Endocrinol Metab.
2020 Dec;35(4):681-695. 10.3803/EnM.2020.772.
Genetic and Environmental Factors Contributing to Visceral Adiposity in Asian Populations
- Affiliations
-
- 1Department of Internal Medicine, University of Central Florida (UCF) College of Medicine, Burnett School of Biomedical Sciences, Orlando, FL, USA
- KMID: 2510997
- DOI: http://doi.org/10.3803/EnM.2020.772
Abstract
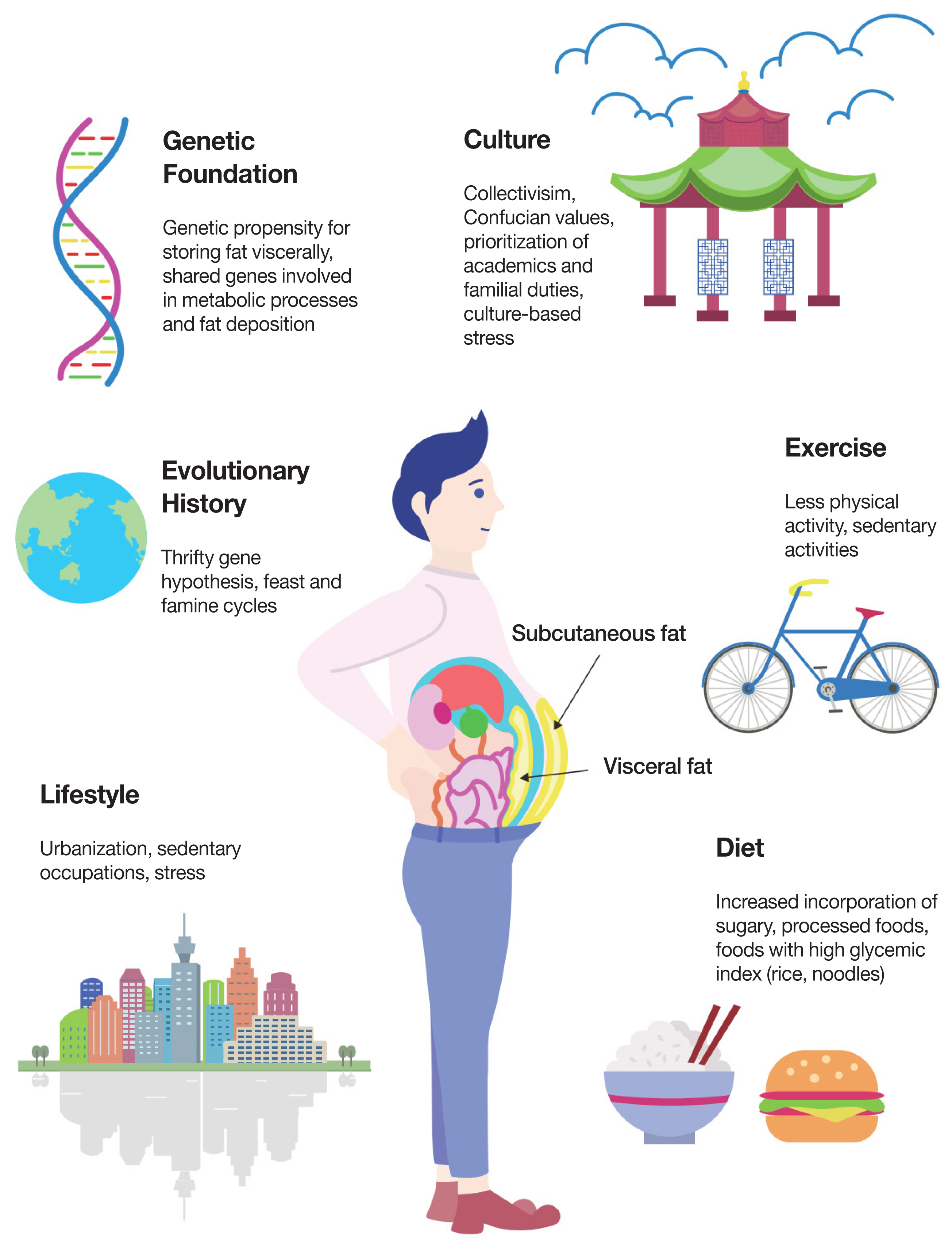
- Obesity-associated metabolic illnesses are increasing at an alarming rate in Asian countries. A common feature observed in the Asian population is a higher incidence of abdominal obesity—the “skinny-fat” Asian syndrome. In this review, we critically evaluate the relative roles of genetics and environmental factors on fat distribution in Asian populations. While there is an upward trend in obesity among most Asian countries, it appears particularly conspicuous in Malaysia. We propose a novel theory, the Malaysian gene-environment multiplier hypothesis, which explains how ancestral variations in feast-and-famine cycles contribute to inherited genetic predispositions that, when acted on by modern-day stressors—most notably, urbanization, westernization, lifestyle changes, dietary transitions, cultural pressures, and stress—contribute to increased visceral adiposity in Asian populations. At present, the major determinants contributing to visceral adiposity in Asians are far from conclusive, but we seek to highlight critical areas for further research.
Keyword
Figure
Reference
-
1. World Health Organization. Obesity and Overweight [Internet]. Geneva: World Health Organization;2020. [cited 2020 Nov 9]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.2. Flatt JP. Use and storage of carbohydrate and fat. Am J Clin Nutr. 1995; 61(4 Suppl):952S–9S.
Article3. Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010; 11:11–8.
Article4. Wang S, Liu Y, Li F, Jia H, Liu L, Xue F. A novel quantitative body shape score for detecting association between obesity and hypertension in China. BMC Public Health. 2015; 15:7.
Article5. Mongraw-Chaffin M, Golden SH, Allison MA, Ding J, Ouyang P, Schreiner PJ, et al. The sex and race specific relationship between anthropometry and body fat composition determined from computed tomography: evidence from the multi-ethnic study of atherosclerosis. PLoS One. 2015; 10:e0139559.
Article6. Bray GA, Bouchard C. Handbook of obesity. 3rd ed. Boca Raton: CRC Press;2014. Chapter 7, Gender, ethnic, and geographic variation in adiposity. p. 75–86.7. Lim U, Ernst T, Buchthal SD, Latch M, Albright CL, Wilkens LR, et al. Asian women have greater abdominal and visceral adiposity than Caucasian women with similar body mass index. Nutr Diabetes. 2011; 1:e6.
Article8. Liu A, Byrne NM, Kagawa M, Ma G, Kijboonchoo K, Nasreddine L, et al. Ethnic differences in body fat distribution among Asian pre-pubertal children: a cross-sectional multicenter study. BMC Public Health. 2011; 11:500.
Article9. Kadowaki S, Miura K, Kadowaki T, Fujiyoshi A, El-Saed A, Masaki KH, et al. International comparison of abdominal fat distribution among four populations: the ERA-JUMP study. Metab Syndr Relat Disord. 2018; 16:166–73.
Article10. Garg SK, Lin F, Kandula N, Ding J, Carr J, Allison M, et al. Ectopic fat depots and coronary artery calcium in South Asians compared with other racial/ethnic groups. J Am Heart Assoc. 2016; 5:e004257.
Article11. Stults-Kolehmainen MA, Stanforth PR, Bartholomew JB, Lu T, Abolt CJ, Sinha R. DXA estimates of fat in abdominal, trunk and hip regions varies by ethnicity in men. Nutr Diabetes. 2013; 3:e64.
Article12. Park YW, Allison DB, Heymsfield SB, Gallagher D. Larger amounts of visceral adipose tissue in Asian Americans. Obes Res. 2001; 9:381–7.
Article13. Wulan SN, Westerterp KR, Plasqui G. Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas. 2010; 65:315–9.
Article14. Slentz CA, Aiken LB, Houmard JA, Bales CW, Johnson JL, Tanner CJ, et al. Inactivity, exercise, and visceral fat. STRRIDE: a randomized, controlled study of exercise intensity and amount. J Appl Physiol (1985). 2005; 99:1613–8.
Article15. Bi X, Loo YT, Henry CJ. Android fat as a determinant of metabolic syndrome: sex differences. Nutrition. 2019; 57:127–32.
Article16. Valsamakis G, Chetty R, Anwar A, Banerjee AK, Barnett A, Kumar S. Association of simple anthropometric measures of obesity with visceral fat and the metabolic syndrome in male Caucasian and Indo-Asian subjects. Diabet Med. 2004; 21:1339–45.
Article17. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843.
Article18. Yajnik CS, Yudkin JS. The Y-Y paradox. Lancet. 2004; 363:163.
Article19. Lotta LA, Wittemans LB, Zuber V, Stewart ID, Sharp SJ, Luan J, et al. Association of genetic variants related to gluteofemoral vs abdominal fat distribution with type 2 diabetes, coronary disease, and cardiovascular risk factors. JAMA. 2018; 320:2553–63.
Article20. Heid IM, Jackson AU, Randall JC, Winkler TW, Qi L, Steinthorsdottir V, et al. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. Nat Genet. 2010; 42:949–60.21. Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, Magi R, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015; 518:187–96.22. Lin X, Qi Q, Zheng Y, Huang T, Lathrop M, Zelenika D, et al. Neuropeptide Y genotype, central obesity, and abdominal fat distribution: the POUNDS LOST trial. Am J Clin Nutr. 2015; 102:514–9.23. Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM Jr. Why are there race/ethnic differences in adult body mass index-adiposity relationships?: a quantitative critical review. Obes Rev. 2016; 17:262–75.
Article24. Lim U, Monroe KR, Buchthal S, Fan B, Cheng I, Kristal BS, et al. Propensity for intra-abdominal and hepatic adiposity varies among ethnic groups. Gastroenterology. 2019; 156:966–75.
Article25. Pulit SL, Karaderi T, Lindgren CM. Sexual dimorphisms in genetic loci linked to body fat distribution. Biosci Rep. 2017; 37:BSR20160184.
Article26. Azuma K, Kadowaki T, Cetinel C, Kadota A, El-Saed A, Kadowaki S, et al. Higher liver fat content among Japanese in Japan compared with non-Hispanic whites in the United States. Metabolism. 2009; 58:1200–7.
Article27. Cook WK, Tseng W, Bautista R, John I. Ethnicity, socioeconomic status, and overweight in Asian American adolescents. Prev Med Rep. 2016; 4:233–7.
Article28. Paley C, Hull H, Ji Y, Toro-Ramos T, Thornton J, Bauer J, et al. Body fat differences by self-reported race/ethnicity in healthy term newborns. Pediatr Obes. 2016; 11:361–8.
Article29. He Q, Horlick M, Thornton J, Wang J, Pierson RN Jr, Heshka S, et al. Sex and race differences in fat distribution among Asian, African-American, and Caucasian prepubertal children. J Clin Endocrinol Metab. 2002; 87:2164–70.
Article30. Freedman DS, Wang J, Thornton JC, Mei Z, Pierson RN Jr, Dietz WH, et al. Racial/ethnic differences in body fatness among children and adolescents. Obesity (Silver Spring). 2008; 16:1105–11.
Article31. Shaw NJ, Crabtree NJ, Kibirige MS, Fordham JN. Ethnic and gender differences in body fat in British schoolchildren as measured by DXA. Arch Dis Child. 2007; 92:872–5.
Article32. Fox A, Feng W, Asal V. What is driving global obesity trends?: globalization or “modernization”? Global Health. 2019; 15:32.
Article33. Jackson P, Spiess WEL, Sultana F. eating, drinking: surviving the international year of global understanding-IYGU. Cham: Springer International Publishing;2016. Chapter, The Nutrition Transition in Developing Asia: Dietary Change, Drivers and Health Impacts. p. 83–8.34. Siddiqui K, Joy SS, Nawaz SS. Impact of early life or intrauterine factors and socio-economic interaction on diabetes: an evidence on thrifty hypothesis. J Lifestyle Med. 2019; 9:92–101.
Article35. Ferreira SR, Lerario DD, Gimeno SG, Sanudo A, Franco LJ; Japanese-Brazilian Diabetes Study Group. Obesity and central adiposity in Japanese immigrants: role of the Western dietary pattern. J Epidemiol. 2002; 12:431–8.
Article36. Shimabukuro M, Higa M, Kinjo R, Yamakawa K, Tanaka H, Kozuka C, et al. Effects of the brown rice diet on visceral obesity and endothelial function: the BRAVO study. Br J Nutr. 2014; 111:310–20.
Article37. Krittanawong C, Tunhasiriwet A, Zhang H, Prokop LJ, Chirapongsathorn S, Sun T, et al. Is white rice consumption a risk for metabolic and cardiovascular outcomes?: a systematic review and meta-analysis. Heart Asia. 2017; 9:e010909.
Article38. Seo MH, Lee WY, Kim SS, Kang JH, Kang JH, Kim KK, et al. 2018 Korean Society for the Study of Obesity guideline for the management of obesity in Korea. J Obes Metab Syndr. 2019; 28:40–5.
Article39. Shin JH, Jung S, Kim SA, Kang MS, Kim MS, Joung H, et al. Differential effects of typical Korean versus American-style diets on gut microbial composition and metabolic profile in healthy overweight Koreans: a randomized crossover trial. Nutrients. 2019; 11:2450.
Article40. Kyrou I, Tsigos C. Stress hormones: physiological stress and regulation of metabolism. Curr Opin Pharmacol. 2009; 9:787–93.
Article41. Drapeau V, Therrien F, Richard D, Tremblay A. Is visceral obesity a physiological adaptation to stress? Panminerva Med. 2003; 45:189–95.42. Chrousos GP. The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: neuro-endocrine and target tissue-related causes. Int J Obes Relat Metab Disord. 2000; 24(Suppl 2):S50–5.
Article43. Vinet A, Obert P, Courteix D, Chapier R, Lesourd B, Verney J, et al. Different modalities of exercise improve macrovascular function but not microvascular function in metabolic syndrome: the RESOLVE randomized trial. Int J Cardiol. 2018; 267:165–70.
Article44. Irving BA, Davis CK, Brock DW, Weltman JY, Swift D, Barrett EJ, et al. Effect of exercise training intensity on abdominal visceral fat and body composition. Med Sci Sports Exerc. 2008; 40:1863–72.
Article45. Hunter GR, Brock DW, Byrne NM, Chandler-Laney PC, Del Corral P, Gower BA. Exercise training prevents regain of visceral fat for 1 year following weight loss. Obesity (Silver Spring). 2010; 18:690–5.
Article46. Rimmele U, Zellweger BC, Marti B, Seiler R, Mohiyeddini C, Ehlert U, et al. Trained men show lower cortisol, heart rate and psychological responses to psychosocial stress compared with untrained men. Psychoneuroendocrinology. 2007; 32:627–35.
Article47. Milani RV, Lavie CJ. Reducing psychosocial stress: a novel mechanism of improving survival from exercise training. Am J Med. 2009; 122:931–8.
Article48. Mikkelsen K, Stojanovska L, Polenakovic M, Bosevski M, Apostolopoulos V. Exercise and mental health. Maturitas. 2017; 106:48–56.
Article49. Kennedy G, Hardman RJ, Macpherson H, Scholey AB, Pipingas A. How does exercise reduce the rate of age-associated cognitive decline?: a review of potential mechanisms. J Alzheimers Dis. 2017; 55:1–18.
Article50. Williams ED, Stamatakis E, Chandola T, Hamer M. Assessment of physical activity levels in South Asians in the UK: findings from the Health Survey for England. J Epidemiol Community Health. 2011; 65:517–21.
Article51. Owen CG, Nightingale CM, Rudnicka AR, Cook DG, Ekelund U, Whincup PH. Ethnic and gender differences in physical activity levels among 9–10-year-old children of white European, South Asian and African-Caribbean origin: the Child Heart Health Study in England (CHASE Study). Int J Epidemiol. 2009; 38:1082–93.
Article52. Kandula NR, Lauderdale DS. Leisure time, non-leisure time, and occupational physical activity in Asian Americans. Ann Epidemiol. 2005; 15:257–65.
Article53. Misra A, Nigam P, Hills AP, Chadha DS, Sharma V, Deepak KK, et al. Consensus physical activity guidelines for Asian Indians. Diabetes Technol Ther. 2012; 14:83–98.
Article54. Babakus WS, Thompson JL. Physical activity among South Asian women: a systematic, mixed-methods review. Int J Behav Nutr Phys Act. 2012; 9:150.
Article55. Bhatnagar P, Shaw A, Foster C. Generational differences in the physical activity of UK South Asians: a systematic review. Int J Behav Nutr Phys Act. 2015; 12:96.
Article56. Horne M, Tierney S. What are the barriers and facilitators to exercise and physical activity uptake and adherence among South Asian older adults: a systematic review of qualitative studies. Prev Med. 2012; 55:276–84.
Article57. Waidyatilaka I, Lanerolle P, Wickremasinghe R, Atukorala S, Somasundaram N, de Silva A. Sedentary behaviour and physical activity in South Asian women: time to review current recommendations? PLoS One. 2013; 8:e58328.
Article58. Smith L, Aggio D, Hamer M. Longitudinal patterns in objective physical activity and sedentary time in a multi-ethnic sample of children from the UK. Pediatr Obes. 2018; 13:120–6.
Article59. Smith L, Lopez Sanchez GF, Diaz Suarez A, Stubbs B, Dowling M, Scruton A, et al. Barriers and facilitators of physical activity in children of a South Asian ethnicity. Sustainability. 2018; 10:761.
Article60. Carver A, Akram M, Barnett A, Mellecker R, Cerin E. Socioeconomic status and physical activity among mothers of young children in an Asian city: the mediating role of household activities and domestic help. Int J Environ Res Public Health. 2020; 17:2498.
Article61. Yan Z, Cardinal BJ. Association of Asian/Asian-American immigrants physical activity behavior and length of residence in the U.S. J Behav Health. 2019; 8:66–70.
Article62. Neel JV. Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet. 1962; 14:353–62.63. Speakman JR. Thrifty genes for obesity, an attractive but flawed idea, and an alternative perspective: the ‘drifty gene’ hypothesis. Int J Obes (Lond). 2008; 32:1611–7.
Article64. Hales CN, Barker DJ. Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis: 1992. Int J Epidemiol. 2013; 42:1215–22.65. Stoger R. The thrifty epigenotype: an acquired and heritable predisposition for obesity and diabetes? Bioessays. 2008; 30:156–66.
Article66. Ozanne SE, Constancia M. Mechanisms of disease: the developmental origins of disease and the role of the epigenotype. Nat Clin Pract Endocrinol Metab. 2007; 3:539–46.
Article67. Li Y, He Y, Qi L, Jaddoe VW, Feskens EJ, Yang X, et al. Exposure to the Chinese famine in early life and the risk of hyperglycemia and type 2 diabetes in adulthood. Diabetes. 2010; 59:2400–6.
Article68. De Rooij SR, Painter RC, Phillips DI, Osmond C, Michels RP, Godsland IF, et al. Impaired insulin secretion after prenatal exposure to the Dutch famine. Diabetes Care. 2006; 29:1897–901.
Article69. Tobi EW, Goeman JJ, Monajemi R, Gu H, Putter H, Zhang Y, et al. DNA methylation signatures link prenatal famine exposure to growth and metabolism. Nat Commun. 2014; 5:5592.
Article70. Whitelaw NC, Whitelaw E. How lifetimes shape epigenotype within and across generations. Hum Mol Genet. 2006; 15(Spec No 2):R131–7.
Article71. Wells JC. Commentary: why are South Asians susceptible to central obesity?: the El Nino hypothesis. Int J Epidemiol. 2007; 36:226–7.72. Kaur N. Malaysia and WHO call for more investment in primary health care the 21st century Kuala Lumpur, Malaysia [Internet]. Geneva: World Health Organization;2019. [cited 2020 Nov 9]. Available from: https://www.who.int/malaysia/news/detail/08-04-2019-malaysia-and-who-call-for-more-investment-in-primary-health-care-the-21st-century.73. Ritchie H, Roser M. Obesity [Internet]. ourworldindata. 2018. [cited 2020 Nov 9]. Available from: https://ourworldindata.org/obesity.74. Law LS, Sulaiman N, Gan WY, Adznam SN, Mohd Taib MN. Predictors of overweight and obesity and its consequences among Senoi Orang Asli (indigenous people) women in Perak, Malaysia. Int J Environ Res Public Health. 2020; 17:2354.
Article75. Noor MI. The nutrition and health transition in Malaysia. Public Health Nutr. 2002; 5(1A):191–5.
Article76. Roser M. Economic growth: our world in data [Internet]. ourworldindata. 2013. [cited 2020 Nov 9]. Available from: https://ourworldindata.org/economic-growth.77. Ritchie H, Roser M. Urbanization [Internet]. ourworldindata. 2018. [cited 2020 Nov 9]. Available from: https://ourworldindata.org/urbanization.78. Koo HC, Hadirah Z, Airina A, Nurul Alifatul Amrina R, Faziela N. Effect of nutrient intakes on anthropometric profiles among university students from a selected private University in Klang Valley, Malaysia. Afr Health Sci. 2019; 19:2243–51.
Article79. Chan YY, Sooryanarayana R, Mohamad Kasim N, Lim KK, Cheong SM, Kee CC, et al. Prevalence and correlates of physical inactivity among older adults in Malaysia: findings from the National Health and Morbidity Survey (NHMS) 2015. Arch Gerontol Geriatr. 2019; 81:74–83.
Article80. Mitra SR, Tan PY, Amini F. Association of ADRB2 rs1042713 with obesity and obesity-related phenotypes and its interaction with dietary fat in modulating glycaemic indices in Malaysian adults. J Nutr Metab. 2019; 2019:8718795.81. Kayser M, Lao O, Saar K, Brauer S, Wang X, Nurnberg P, et al. Genome-wide analysis indicates more Asian than Melanesian ancestry of Polynesians. Am J Hum Genet. 2008; 82:194–8.
Article82. Central Intelligence Agency. The world factbook: obesity adult prevalence rate [Internet]. CIA;2016. [cited 2020 Nov 9]. Available from: https://www.cia.gov/library/publications/the-world-factbook/rankorder/2228rank.html.83. The astonishing story of Nauru, the tiny island nation with the world’s highest rates of type 2 diabetes [Internet]. Diabetes.co.uk. 2019. [cited 2020 Nov 9]. Available from: https://www.diabetes.co.uk/in-depth/i-have-seen-so-many-funerals-for-such-a-small-island-the-astonishing-story-of-nauru-the-tiny-island-nation-with-the-worlds-highest-rates-of-type-2-diabetes.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults
- Association between Blood Mercury Level and Visceral Adiposity in Adults
- Changing Epidemiology and Future Challenges of Inflammatory Bowel Disease in Asia
- Visceral Obesity
- Obesity : Genetic vs Environmental Factors