Int J Thyroidol.
2021 May;14(1):37-41. 10.11106/ijt.2021.14.1.37.
Branchial Cleft Cyst Mimicking Malignant Thyroid Neoplasm Concurrent with Medullary and Papillary Thyroid Carcinoma: a Case Report
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 2Department of Otorhinolaryngology–Head and Neck Surgery, Pusan National University Hospital, Busan, Korea
- 3Department of Pathology, Pusan National University Hospital, Busan, Korea
- KMID: 2516163
- DOI: http://doi.org/10.11106/ijt.2021.14.1.37
Abstract
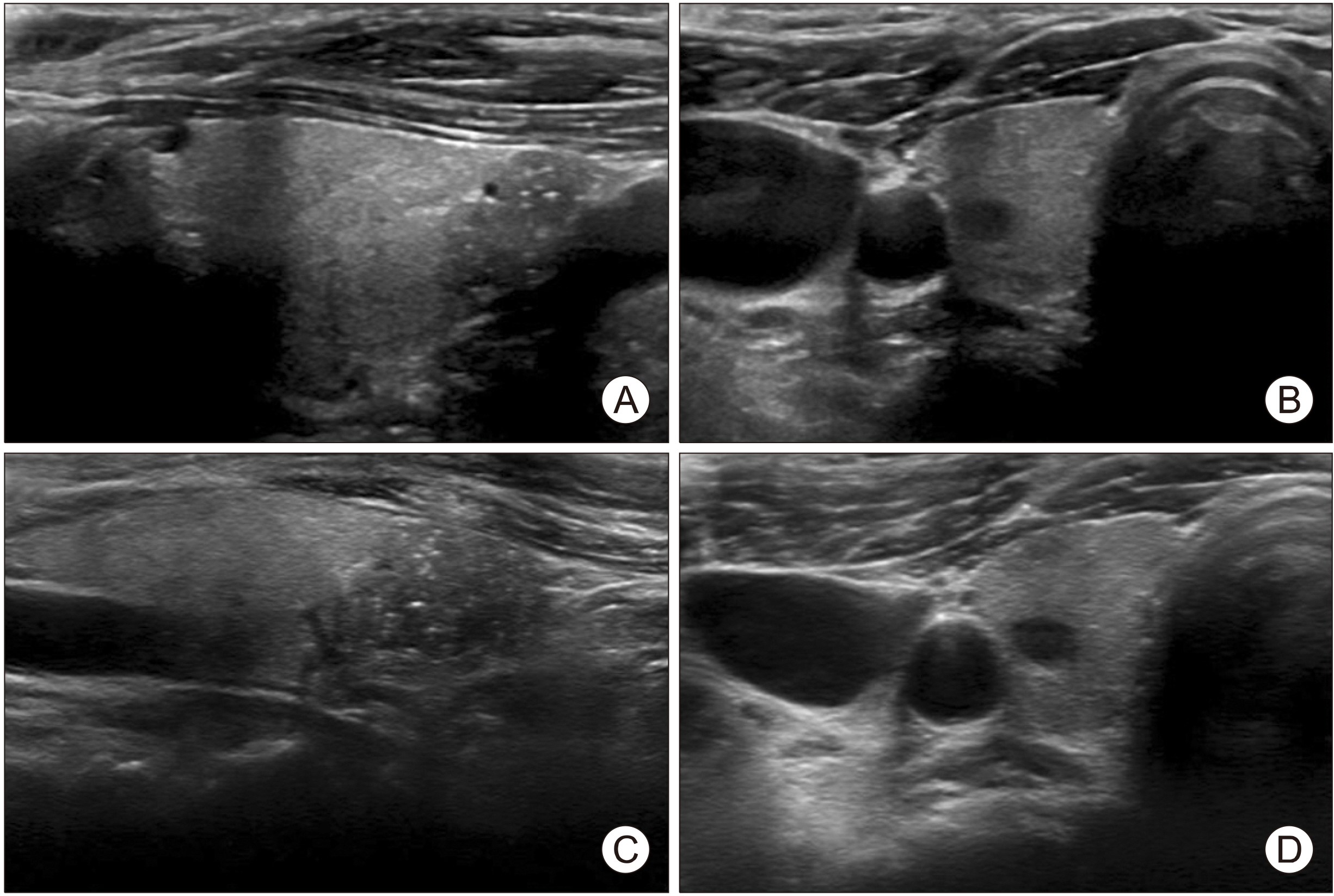
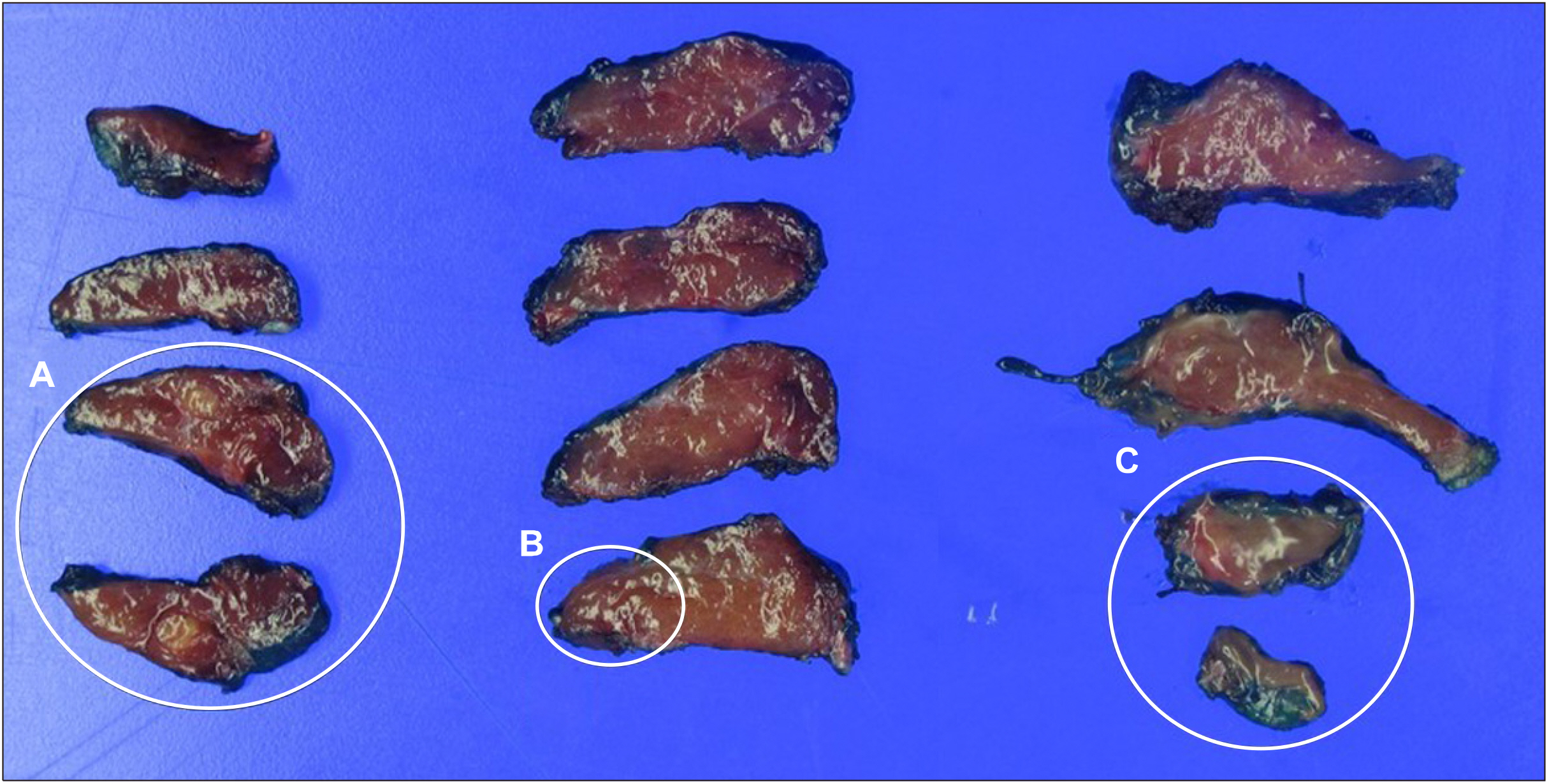
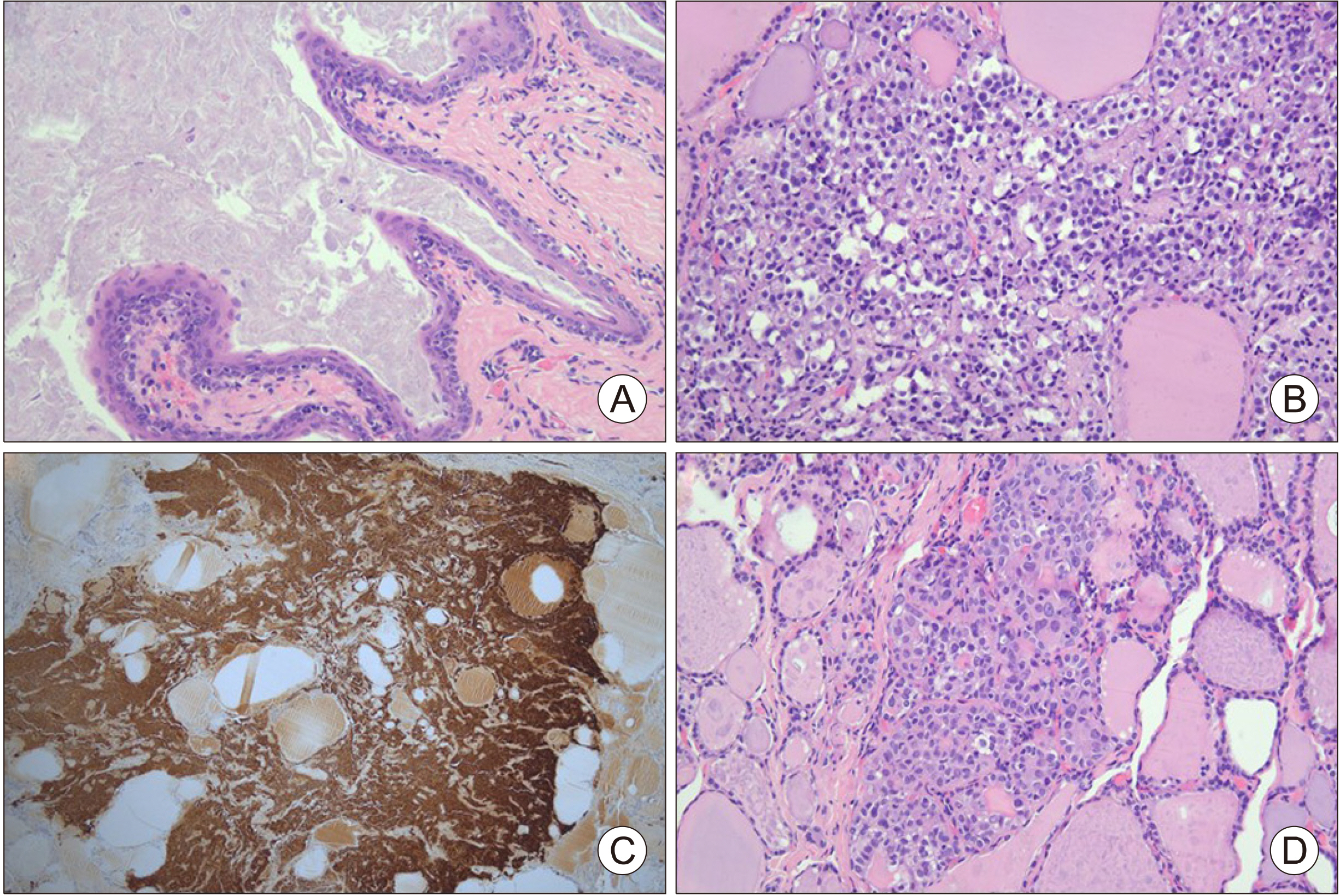
- Branchial cleft cysts are the most common lateral neck mass, and usually have well-delineated cystic structures under ultrasonography. Ultrasonography and fine needle aspiration cytology is very helpful during preoperative diagnosis. However, these cysts may occur in unusual locations and have a sonographic morphology similar to malignant thyroid neoplasm. A 61-year-old woman presented with thyroid nodules, and ultrasonography revealed a 0.8-cm, hypoechoic, solid nodule with microcalcifications in the right lobe of thyroid in the lower portion. Postoperative histopathological examination revealed the 0.8-cm hypoechoic nodule to be a branchial cleft cyst. In addition, concurrent medullary thyroid carcinoma (MTC) and papillary thyroid carcinoma (PTC) were found. Herein, we present a rare case of branchial cleft cyst mimicking malignant thyroid neoplasm concurrent with medullary and PTC.
Keyword
Figure
Reference
-
References
1. Maran AG, Buchanan DR. 1978; Branchial cysts, sinuses and fistulae. Clin Otolaryngol Allied Sci. 3(1):77–92. DOI: 10.1111/j.1365-2273.1978.tb00670.x. PMID: 348350.
Article2. Giunta J, Cataldo E. 1973; Lymphoepithelial cysts of the oral mucosa. Oral Surg Oral Med Oral Pathol. 35(1):77–84. DOI: 10.1016/0030-4220(73)90096-0. PMID: 4508843.
Article3. Weidner N, Geisinger KR, Sterling RT, Miller TR, Yen TS. 1986; Benign lymphoepithelial cysts of the parotid gland. A histologic, cytologic, and ultrastructural study. Am J Clin Pathol. 85(4):395–401. DOI: 10.1093/ajcp/85.4.395. PMID: 3953495.
Article4. Miyazaki M, Kiuchi S, Fujioka Y. 2016; Branchial cleft-like cysts in Hashimoto's thyroiditis: a case report and literature review. Pathol Int. 66(5):297–301. DOI: 10.1111/pin.12411. PMID: 27112136.
Article5. Thomas B, Shroff M, Forte V, Blaser S, James A. 2010; Revisiting imaging features and the embryologic basis of third and fourth branchial anomalies. AJNR Am J Neuroradiol. 31(4):755–60. DOI: 10.3174/ajnr.A1902. PMID: 20007720. PMCID: PMC7964224.
Article6. Bagchi A, Hira P, Mittal K, Priyamvara A, Dey AK. 2018; Branchial cleft cysts: a pictorial review. Pol J Radiol. 83:e204–e9. DOI: 10.5114/pjr.2018.76278. PMID: 30627236. PMCID: PMC6323601.7. Gritzmann N, Hollerweger A, Macheiner P, Rettenbacher T. 2002; Sonography of soft tissue masses of the neck. J Clin Ultrasound. 30(6):356–73. DOI: 10.1002/jcu.10073. PMID: 12116098.
Article8. Brown RE, Harave S. 2016; Diagnostic imaging of benign and malignant neck masses in children-a pictorial review. Quant Imaging Med Surg. 6(5):591–604. DOI: 10.21037/qims.2016.10.10. PMID: 27942480. PMCID: PMC5130564.
Article9. Sizemore GW. 1987; Medullary carcinoma of the thyroid gland. Semin Oncol. 14(3):306–14. PMID: 2888195.10. Liberman M, Kay S, Emil S, Flageole H, Nguyen LT, Tewfik TL, et al. 2002; Ten years of experience with third and fourth branchial remnants. J Pediatr Surg. 37(5):685–90. DOI: 10.1053/jpsu.2002.32253. PMID: 11987078.
Article11. Gage H, Hubbard E, Nodit L. 2016; Multiple squamous cells in thyroid fine needle aspiration: friends or foes? Diagn Cytopathol. 44(8):676–81. DOI: 10.1002/dc.23512. PMID: 27265307.
Article12. Lamberg BA, Reissel P, Stenman S, Koivuniemi A, Ekbolm M, Makinen J, et al. 1981; Concurrent medullary and papillary thyroid carcinoma in the same thyroid lobe and in siblings. Acta Med Scand. 209(5):421–4. DOI: 10.1111/j.0954-6820.1981.tb11620.x. PMID: 7246276.
Article13. Hedinger C, Williams ED, Sobin LH. 1989; The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 63(5):908–11. DOI: 10.1002/1097-0142(19890301)63:5<908::AID-CNCR2820630520>3.0.CO;2-I. PMID: 2914297.
Article14. Dikbas O, Duman AA, Guvendi GF. 2019; Medullary thyroid carcinoma and papillary thyroid carcinoma in the same patient as a collision tumour. Case Rep Endocrinol. 2019:4038628. DOI: 10.1155/2019/4038628. PMID: 30993022. PMCID: PMC6434312.
Article15. Kim WG, Gong G, Kim EY, Kim TY, Hong SJ, Kim WB, et al. 2010; Concurrent occurrence of medullary thyroid carcinoma and papillary thyroid carcinoma in the same thyroid should be considered as coincidental. Clin Endocrinol (Oxf). 72(2):256–63. DOI: 10.1111/j.1365-2265.2009.03622.x. PMID: 20447064.
Article16. Adnan Z, Arad E, Dana J, Shendler Y, Baron E. 2013; Simultaneous occurrence of medullary and papillary thyroid microcarcinomas: a case series and review of the literature. J Med Case Rep. 7:26. DOI: 10.1186/1752-1947-7-26. PMID: 23336429. PMCID: PMC3552861.
Article17. Appetecchia M, Lauretta R, Barnabei A, Pieruzzi L, Terrenato I, Cavedon E, et al. 2019; Epidemiology of simultaneous medullary and papillary thyroid carcinomas (MTC/PTC): an Italian multicenter study. Cancers (Basel). 11(10):1516. DOI: 10.3390/cancers11101516. PMID: 31600997. PMCID: PMC6826384.
Article18. Wells SA Jr, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, et al. 2015; Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 25(6):567–610. DOI: 10.1089/thy.2014.0335. PMID: 25810047. PMCID: PMC4490627.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- A Case of a Metastatic Papillary Thyroid Carcinoma Presenting as a Lateral Neck Cyst
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- Primary papillary carcinoma originated from a branchial cleft cyst
- A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma