Cancer Res Treat.
2021 Apr;53(2):584-592. 10.4143/crt.2020.735.
Difficulties Doctors Experience during Life-Sustaining Treatment Discussion after Enactment of the Life-Sustaining Treatment Decisions Act: A Cross-Sectional Study
- Affiliations
-
- 1Center for Palliative Care and Clinical Ethics, Seoul National University Hospital, Seoul, Korea
- 2Department of Pediatrics, Seoul National University Hospital, Seoul, Korea
- 3Department of Psychiatry, Seoul National University Hospital, Seoul, Korea
- 4Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2514939
- DOI: http://doi.org/10.4143/crt.2020.735
Abstract
- Purpose
This study aimed to investigate difficulties doctors experience during life-sustaining treatment (LST) discussion with seriously ill patients and their families after enactment of the LST Decisions Act in February 2018.
Materials and Methods
A cross-sectional survey was conducted in a tertiary hospital in the Republic of Korea in August 2019. Six hundred eighty-six doctors who care for seriously ill patients were given a structured questionnaire, and difficulties during the discussion were examined.
Results
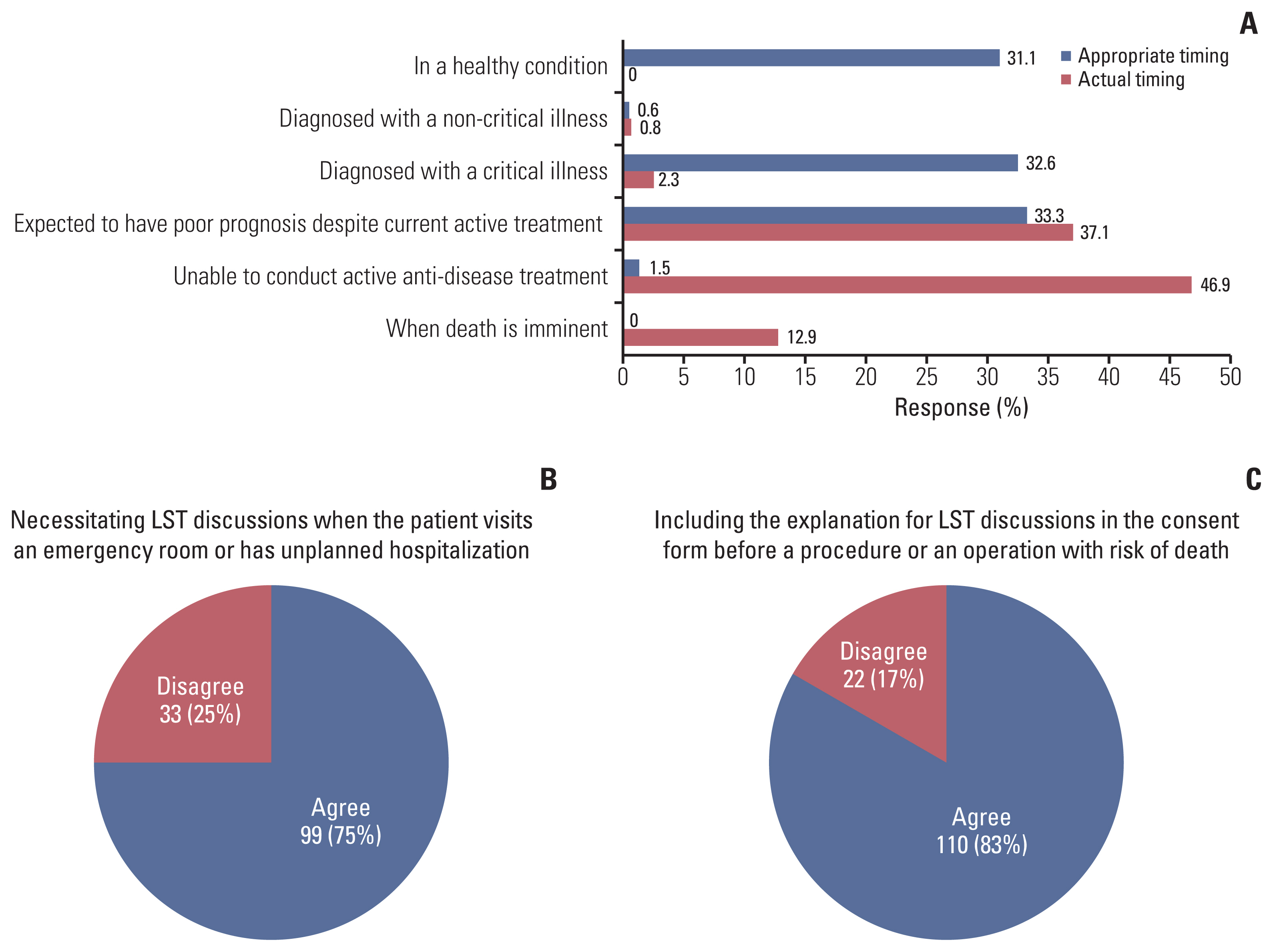
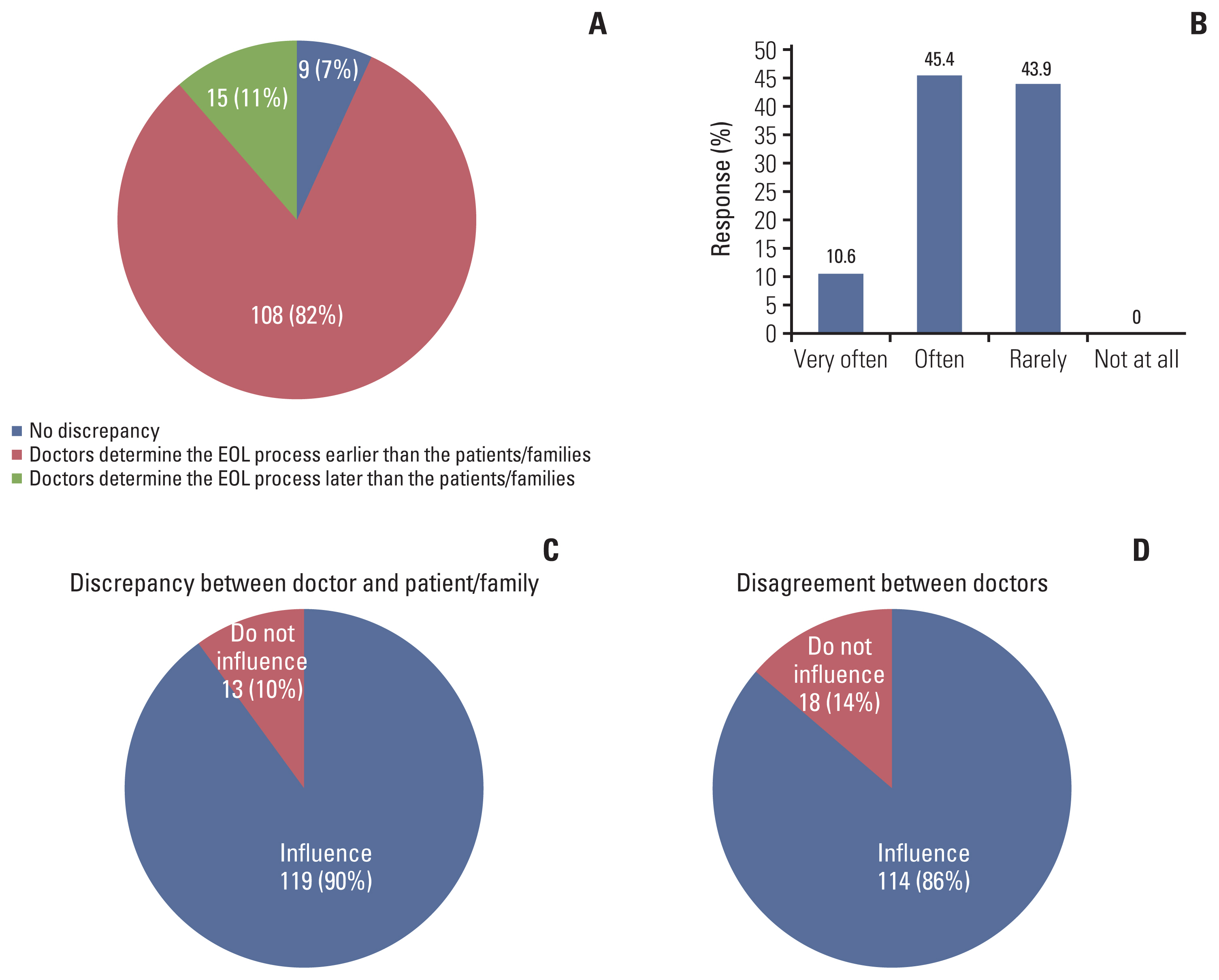
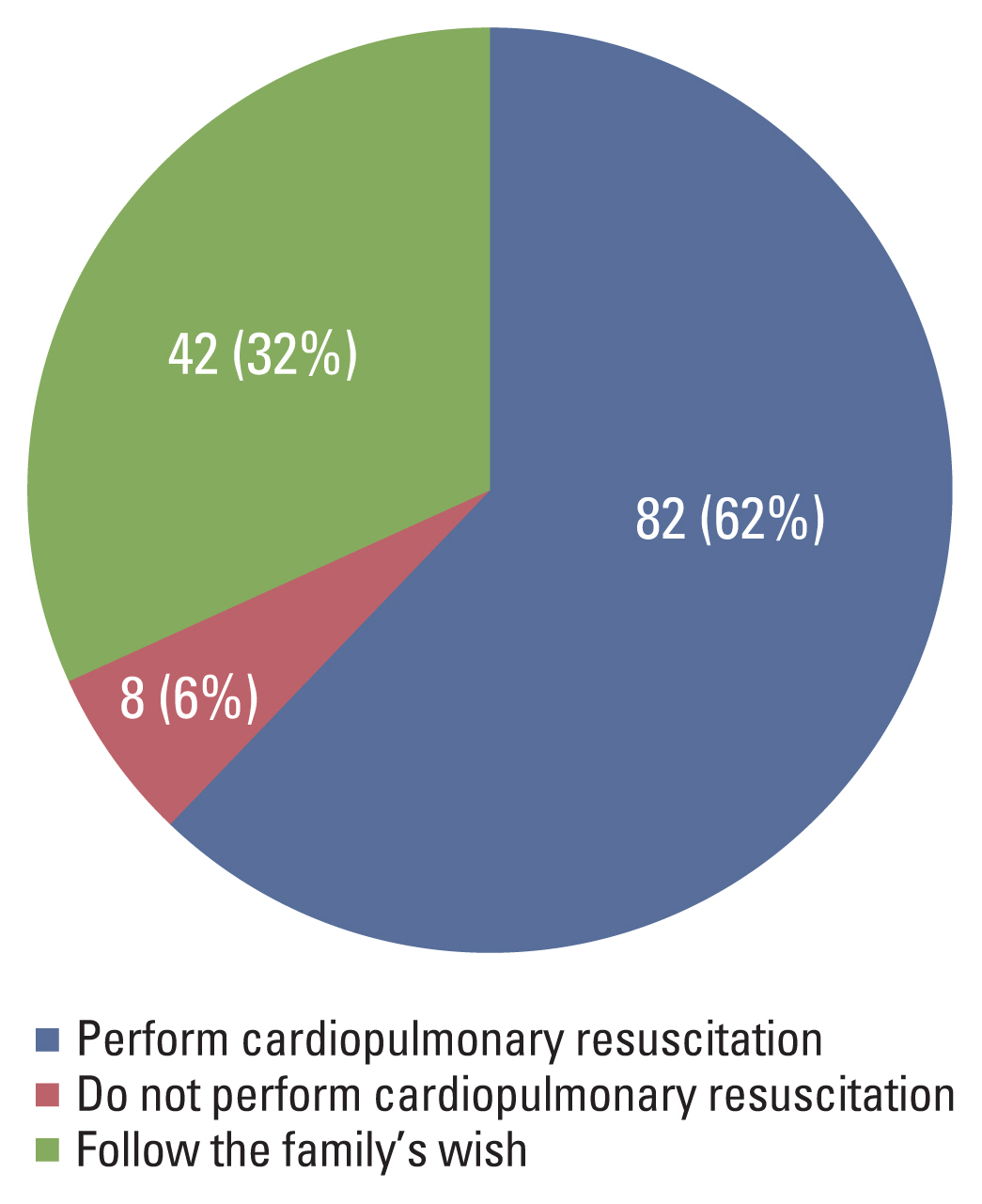
One hundred thirty-two doctors completed the questionnaire. Eighty-five percent answered they treat cancer patients. Most (86.4%) experienced considerable difficulties during LST discussions (mean score, 7.4±1.6/10). The two most common difficulties were communication with patients and family and determining when to discuss LST. Two-thirds of doctors found direct discussions with the patient difficult and said they would initiate LST discussions only with family. LST discussions were actually initiated later than considered appropriate. When medically assessing whether the patient is imminently dying, 56% of doctors experienced disagreements with other doctors, which could affect their decisions.
Conclusion
This study found that most doctors experienced serious difficulties regarding communication with patients and family and medical assessment of dying process during LST discussions. To alleviate these difficulties, further institutional support is needed to improve the LST discussion between doctors, patients, and family.
Figure
Cited by 1 articles
-
Analysis of Cancer Patient Decision-Making and Health Service Utilization after Enforcement of the Life-Sustaining Treatment Decision-Making Act in Korea
Dalyong Kim, Shin Hye Yoo, Seyoung Seo, Hyun Jung Lee, Min Sun Kim, Sung Joon Shin, Chi-Yeon Lim, Do Yeun Kim, Dae Seog Heo, Chae-Man Lim
Cancer Res Treat. 2022;54(1):20-29. doi: 10.4143/crt.2021.131.
Reference
-
References
1. Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients’ perspectives. JAMA. 1999; 281:163–8.2. Matsuyama R, Reddy S, Smith TJ. Why do patients choose chemotherapy near the end of life? A review of the perspective of those facing death from cancer. J Clin Oncol. 2006; 24:3490–6.
Article3. Jho HJ, Nam EJ, Shin IW, Kim SY. Changes of end of life practices for cancer patients and their association with hospice palliative care referral over 2009–2014: a single institution study. Cancer Res Treat. 2020; 52:419–25.
Article4. Kim DY, Lee KE, Nam EM, Lee HR, Lee KW, Kim JH, et al. Do-not-resuscitate orders for terminal patients with cancer in teaching hospitals of Korea. J Palliat Med. 2007; 10:1153–8.
Article5. Oh DY, Kim JH, Kim DW, Im SA, Kim TY, Heo DS, et al. CPR or DNR? End-of-life decision in Korean cancer patients: a single center’s experience. Support Care Cancer. 2006; 14:103–8.
Article6. Baek SK, Chang HJ, Byun JM, Han JJ, Heo DS. The association between end-of-life care and the time interval between provision of a do-not-resuscitate consent and death in cancer patients in Korea. Cancer Res Treat. 2017; 49:502–8.
Article7. Choi Y, Keam B, Kim TM, Lee SH, Kim DW, Heo DS. Cancer treatment near the end-of-life becomes more aggressive: changes in trend during 10 years at a single institute. Cancer Res Treat. 2015; 47:555–63.
Article8. Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008; 26:3860–6.
Article9. National Law Information Center. Act on decisions on lifesustaining treatment for patients in hospice and palliative care or at the end of life. Act No. 14013 (August 4, 2017).10. Lee SY, Seo HJ, Kim S, Eo JS, Oh SC. Prognostic significance of interim 18F-fluorodeoxyglucose positron emission tomography-computed tomography volumetric parameters in metastatic or recurrent gastric cancer. Asia Pac J Clin Oncol. 2018; 14:e302–9.
Article11. Koh SJ, Kim S, Kim J. Communication for end-of-life care planning among Korean patients with terminal cancer: a context-oriented model. Palliat Support Care. 2016; 14:69–76.
Article12. Koh SJ, Kim S, Kim J, Keam B, Heo DS, Lee KH, et al. Experiences and opinions related to end-of-life discussion: from oncologists’ and resident physicians’ perspectives. Cancer Res Treat. 2018; 50:614–23.
Article13. Shin DW, Lee JE, Cho B, Yoo SH, Kim S, Yoo JH. End-of-life communication in Korean older adults: With focus on advance care planning and advance directives. Geriatr Gerontol Int. 2016; 16:407–15.
Article14. Lee J, Kim J, Kim TS, Kim C. Communication about death and confidence levels concerning death-related issues among Koreans. Korean J Fam Pract. 2019; 9:303–10.
Article15. Kim JS, Yoo SH, Choi W, Kim Y, Hong J, Kim MS, et al. Implication of the life-sustaining treatment decisions act on end-of-life care for Korean terminal patients. Cancer Res Treat. 2020; 52:917–24.
Article16. Balaban RB. A physician’s guide to talking about end-of-life care. J Gen Intern Med. 2000; 15:195–200.
Article17. Kim SH. Preferences for autonomy in end-of-life decision making in modern Korean society. Nurs Ethics. 2015; 22:228–36.
Article18. Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017; 35:96–112.
Article19. Park IK, Jun HJ, Park SJ, Lim GJ, Cho SJ, Song A, et al. Differences in end-of-life care decision making between patients with and without cancer. Am J Hosp Palliat Care. 2015; 32:797–801.
Article20. Lee JE, Goo A, Shin DW, Yoo JH. Korean Geriatrics Society End-of-Life Research Group. Korean medical professionals’ attitudes and experiences on advance care planning for noncancerous disease. Ann Geriatr Med Res. 2019; 23:63–70.
Article21. An HJ, Jeon HJ, Chun SH, Jung HA, Ahn HK, Lee KH, et al. Feasibility study of physician orders for life-sustaining treatment for patients with terminal cancer. Cancer Res Treat. 2019; 51:1632–8.
Article22. Surbone A. Truth telling to the patient. JAMA. 1992; 268:1661–2.
Article23. Smith TJ, Swisher K. Telling the truth about terminal cancer. JAMA. 1998; 279:1746–8.
Article24. Sulmasy DP, Snyder L. Substituted interests and best judgments: an integrated model of surrogate decision making. JAMA. 2010; 304:1946–7.25. Yamamoto S, Arao H, Masutani E, Aoki M, Kishino M, Morita T, et al. Decision making regarding the place of end-of-life cancer care: the burden on bereaved families and related factors. J Pain Symptom Manage. 2017; 53:862–70.
Article26. Daugherty CK, Hlubocky FJ. What are terminally ill cancer patients told about their expected deaths? A study of cancer physicians’ self-reports of prognosis disclosure. J Clin Oncol. 2008; 26:5988–93.
Article27. Fallowfield L, Lipkin M, Hall A. Teaching senior oncologists communication skills: results from phase I of a comprehensive longitudinal program in the United Kingdom. J Clin Oncol. 1998; 16:1961–8.
Article28. Schroder C, Heyland D, Jiang X, Rocker G, Dodek P. Canadian Researchers at the End of Life Network. Educating medical residents in end-of-life care: insights from a multicenter survey. J Palliat Med. 2009; 12:459–70.
Article29. Billings ME, Curtis JR, Engelberg RA. Medicine residents’ self-perceived competence in end-of-life care. Acad Med. 2009; 84:1533–9.
Article30. Mack JW, Cronin A, Taback N, Huskamp HA, Keating NL, Malin JL, et al. End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med. 2012; 156:204–10.31. Honiden S, Possick J. Should physicians new to a case counsel patients and their families to change course at the end of life? AMA J Ethics. 2018; 20:E699–707.32. Vig EK, Sudore RL, Berg KM, Fromme EK, Arnold RM. Responding to surrogate requests that seem inconsistent with a patient’s living will. J Pain Symptom Manage. 2011; 42:777–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Well-Dying: Assisted Justice Act as a Dignified and Happy ‘Right to Self-Determination’
- Hemodialysis as a life-sustaining treatment at the end of life
- Trends in Nursing Research on Life-Sustaining Treatment in South Korea after the Enforcement of the Act on Decisions on Life-Sustaining Treatment
- The Characteristics of Patients in the Actively Dying Phase by Documenting the Implementation of Decisions on Life-sustaining Treatment
- The Problems and the Improvement Plan of the Hospice/Palliative Care and Dying Patient's Decisions on Life-Sustaining Treatment Act