenectomy
- The impact of perioperative inotropes on the incidence of pancreatic leak following pancreaticoduodenectomy
- Factors Influencing the Pancreatic Leakage after Pancreaticoduodenectomy
- A Clinical Analysis on the Pancreaticoduodenectomy
- Pancreatic Pseudocyst-Portal Vein Fistula: Serial Imaging and Clinical Follow-up from Pseudocyst to Fistula