Neonatal Med.
2020 Nov;27(4):187-191. 10.5385/nm.2020.27.4.187.
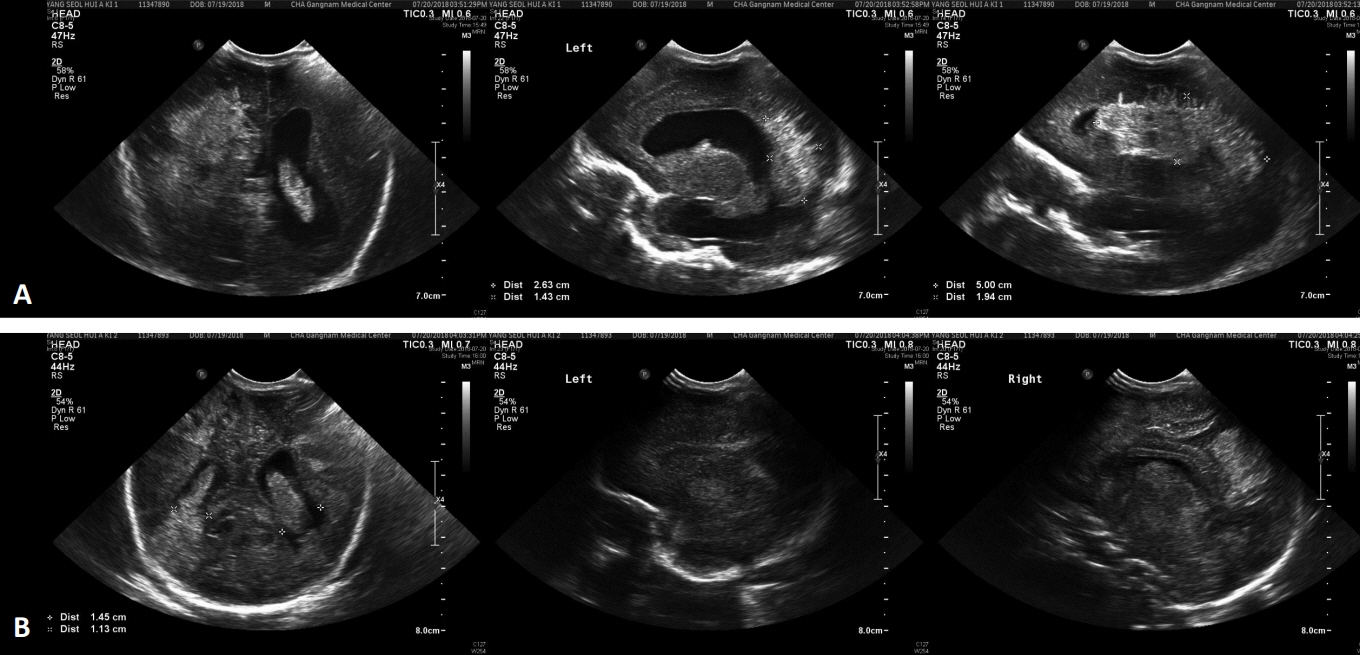
Acute Fetomaternal Hemorrhage Confirmed by Maternal Alfa-Fetoprotein in Monochorionic Diamniotic Neonates under 1,500 g
- Affiliations
-
- 1Department of Pediatrics, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 2Department of Pediatrics, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea
- 3Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
- KMID: 2510824
- DOI: http://doi.org/10.5385/nm.2020.27.4.187
Abstract
- Fetomaternal hemorrhage (FMH) is due to the entry of fetal blood into the maternal circulation. Although very rare, FMH complicates pregnancies, presents with severe symptoms, and leads to fetal death. Majority of FMH cases are idiopathic and difficult to diagnose. The known used diagnostic tests are Kleihauer-Betke Test (KBT) and flow cytometry, which can detect fetal hemoglobin in the maternal blood. However, such methods have limited use because of low sensitivity, labor-intensive and error-susceptible procedures, poor reproducibility, and tendency to overestimate the FMH volume. Other tests include high performance liquid chromatography (HPLC) and alpha-fetoprotein (AFP) tests, which can be as favorable to confirm FMH as KBT. However, in case of acute FMH, the diagnostic results of KBT, flow cytometry, and HPLC may be false negative. AFP test is a noninvasive, fast, easily assessable, adjuvant, and confirmatory diagnostic test. Published Korean articles show confirmed FMH by KBT or HPLC in singleton late-preterm and term neonates. Herein, we report a case of monochorionic diamniotic twin neonates (birth weight <1,500 g) who presented borderline fetal hemoglobin level because of acute FMH and were diagnosed with FMH by maternal AFP. Our experience of diagnosing FMH rapidly by AFP test will be very helpful to clinicians for the prevention and treatment of FMH during pregnancy.
Keyword
Figure
Reference
-
1. Menendez Hernando C, Chacon Aguilar R, Farinas Salto M, Perez Crespo R, Martin Molina R, Moreno Novillo R, et al. Severe neonatal anemia due to fetomaternal hemorrhage: an ilustrative case. Arch Argent Pediatr. 2019; 117:e142–6.2. Solomonia N, Playforth K, Reynolds EW. Fetal-maternal hemorrhage: a case and literature review. AJP Rep. 2012; 2:7–14.3. Ahmed M, Abdullatif M. Fetomaternal transfusion as a cause of severe fetal anemia causing early neonatal death: a case report. Oman Med J. 2011; 26:444–6.4. Weisberg L, Kingdom J, Keating S, Ryan G, Seaward G, Kelly E, et al. Treatment options in fetomaternal hemorrhage: four case studies. J Obstet Gynaecol Can. 2004; 26:893–8.5. Den Besten G, van der Weide K, Schuerman FA, Michael Cotten C, Rondeel JM. Establishing the cause of anemia in a premature newborn infant. Lab Med. 2018; 49:e74–7.6. Thomas A, Mathew M, Unciano Moral E, Vaclavinkova V. Acute massive fetomaternal hemorrhage: case reports and review of the literature. Acta Obstet Gynecol Scand. 2003; 82:479–80.7. Doshi K, Shastry S, Shivhare A, Raturi M. Cellular mimicry in Kleihauer-Betke assay. Glob J Transfus Med. 2016; 1:85–7.8. Duguid JK, Bromilow IM. Laboratory measurement of fetomaternal hemorrhage and its clinical relevance. Transfus Med Rev. 1999; 13:43–8.9. Stefanovic V. Fetomaternal hemorrhage complicated pregnancy: risks, identification, and management. Curr Opin Obstet Gynecol. 2016; 28:86–94.10. Scientific subcommittee of the Australian & New Zealand Society of Blood Transfusion Inc. Guidelines for laboratory assessment of fetomaternal haemorrhage. Sydney: The Society;2002. p. 1–14.11. Kim YA, Makar RS. Detection of fetomaternal hemorrhage. Am J Hematol. 2012; 87:417–23.12. Choi JW, Oh JH, Seok JE, Lee YJ, Oh YK. A case of matemal hemorrhage. J Korean Soc Neonatol. 1999; 6:272–5.13. Kim HK, Choi MY, Yoon HS, Yun BY, Bae SW, Son DW. Clinical study on massive fetomaternal hemorrhage. Korean J Perinatol. 2001; 12:267–73.14. Lee CH, Kim JK, Han MK, Kim JW, Lee JJ. Two cases of massive fetomaternal hemorrhage treated by exchange transfusion. Korean J Perinatol. 2008; 19:203–8.15. Park HC, Park SK, Choi MS. Neonatal severe anemia due to massive fetomaternal hemorrhage. Perinatology. 2019; 30:40–5.16. Giacoia GP. Severe fetomaternal hemorrhage: a review. Obstet Gynecol Surv. 1997; 52:372–80.17. Maier JT, Schalinski E, Schneider W, Gottschalk U, Hellmeyer L. Fetomaternal hemorrhage (FMH), an update: review of literature and an illustrative case. Arch Gynecol Obstet. 2015; 292:595–602.18. Stroustrup A, Plafkin C. A pilot prospective study of fetomaternal hemorrhage identified by anemia in asymptomatic neonates. J Perinatol. 2016; 36:366–9.19. Verco CJ, Jones WR. Monoamniotic twin pregnancy complicated by massive fetal-maternal haemorrhage. Aust N Z J Obstet Gynaecol. 1981; 21:186–7.20. Watanabe N, Jwa SC, Ozawa N, Sago H. Sinusoidal heart rate patterns as a manifestation of massive fetomaternal hemorrhage in a monochorionic-diamniotic twin pregnancy: a case report. Fetal Diagn Ther. 2010; 27:168–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of massive fetomaternal hemorrhage treated by exchange transfusion
- Neonatal Severe Anemia Due to Massive Fetomaternal Hemorrhage
- Fetomaternal hemorrhage caused by an intraplacental choriocarcinoma
- Prediction of Amnionicity Using the Number of Yolk Sacs in Monochorionic Multifetal Pregnancy
- A Case of Stillbirth Due to Fetomaternal Transfusion