Yeungnam Univ J Med.
2021 Jan;38(1):74-77. 10.12701/yujm.2020.00297.
Transpedal lymphatic embolization for lymphorrhea at the graft harvest site after coronary artery bypass grafting
- Affiliations
-
- 1Department of Radiology, Kyungpook National University Hospital, Daegu, Korea
- 2Department of Radiology, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Department of Thoracic and Cardiovascular Surgery, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2512071
- DOI: http://doi.org/10.12701/yujm.2020.00297
Abstract
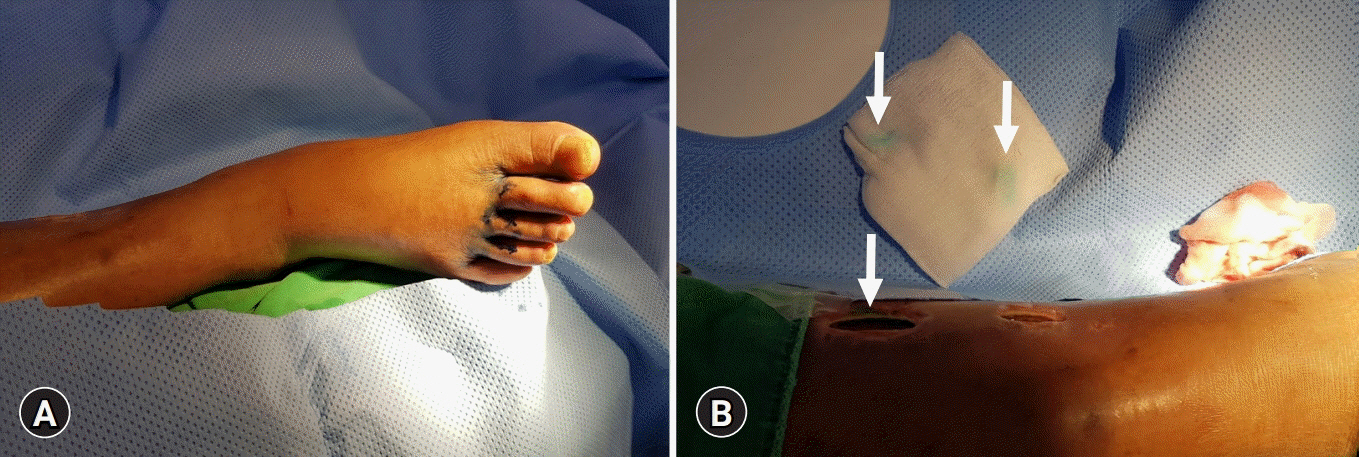
- Lymphorrhea is a rare but potentially severe complication that occurs after various surgical procedures. Untreated lymphorrhea may lead to wound dehiscence, infection, and prolonged hospital stay. Currently, there is no standard effective treatment. Early management usually includes leg elevation, drainage, and pressure dressing. However, these methods are associated with prolonged recovery and high recurrence rates. We report a case of lymphorrhea from a calf wound after endoscopic great saphenous vein (GSV) harvesting for coronary artery bypass grafting (CABG). The patient presented with intractable oozing from the postoperative wound on the right calf. Lymphorrhea perGsisted for 6 weeks despite negative-pressure wound therapy with a long-acting somatostatin. We performed unilateral pedal lymphangiography that confirmed wound lymphorrhea, followed by glue embolization. No recurrence was observed after 8 months of follow-up. This case report demonstrates the successful use of lymphangiography with glue embolization in the control of lymphorrhea after GSV harvesting for CABG.
Keyword
Figure
Reference
-
References
1. Unno N, Yamamoto N, Suzuki M, Tanaka H, Mano Y, Sano M, et al. Intraoperative lymph mapping with preoperative vein mapping to prevent postoperative lymphorrhea following paramalleolar bypass surgery in patients with critical limb ischemia. Surg Today. 2014; 44:436–42.
Article2. Heitink MV, Schurink GWH, de Pont CDJM, van Kroonenburgh MJPG, Veraart JCJM. Lymphedema after greater saphenous vein surgery. Eur J Vasc Endovasc Surg. 2009; 38:656.
Article3. Kos S, Haueisen H, Lachmund U, Roeren T. Lymphangiography: forgotten tool or rising star in the diagnosis and therapy of postoperative lymphatic vessel leakage. Cardiovasc Intervent Radiol. 2007; 30:968–73.
Article4. Rajebi MR, Chaudry G, Padua HM, Dillon B, Yilmaz S, Arnold RW, et al. Intranodal lymphangiography: feasibility and preliminary experience in children. J Vasc Interv Radiol. 2011; 22:1300–5.
Article5. Nadolski GJ, Itkin M. Feasibility of ultrasound-guided intranodal lymphangiogram for thoracic duct embolization. J Vasc Interv Radiol. 2012; 23:613–6.
Article6. Shinaoka A, Koshimune S, Suami H, Yamada K, Kumagishi K, Boyages J, et al. Lower-limb lymphatic drainage pathways and lymph nodes: a CT lymphangiography cadaver study. Radiology. 2020; 294:223–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of lymphatic interventional radiology for postoperative lymphorrhea
- The Right Gastroepiploic Artery Graft for Coronary Artery Bypass Grafting: A 30-Year Experience
- Wrapping of an Ascending Aortic Aneurysm with the Multiple Boot-Straps Technique in a Patient Undergoing Off-Pump Coronary Artery Bypass Grafting
- Off-Pump Coronary Artery Bypass Grafting
- Resuscitated cardiac arrest caused by coronary artery spasm after coronary artery bypass grafting: A case report-