Clin Endosc.
2021 Mar;54(2):211-221. 10.5946/ce.2020.068.
Prospective Comparison of the AIMS65 Score, Glasgow-Blatchford Score, and Rockall Score for Predicting Clinical Outcomes in Patients with Variceal and Nonvariceal Upper Gastrointestinal Bleeding
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Hatyai Hospital, Songkhla, Thailand
- 2Department of Internal Medicine, Hatyai Hospital, Songkhla, Thailand
- 3Siriraj Gastrointestinal Endoscopy Center, Division of Gastroenterology, Department of Internal Medicine, Siriraj Hospital, Faculty of Medicine, Mahidol University, Bangkok, Thailand
- KMID: 2514175
- DOI: http://doi.org/10.5946/ce.2020.068
Abstract
- Background/Aims
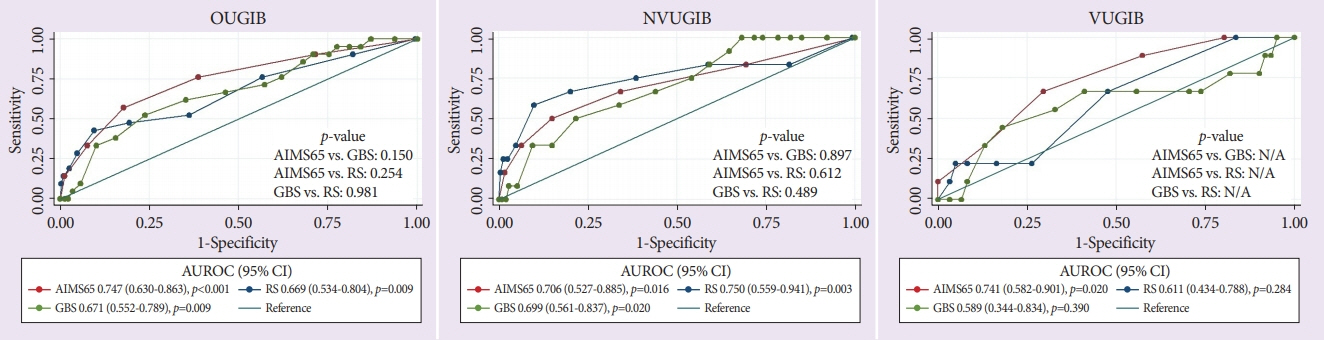
This study aimed to determine the performance of the AIMS65 score (AIMS65), Glasgow-Blatchford score (GBS), and Rockall score (RS) in predicting outcomes in patients with upper gastrointestinal bleeding (UGIB), and to compare the results between patients with nonvariceal UGIB (NVUGIB) and those with variceal UGIB (VUGIB).
Methods
We conducted a prospective observational study between March 2016 and December 2017. Receiver operating characteristic curve analysis was performed for all outcomes for comparison. The associations of all three scores with mortality were evaluated using multivariate logistic regression analysis.
Results
Of the total of 337 patients with UGIB, 267 patients (79.2%) had NVUGIB. AIMS65 was significantly associated (odds ratio [OR]=1.735; 95% confidence interval [CI]=1.148–2.620), RS was marginally associated (OR=1.225; 95% CI=0.973–1.543), but GBS was not associated (OR=1.017; 95% CI=0.890–1.163) with mortality risk in patients with UGIB. However, all three scores accurately predicted all other outcomes (all p<0.05) except rebleeding (p>0.05). Only AIMS65 precisely predicted mortality, the need for blood transfusion and the composite endpoint (all p<0.05) in patients with VUGIB.
Conclusions
AIMS65 is superior to GBS and RS in predicting mortality in patients with UGIB, and also precisely predicts the need for blood transfusion and the composite endpoint in patients with VUGIB. No scoring system could satisfactorily predict rebleeding in all patients with UGIB.
Keyword
Figure
Cited by 1 articles
-
The Value of Risk Scores to Predict Clinical Outcomes in Patients with Variceal and Non-Variceal Upper Gastrointestinal Bleeding
James Yun-wong Lau
Clin Endosc. 2021;54(2):145-146. doi: 10.5946/ce.2021.077.
Reference
-
1. Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010; 152:101–113.
Article2. Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012; 107:345–360. quiz 361.
Article3. Gralnek IM, Dumonceau JM, Kuipers EJ, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2015; 47:a1–a46.
Article4. Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996; 38:316–321.
Article5. Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000; 356:1318–1321.
Article6. Saltzman JR, Tabak YP, Hyett BH, Sun X, Travis AC, Johannes RS. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. Gastrointest Endosc. 2011; 74:1215–1224.
Article7. Robertson M, Majumdar A, Boyapati R, et al. Risk stratification in acute upper GI bleeding: comparison of the AIMS65 score with the Glasgow-Blatchford and Rockall scoring systems. Gastrointest Endosc. 2016; 83:1151–1160.
Article8. Stanley AJ, Laine L, Dalton HR, et al. Comparison of risk scoring systems for patients presenting with upper gastrointestinal bleeding: international multicentre prospective study. BMJ. 2017; 356:i6432.
Article9. Park SM, Yeum SC, Kim BW, et al. Comparison of AIMS65 score and other scoring systems for predicting clinical outcomes in Koreans with nonvariceal upper gastrointestinal bleeding. Gut Liver. 2016; 10:526–531.
Article10. Gu L, Xu F, Yuan J. Comparison of AIMS65, Glasgow-Blatchford and Rockall scoring approaches in predicting the risk of in-hospital death among emergency hospitalized patients with upper gastrointestinal bleeding: a retrospective observational study in Nanjing, China. BMC Gastroenterol. 2018; 18:98.
Article11. Martínez-Cara JG, Jiménez-Rosales R, Úbeda-Muñoz M, de Hierro ML, de Teresa J, Redondo-Cerezo E. Comparison of AIMS65, Glasgow-Blatchford score, and Rockall score in a European series of patients with upper gastrointestinal bleeding: performance when predicting in-hospital and delayed mortality. United European Gastroenterol J. 2016; 4:371–379.
Article12. Marmo R, Koch M, Cipolletta L, et al. Predicting mortality in non-variceal upper gastrointestinal bleeders: validation of the Italian PNED score and prospective comparison with the Rockall score. Am J Gastroenterol. 2010; 105:1284–1291.
Article13. Jung SH, Oh JH, Lee HY, et al. Is the AIMS65 score useful in predicting outcomes in peptic ulcer bleeding? World J Gastroenterol. 2014; 20:1846–1851.14. Romagnuolo J, Barkun AN, Enns R, Armstrong D, Gregor J. Simple clinical predictors may obviate urgent endoscopy in selected patients with nonvariceal upper gastrointestinal tract bleeding. Arch Intern Med. 2007; 167:265–270.
Article15. Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017; 65:310–335.
Article16. de Franchis R. Expanding consensus in portal hypertension: report of the Baveno VI consensus workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015; 63:743–752.17. Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013; 368:11–21.
Article18. Hyett BH, Abougergi MS, Charpentier JP, et al. The AIMS65 score compared with the Glasgow-Blatchford score in predicting outcomes in upper GI bleeding. Gastrointest Endosc. 2013; 77:551–557.
Article19. Bryant RV, Kuo P, Williamson K, et al. Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding. Gastrointest Endosc. 2013; 78:576–583.
Article20. Abougergi MS, Charpentier JP, Bethea E, et al. A prospective, multicenter study of the AIMS65 score compared with the Glasgow-Blatchford score in predicting upper gastrointestinal hemorrhage outcomes. J Clin Gastroenterol. 2016; 50:464–469.
Article21. Yaka E, Yılmaz S, Doğan N, Pekdemir M. Comparison of the Glasgow-Blatchford and AIMS65 scoring systems for risk stratification in upper gastrointestinal bleeding in the emergency department. Acad Emerg Med. 2015; 22:22–30.
Article22. Aquarius M, Smeets FG, Konijn HW, et al. Prospective multicenter validation of the Glasgow Blatchford bleeding score in the management of patients with upper gastrointestinal hemorrhage presenting at an emergency department. Eur J Gastroenterol Hepatol. 2015; 27:1011–1016.
Article23. Reed EA, Dalton H, Blatchford O, et al. Is the Glasgow Blatchford score useful in the risk assessment of patients presenting with variceal haemorrhage? Eur J Gastroenterol Hepatol. 2014; 26:432–437.
Article24. Choe JW, Kim SY, Hyun JJ, et al. Is the AIMS 65 score useful in prepdicting clinical outcomes in Korean patients with variceal and nonvariceal upper gastrointestinal bleeding? Gut Liver. 2017; 11:813–820.
Article25. Thanapirom K, Ridtitid W, Rerknimitr R, et al. Prospective comparison of three risk scoring systems in non-variceal and variceal upper gastrointestinal bleeding. J Gastroenterol Hepatol. 2016; 31:761–767.
Article26. Budimir I, Gradišer M, Nikolić M, et al. Glasgow Blatchford, pre-endoscopic Rockall and AIMS65 scores show no difference in predicting rebleeding rate and mortality in variceal bleeding. Scand J Gastroenterol. 2016; 51:1375–1379.
Article27. Alexandrino G, Carvalho R, Reis J. Comparison of the AIMS65 score with other risk stratification scores in upper variceal and nonvariceal gastrointestinal bleeding. Gut Liver. 2018; 12:111–113.
Article28. Robertson M, Ng J, Abu Shawish W, et al. Risk stratification in acute variceal bleeding: comparison of the AIMS65 score to established upper gastrointestinal bleeding and liver disease severity risk stratification scoring systems in predicting mortality and rebleeding. Dig Endosc. 2020; 32:761–768.
Article29. Kim BJ, Park MK, Kim SJ, et al. Comparison of scoring systems for the prediction of outcomes in patients with nonvariceal upper gastrointestinal bleeding: a prospective study. Dig Dis Sci. 2009; 54:2523–2529.
Article30. Yang HM, Jeon SW, Jung JT, et al. Comparison of scoring systems for nonvariceal upper gastrointestinal bleeding: a multicenter prospective cohort study. J Gastroenterol Hepatol. 2016; 31:119–125.
Article31. Nakamura S, Matsumoto T, Sugimori H, Esaki M, Kitazono T, Hashizume M. Emergency endoscopy for acute gastrointestinal bleeding: prognostic value of endoscopic hemostasis and the AIMS65 score in Japanese patients. Dig Endosc. 2014; 26:369–376.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of AIMS65 Score and Other Scoring Systems for Predicting Clinical Outcomes in Koreans with Nonvariceal Upper Gastrointestinal Bleeding
- Is the AIMS 65 Score Useful in Prepdicting Clinical Outcomes in Korean Patients with Variceal and Nonvariceal Upper Gastrointestinal Bleeding?
- Validation of the Glasgow-Blatchford score and the Pre-endoscopic Rockall Score for Predicting Active Gastrointestinal Bleeding in Emergency Department Patients with Suspected Upper Gastrointestinal Bleeding
- The AIMS65 Score Is a Useful Predictor of Mortality in Patients with Nonvariceal Upper Gastrointestinal Bleeding: Urgent Endoscopy in Patients with High AIMS65 Scores
- Risk Stratification in Cancer Patients with Acute Upper Gastrointestinal Bleeding: Comparison of Glasgow-Blatchford, Rockall and AIMS65, and Development of a New Scoring System