Sex-, Age-, and Metabolic Disorder-Dependent Distributions of Selected Inflammatory Biomarkers among Community-Dwelling Adults
- Affiliations
-
- 1Department of Public Health, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Cardiovascular and Metabolic Diseases Etiology Research Center, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2513033
- DOI: http://doi.org/10.4093/dmj.2019.0119
Abstract
Background Inflammatory cytokines are increasingly utilized to detect high-risk individuals for cardiometabolic diseases. However, with large population and assay methodological heterogeneity, no clear reference currently exists.
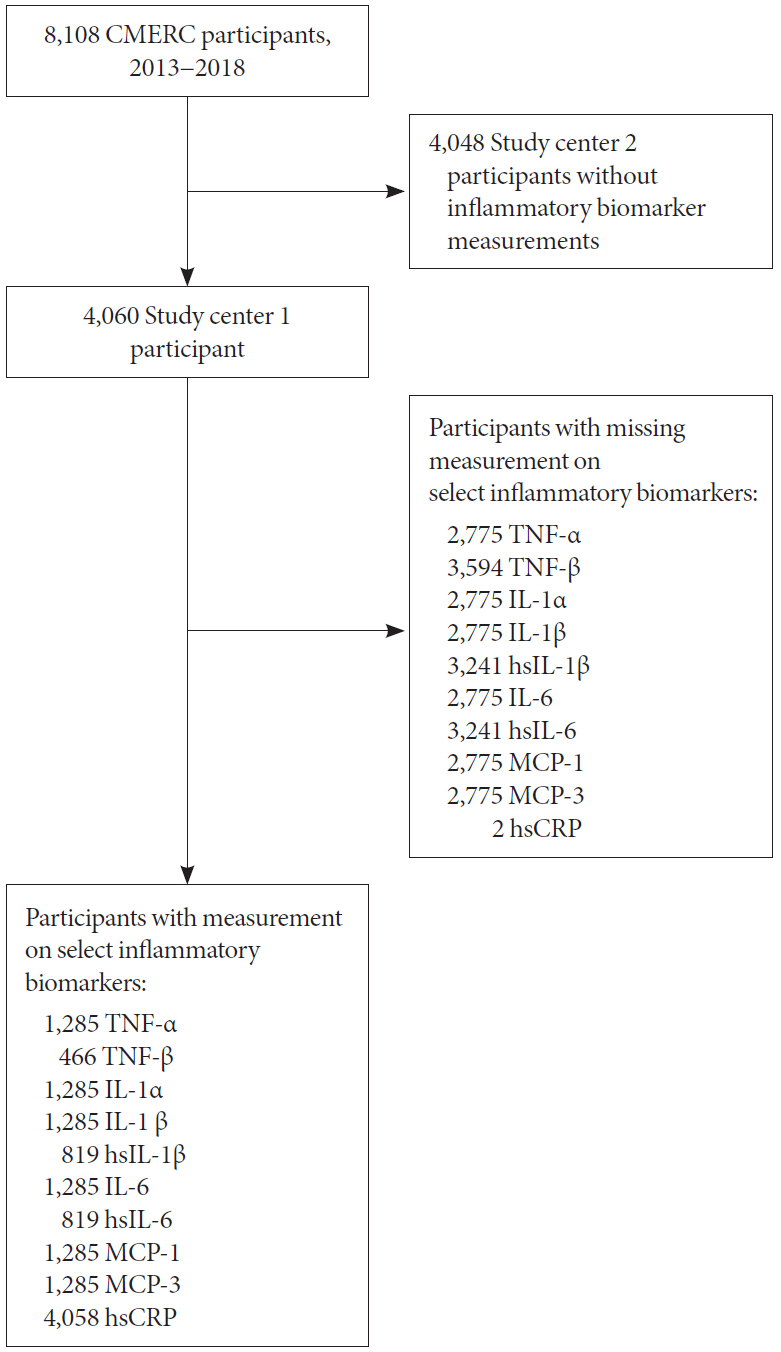
Methods Among participants of the Cardiovascular and Metabolic Diseases Etiology Research Center cohort, of community-dwelling adults aged 30 to 64 without overt cardiovascular diseases, we presented distributions of tumor necrosis factor (TNF)-α and -β, interleukin (IL)-1α, -1β, and 6, monocyte chemoattractant protein (MCP)-1 and -3 and high sensitivity C-reactive protein (hsCRP) with and without non-detectable (ND) measurements using multiplex enzyme-linked immunosorbent assay. Then, we compared each markers by sex, age, and prevalence of type 2 diabetes mellitus, hypertension, and dyslipidemia, using the Wilcoxon Rank-Sum Test.
Results In general, there were inconsistencies in direction and magnitude of differences in distributions by sex, age, and prevalence of cardiometabolic disorders. Overall, the median and the 99th percentiles were higher in men than in women. Older participants had higher TNF-α, high sensitivity IL-6 (hsIL-6), MCP-1, hsCRP, TNF-β, and MCP-3 median, after excluding the NDs. Participants with type 2 diabetes mellitus had higher median for all assayed biomarkers, except for TNF-β, IL-1α, and MCP-3, in which the medians for both groups were 0.00 due to predominant NDs. Compared to normotensive group, participants with hypertension had higher TNF-α, hsIL-6, MCP-1, and hsCRP median. When stratifying by dyslipidemia prevalence, the comparison varied significantly depending on the treatment of NDs.
Conclusion Our findings provide sex-, age-, and disease-specific reference values to improve risk prediction and diagnostic performance for inflammatory diseases in both population- and clinic-based settings.
Figure
Reference
-
1. Popa C, Netea MG, van Riel PL, van der Meer JW, Stalenhoef AF. The role of TNF-alpha in chronic inflammatory conditions, intermediary metabolism, and cardiovascular risk. J Lipid Res. 2007; 48:751–762.2. Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA. 2001; 286:327–334.
Article3. Ridker PM, Rifai N, Stampfer MJ, Hennekens CH. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000; 101:1767–1772.
Article4. Kaptoge S, Seshasai SR, Gao P, Freitag DF, Butterworth AS, Borglykke A, Di Angelantonio E, Gudnason V, Rumley A, Lowe GD, Jørgensen T, Danesh J. Inflammatory cytokines and risk of coronary heart disease: new prospective study and updated meta-analysis. Eur Heart J. 2014; 35:578–589.
Article5. Schöttker B, Herder C, Rothenbacher D, Roden M, Kolb H, Müller H, Brenner H. Proinflammatory cytokines, adiponectin, and increased risk of primary cardiovascular events in diabetic patients with or without renal dysfunction: results from the ESTHER study. Diabetes Care. 2013; 36:1703–1711.
Article6. Koch W, Kastrati A, Bottiger C, Mehilli J, von Beckerath N, Schomig A. Interleukin-10 and tumor necrosis factor gene polymorphisms and risk of coronary artery disease and myocardial infarction. Atherosclerosis. 2001; 159:137–144.
Article7. Lee J, Yoon K, Ryu S, Chang Y, Kim HR. High-normal levels of hs-CRP predict the development of non-alcoholic fatty liver in healthy men. PLoS One. 2017; 12:e0172666.
Article8. Ridker PM. C-reactive protein and the prediction of cardiovascular events among those at intermediate risk: moving an inflammatory hypothesis toward consensus. J Am Coll Cardiol. 2007; 49:2129–2138.9. Parameswaran N, Patial S. Tumor necrosis factor-α signaling in macrophages. Crit Rev Eukaryot Gene Expr. 2010; 20:87–103.
Article10. Tousoulis D, Oikonomou E, Economou EK, Crea F, Kaski JC. Inflammatory cytokines in atherosclerosis: current therapeutic approaches. Eur Heart J. 2016; 37:1723–1732.
Article11. Jia T, Serbina NV, Brandl K, Zhong MX, Leiner IM, Charo IF, Pamer EG. Additive roles for MCP-1 and MCP-3 in CCR2-mediated recruitment of inflammatory monocytes during Listeria monocytogenes infection. J Immunol. 2008; 180:6846–6853.
Article12. Bogavac-Stanojevic N, Jelic-Ivanovic Z, Spasojevic-Kalimanovska V, Spasic S, Kalimanovska-Ostric D. Lipid and inflammatory markers for the prediction of coronary artery disease: a multi-marker approach. Clin Biochem. 2007; 40:1000–1006.13. Fatkhullina AR, Peshkova IO, Koltsova EK. The role of cytokines in the development of atherosclerosis. Biochemistry (Mosc). 2016; 81:1358–1370.
Article14. Ramji DP, Davies TS. Cytokines in atherosclerosis: key players in all stages of disease and promising therapeutic targets. Cytokine Growth Factor Rev. 2015; 26:673–685.
Article15. Ait-Oufella H, Taleb S, Mallat Z, Tedgui A. Recent advances on the role of cytokines in atherosclerosis. Arterioscler Thromb Vasc Biol. 2011; 31:969–979.
Article16. Shim JS, Song BM, Lee JH, Lee SW, Park JH, Choi DP, Lee MH, Ha KH, Kim DJ, Park S, Lee WW, Youm Y, Shin EC, Kim HC. Cohort profile: the cardiovascular and metabolic diseases etiology research center cohort in Korea. Yonsei Med J. 2019; 60:804–810.
Article17. Ko SH, Kim SR, Kim DJ, Oh SJ, Lee HJ, Shim KH, Woo MH, Kim JY, Kim NH, Kim JT, Kim CH, Kim HJ, Jeong IK, Hong EK, Cho JH, Mok JO, Yoon KH. Committee of Clinical Practice Guidelines. Korean Diabetes Association. 2011 Clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J. 2011; 35:431–436.
Article18. Shin J, Park JB, Kim KI, Kim JH, Yang DH, Pyun WB, Kim YG, Kim GH, Chae SC. Guideline Committee of the Korean Society of Hypertension. 2013 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology and diagnosis of hypertension. Clin Hypertens. 2015; 21:1.
Article19. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520.20. Committee for the Korean Guidelines for the Management of Dyslipidemia. 2015 Korean guidelines for the management of dyslipidemia: executive summary (English translation). Korean Circ J. 2016; 46:275–306.21. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001; 285:2486–2497.22. Zhai Y, Shi XM, Fitzgerald SM, Qian HZ, Kraus VB, Sereny M, Hu P, Yin ZX, Xu JW, Zeng Y. High sensitivity C-reactive protein associated with different health predictors in middle-aged and oldest old Chinese. Biomed Environ Sci. 2012; 25:257–266.23. Charuruks N, Laohajinda B, Rujiwanitgun S, Chaiworaporn M. Reference value for C-reactive protein and its distribution pattern in Thai adults. Circ J. 2005; 69:339–344.
Article24. Hirschfield GM, Pepys MB. C-reactive protein and cardiovascular disease: new insights from an old molecule. QJM. 2003; 96:793–807.
Article25. Collerton J, Martin-Ruiz C, Davies K, Hilkens CM, Isaacs J, Kolenda C, Parker C, Dunn M, Catt M, Jagger C, von Zglinicki T, Kirkwood TB. Frailty and the role of inflammation, immunosenescence and cellular ageing in the very old: cross-sectional findings from the Newcastle 85+ Study. Mech Ageing Dev. 2012; 133:456–466.
Article26. Effoe VS, Correa A, Chen H, Lacy ME, Bertoni AG. High-sensitivity C-reactive protein is associated with incident type 2 diabetes among African Americans: the Jackson Heart Study. Diabetes Care. 2015; 38:1694–1700.
Article27. Aniszewska A, Chlodzinska N, Bartkowska K, Winnicka MM, Turlejski K, Djavadian RL. The expression of interleukin-6 and its receptor in various brain regions and their roles in exploratory behavior and stress responses. J Neuroimmunol. 2015; 284:1–9.
Article28. Qi L, Rifai N, Hu FB. Interleukin-6 receptor gene variations, plasma interleukin-6 levels, and type 2 diabetes in U.S. Women. Diabetes. 2007; 56:3075–3081.
Article29. Lopez-Castejon G, Brough D. Understanding the mechanism of IL-1β secretion. Cytokine Growth Factor Rev. 2011; 22:189–195.
Article30. Liu T, Zhang L, Joo D, Sun SC. NF-κB signaling in inflammation. Signal Transduct Target Ther. 2017; 2:17023.
Article31. Rider P, Carmi Y, Guttman O, Braiman A, Cohen I, Voronov E, White MR, Dinarello CA, Apte RN. IL-1α and IL-1β recruit different myeloid cells and promote different stages of sterile inflammation. J Immunol. 2011; 187:4835–4843.
Article32. Di Paolo NC, Shayakhmetov DM. Interleukin 1α and the inflammatory process. Nat Immunol. 2016; 17:906–913.
Article33. Slimani H, Zhai Y, Yousif NG, Ao L, Zeng Q, Fullerton DA, Meng X. Enhanced monocyte chemoattractant protein-1 production in aging mice exaggerates cardiac depression during endotoxemia. Crit Care. 2014; 18:527.
Article34. Hubbard RE, O'Mahony MS, Savva GM, Calver BL, Woodhouse KW. Inflammation and frailty measures in older people. J Cell Mol Med. 2009; 13(9B):3103–3109.
Article35. Acuner Ozbabacan SE, Gursoy A, Nussinov R, Keskin O. The structural pathway of interleukin 1 (IL-1) initiated signaling reveals mechanisms of oncogenic mutations and SNPs in inflammation and cancer. PLoS Comput Biol. 2014; 10:e1003470.
Article36. Han L, Song JH, Yoon JH, Park YG, Lee SW, Choi YJ, Nam SW, Lee JY, Park WS. TNF-α and TNF-β polymorphisms are associated with susceptibility to osteoarthritis in a Korean population. Korean J Pathol. 2012; 46:30–37.
Article37. Svenungsson E, Gunnarsson I, Fei GZ, Lundberg IE, Klareskog L, Frostegard J. Elevated triglycerides and low levels of high-density lipoprotein as markers of disease activity in association with up-regulation of the tumor necrosis factor alpha/tumor necrosis factor receptor system in systemic lupus erythematosus. Arthritis Rheum. 2003; 48:2533–2540.38. Aggarwal BB. Signalling pathways of the TNF superfamily: a double-edged sword. Nat Rev Immunol. 2003; 3:745–756.
Article39. Stephens JM, Pekala PH. Transcriptional repression of the GLUT4 and C/EBP genes in 3T3-L1 adipocytes by tumor necrosis factor-alpha. J Biol Chem. 1991; 266:21839–21845.
Article40. Bruun JM, Lihn AS, Verdich C, Pedersen SB, Toubro S, Astrup A, Richelsen B. Regulation of adiponectin by adipose tissue-derived cytokines: in vivo and in vitro investigations in humans. Am J Physiol Endocrinol Metab. 2003; 285:E527–E533.41. Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res. 2009; 29:313–326.
Article42. Tsou CL, Peters W, Si Y, Slaymaker S, Aslanian AM, Weisberg SP, Mack M, Charo IF. Critical roles for CCR2 and MCP-3 in monocyte mobilization from bone marrow and recruitment to inflammatory sites. J Clin Invest. 2007; 117:902–909.
Article43. Gu L, Okada Y, Clinton SK, Gerard C, Sukhova GK, Libby P, Rollins BJ. Absence of monocyte chemoattractant protein-1 reduces atherosclerosis in low density lipoprotein receptor-deficient mice. Mol Cell. 1998; 2:275–281.
Article44. Boring L, Gosling J, Cleary M, Charo IF. Decreased lesion formation in CCR2-/- mice reveals a role for chemokines in the initiation of atherosclerosis. Nature. 1998; 394:894–897.
Article45. Aiello RJ, Bourassa PA, Lindsey S, Weng W, Natoli E, Rollins BJ, Milos PM. Monocyte chemoattractant protein-1 accelerates atherosclerosis in apolipoprotein E-deficient mice. Arterioscler Thromb Vasc Biol. 1999; 19:1518–1525.
Article46. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001; 56:M146–M156.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Co-occurrence of Frailty, Possible Sarcopenia, and Malnutrition in Community-Dwelling Older Outpatients: A Multicentre Observational Study
- Examination of Factors Associated with Self-Reported Cane Use among Community-Dwelling Older Adults
- Development of a Knowledge Scale of Fall Risk Factors for Community-dwelling Older Adults
- Perceived Benefits and Barriers of Exercise in Community-Dwelling Adults at a Local City in Korea
- Factors Contributing to Low Weight in Community-Dwelling Older Adults