J Korean Med Sci.
2021 Mar;36(9):e68. 10.3346/jkms.2021.36.e68.
Epidemiological Study of Malignant Gliomas in Korea Using Nationwide Dataset from 2007 to 2017
- Affiliations
-
- 1Department of Neurosurgery, Myong Ji St. Mary's Hospital, Seoul, Korea
- 2Department of Neurosurgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Neurosurgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 5Department of Biostatistics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 6Department of Neurosurgery, Cell Death Disease Research Center, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2513588
- DOI: http://doi.org/10.3346/jkms.2021.36.e68
Abstract
- Background
The purpose of the study was to investigate the incidence, prevalence, and survival of malignant gliomas (MGs) using population-based Korean National Health Insurance Database (NHID) data.
Methods
Using the Korean NHID, we identified patients with MG as C71 codes in KCD 5–7 according to ICD-10 from January 1, 2007 to December 31, 2017. Epidemiological characteristics of MG, including annual incidence, prevalence, mortality rates, and survival rates, were collected and analyzed according to socioeconomic state (SES) and treatments received.
Results
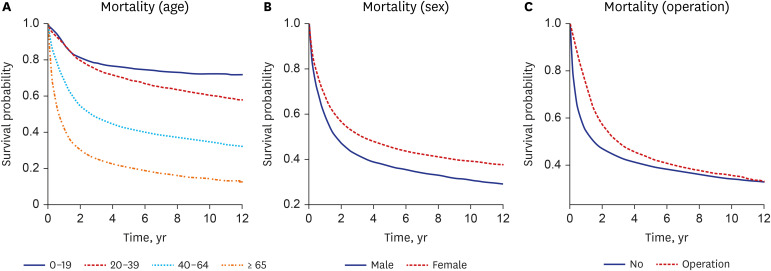
We identified 45,066 newly diagnosed-MG patients from 2007 to 2017, for an age-adjusted incidence of 7.47 per 100,000 people. The mean age at diagnosis was 54 years. The male to female ratio was 1.11. Mortality and survival probability were analyzed among total subjects and in subgroups. The mortality rates were lower in female than that of male patients (hazard ratio, 0.69; 95% confidence interval, 0.67–0.71), and in younger age population and in higher income group. Patients operated had a slightly higher survival rate. The 1-, 3-, 5-, and 10-year survival rates were estimated at 63.4%, 46.2%, 39.4%, and 34.8%, respectively. This is the first population-based study to determine the incidence and prevalence of MG according to epidemiological characteristics in Korea using NHID.
Conclusion
Our study found that female sex and high SES were factors that significantly lowered the mortality rate in MG, and younger groups and operated patients showed significantly higher survival rates.
Keyword
Figure
Reference
-
1. Porter KR, McCarthy BJ, Freels S, Kim Y, Davis FG. Prevalence estimates for primary brain tumors in the United States by age, gender, behavior, and histology. Neuro Oncol. 2010; 12(6):520–527. PMID: 20511189.
Article2. Baker GJ, Yadav VN, Motsch S, Koschmann C, Calinescu AA, Mineharu Y, et al. Mechanisms of glioma formation: iterative perivascular glioma growth and invasion leads to tumor progression, VEGF-independent vascularization, and resistance to antiangiogenic therapy. Neoplasia. 2014; 16(7):543–561. PMID: 25117977.
Article3. Dubrow R, Darefsky AS. Demographic variation in incidence of adult glioma by subtype, United States, 1992-2007. BMC Cancer. 2011; 11(1):325. PMID: 21801393.
Article4. Ostrom QT, Gittleman H, Liao P, Vecchione-Koval T, Wolinsky Y, Kruchko C, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2010-2014. Neuro Oncol. 2017; 19(suppl_5):v1–v88. PMID: 29117289.
Article5. Dho YS, Jung KW, Ha J, Seo Y, Park CK, Won YJ, et al. An updated nationwide epidemiology of primary brain tumors in Republic of Korea, 2013. Brain Tumor Res Treat. 2017; 5(1):16–23. PMID: 28516074.
Article6. Lee CH, Jung KW, Yoo H, Park S, Lee SH. Epidemiology of primary brain and central nervous system tumors in Korea. J Korean Neurosurg Soc. 2010; 48(2):145–152. PMID: 20856664.
Article7. Seo HJ, Oh IH, Yoon SJ. A comparison of the cancer incidence rates between the national cancer registry and insurance claims data in Korea. Asian Pac J Cancer Prev. 2012; 13(12):6163–6168. PMID: 23464424.
Article8. Arora RS, Alston RD, Eden TO, Estlin EJ, Moran A, Birch JM. Age-incidence patterns of primary CNS tumors in children, adolescents, and adults in England. Neuro Oncol. 2009; 11(4):403–413. PMID: 19033157.
Article9. Crocetti E, Trama A, Stiller C, Caldarella A, Soffietti R, Jaal J, et al. Epidemiology of glial and non-glial brain tumours in Europe. Eur J Cancer. 2012; 48(10):1532–1542. PMID: 22227039.
Article10. Ostrom QT, Cioffi G, Gittleman H, Patil N, Waite K, Kruchko C, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro Oncol. 2019; 21(Suppl 5):v1–v100. PMID: 31675094.
Article11. Walker EV, Davis FG. Malignant primary brain and other central nervous system tumors diagnosed in Canada from 2009 to 2013. Neuro Oncol. 2019; 21(3):360–369. PMID: 30649461.
Article12. Wöhrer A, Waldhör T, Heinzl H, Hackl M, Feichtinger J, Gruber-Mösenbacher U, et al. The Austrian Brain Tumour Registry: a cooperative way to establish a population-based brain tumour registry. J Neurooncol. 2009; 95(3):401–411. PMID: 19562257.
Article13. Larjavaara S, Mäntylä R, Salminen T, Haapasalo H, Raitanen J, Jääskeläinen J, et al. Incidence of gliomas by anatomic location. Neuro Oncol. 2007; 9(3):319–325. PMID: 17522333.
Article14. Gousias K, Markou M, Voulgaris S, Goussia A, Voulgari P, Bai M, et al. Descriptive epidemiology of cerebral gliomas in northwest Greece and study of potential predisposing factors, 2005-2007. Neuroepidemiology. 2009; 33(2):89–95. PMID: 19494549.15. Narita Y, Shibui S. Committee of Brain Tumor Registry of Japan Supported by the Japan Neurosurgical Society. Trends and outcomes in the treatment of gliomas based on data during 2001-2004 from the Brain Tumor Registry of Japan. Neurol Med Chir (Tokyo). 2015; 55(4):286–295.
Article16. Rasmussen BK, Hansen S, Laursen RJ, Kosteljanetz M, Schultz H, Nørgård BM, et al. Epidemiology of glioma: clinical characteristics, symptoms, and predictors of glioma patients grade I-IV in the the Danish Neuro-Oncology Registry. J Neurooncol. 2017; 135(3):571–579. PMID: 28861666.
Article17. Khanolkar AR, Ljung R, Talbäck M, Brooke HL, Carlsson S, Mathiesen T, et al. Socioeconomic position and the risk of brain tumour: a Swedish national population-based cohort study. J Epidemiol Community Health. 2016; 70(12):1222–1228. PMID: 27325866.
Article18. Plascak JJ, Fisher JL. Area-based socioeconomic position and adult glioma: a hierarchical analysis of surveillance epidemiology and end results data. PLoS One. 2013; 8(4):e60910. PMID: 23585860.
Article19. Cote DJ, Ostrom QT, Gittleman H, Duncan KR, CreveCoeur TS, Kruchko C, et al. Glioma incidence and survival variations by county-level socioeconomic measures. Cancer. 2019; 125(19):3390–3400. PMID: 31206646.
Article20. Ostrom QT, Cote DJ, Ascha M, Kruchko C, Barnholtz-Sloan JS. Adult glioma incidence and survival by race or ethnicity in the United States from 2000 to 2014. JAMA Oncol. 2018; 4(9):1254–1262. PMID: 29931168.
Article21. Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008; 358(23):2468–2481. PMID: 18525043.
Article22. Bleyer A, Barr R, Hayes-Lattin B, Thomas D, Ellis C, Anderson B, et al. The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer. 2008; 8(4):288–298. PMID: 18354417.
Article23. Alston RD, Geraci M, Eden TO, Moran A, Rowan S, Birch JM. Changes in cancer incidence in teenagers and young adults (ages 13 to 24 years) in England 1979-2003. Cancer. 2008; 113(10):2807–2815. PMID: 18846564.
Article24. Aben KK, van Gaal C, van Gils NA, van der Graaf WT, Zielhuis GA. Cancer in adolescents and young adults (15-29 years): a population-based study in the Netherlands 1989-2009. Acta Oncol. 2012; 51(7):922–933. PMID: 22934554.
Article25. Desandes E, Lacour B, Belot A, Molinie F, Delafosse P, Tretarre B, et al. Cancer incidence and survival in adolescents and young adults in France, 2000-2008. Pediatr Hematol Oncol. 2013; 30(4):291–306. PMID: 23363314.
Article26. Moon EK, Park HJ, Oh CM, Jung KW, Shin HY, Park BK, et al. Cancer incidence and survival among adolescents and young adults in Korea. PLoS One. 2014; 9(5):e96088. PMID: 24789075.
Article27. Ostrom QT, Kinnersley B, Wrensch MR, Eckel-Passow JE, Armstrong G, Rice T, et al. Sex-specific glioma genome-wide association study identifies new risk locus at 3p21.31 in females, and finds sex-differences in risk at 8q24.21. Sci Rep. 2018; 8(1):7352. PMID: 29743610.
Article28. Liu LY, Schaub MA, Sirota M, Butte AJ. Sex differences in disease risk from reported genome-wide association study findings. Hum Genet. 2012; 131(3):353–364. PMID: 21858542.
Article29. Stewart LA. Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet. 2002; 359(9311):1011–1018. PMID: 11937180.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expression of Trans forming Growth Factor-a and Proliferating Cell Nuclear Antigen in Human Gliomas
- Aberrant CpG Islands Hypermethylation Profiles in Malignant Gliomas
- Overcoming Treatment Resistance in High Grade Gliomas
- Surgical Treatment of the Intracranial Gliomas
- Experience Profiling of Fluorescence-Guided Surgery I: Gliomas