Neonatal Med.
2020 Nov;27(4):159-166. 10.5385/nm.2020.27.4.159.
Neurodevelopmental Outcomes of Moderate-to-Late Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- KMID: 2510820
- DOI: http://doi.org/10.5385/nm.2020.27.4.159
Abstract
- Purpose
Preterm infants are known to be at a risk of neurodevelopmental delay; however, limited data are available on the outcomes of moderate-to-late preterm (MLPT) infants (born at 32 to 36 weeks’ gestation). The Korean Developmental Screening Test (K-DST) for infants and children is a recently designed screening test for Korean infants and children. The current study aimed to evaluate the neurodevelopmental outcomes of MLPT infants and investigate the risk factors associated with neurodevelopmental delay.
Methods
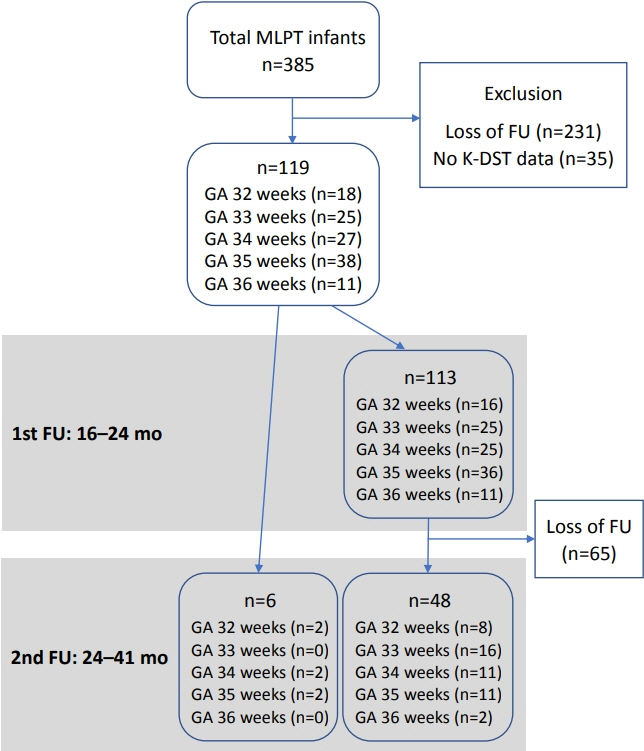
A total of 119 MLPT infants admitted to a neonatal intensive care unit (NICU) of a tertiary hospital in Korea were enrolled. The infants were assessed during two follow-up periods (first: 16 to 24 months of corrected age; second: 24 to 41 months of corrected age). The perinatal factors in the NICU that were associated with delayed development were analyzed.
Results
In all sections of the K-DST, the proportion of infants with developmental delay was higher in the second period (5.6% to 9.3%) than in the first period (0.9% to 5.4%). A total of 10% to 17% of the infants presented with persistent delay throughout the two periods based on five sections of the K-DST. Male sex, oxygen therapy duration, and younger maternal age were the risk factors affecting at least one section during the second period.
Conclusion
MLPT infants showed greater developmental delay than the general infant population. Considering that early intervention is important for good longterm outcomes, close observation of male MLPT infants and MLPT infants who received oxygen therapy is warranted.
Keyword
Figure
Reference
-
1. Raju TN, Higgins RD, Stark AR, Leveno KJ. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics. 2006; 118:1207–14.2. March of Dimes Birth Defects Foundation; World Health Organization; Partnership for Maternal Newborn & Child Health; Save the Children. Born too soon: the global action report on preterm birth. Geneva: World Health Organization;2012.3. Cheong JL, Doyle LW, Burnett AC, Lee KJ, Walsh JM, Potter CR, et al. Association between moderate and late preterm birth and neurodevelopment and social-emotional development at age 2 years. JAMA Pediatr. 2017; 171:e164805.4. Johnson S, Matthews R, Draper ES, Field DJ, Manktelow BN, Marlow N, et al. Early emergence of delayed social competence in infants born late and moderately preterm. J Dev Behav Pediatr. 2015; 36:690–9.5. Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR. Differences in mortality between late-preterm and term singleton infants in the United States, 1995-2002. J Pediatr. 2007; 151:450–6.6. Ohgi S, Fukuda M, Akiyama T, Gima H. Effect of an early intervention programme on low birthweight infants with cerebral injuries. J Paediatr Child Health. 2004; 40:689–95.7. Resnick MB, Armstrong S, Carter RL. Developmental intervention program for high-risk premature infants: effects on development and parent-infant interactions. J Dev Behav Pediatr. 1988; 9:73–8.8. Korea Centers for Disease Control and Prevention. Korean-development screening test for infants and children. Cheongju: Korea Centers for Disease Control and Prevention;2014.9. Yim CH, Kim GH, Eun BL. Usefulness of the Korean Developmental Screening Test for infants and children for the evaluation of developmental delay in Korean infants and children: a single-center study. Korean J Pediatr. 2017; 60:312–9.10. Pascal A, Govaert P, Oostra A, Naulaers G, Ortibus E, Van den Broeck C. Neurodevelopmental outcome in very preterm and very-low-birthweight infants born over the past decade: a meta-analytic review. Dev Med Child Neurol. 2018; 60:342–55.11. World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision. 2nd ed. Geneva: WHO;2004.12. Sung IK, Vohr B, Oh W. Growth and neurodevelopmental outcome of very low birth weight infants with intrauterine growth retardation: comparison with control subjects matched by birth weight and gestational age. J Pediatr. 1993; 123:618–24.13. Vohr BR, Wright LL, Poole WK, McDonald SA. Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks’ gestation between 1993 and 1998. Pediatrics. 2005; 116:635–43.14. Jin JH, Yoon SW, Song J, Kim SW, Chung HJ. Long-term cognitive, executive, and behavioral outcomes of moderate and late preterm at school age. Clin Exp Pediatr. 2020; 63:219–25.15. Suh CR, Sohn SY, Kim GH, Jung SK, Eun BL. Single-center experience of the Korean-Developmental Screening Test for infants and children. Korean J Pediatr. 2016; 59:483–49.16. Chan E, Leong P, Malouf R, Quigley MA. Long-term cognitive and school outcomes of late-preterm and early-term births: a systematic review. Child Care Health Dev. 2016; 42:297–312.17. Chyi LJ, Lee HC, Hintz SR, Gould JB, Sutcliffe TL. School outcomes of late preterm infants: special needs and challenges for infants born at 32 to 36 weeks gestation. J Pediatr. 2008; 153:25–31.18. Johnson S, Evans TA, Draper ES, Field DJ, Manktelow BN, Marlow N, et al. Neurodevelopmental outcomes following late and moderate prematurity: a population-based cohort study. Arch Dis Child Fetal Neonatal Ed. 2015; 100:F301–8.19. Petrini JR, Dias T, McCormick MC, Massolo ML, Green NS, Escobar GJ. Increased risk of adverse neurological development for late preterm infants. J Pediatr. 2009; 154:169–76.20. Gargus RA, Vohr BR, Tyson JE, High P, Higgins RD, Wrage LA, et al. Unimpaired outcomes for extremely low birth weight infants at 18 to 22 months. Pediatrics. 2009; 124:112–21.21. Hirvonen M, Ojala R, Korhonen P, Haataja P, Eriksson K, Gissler M, et al. Visual and hearing impairments after preterm birth. Pediatrics. 2018; 142:e20173888.22. Leversen KT, Sommerfelt K, Ronnestad A, Kaaresen PI, Farstad T, Skranes J, et al. Prediction of neurodevelopmental and sensory outcome at 5 years in Norwegian children born extremely preterm. Pediatrics. 2011; 127:e630–8.23. Serenius F, Kallen K, Blennow M, Ewald U, Fellman V, Holmstrom G, et al. Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA. 2013; 309:1810–20.24. Guihard-Costa AM, Larroche JC. Differential growth between the fetal brain and its infratentorial part. Early Hum Dev. 1990; 23:27–40.25. Kapellou O, Counsell SJ, Kennea N, Dyet L, Saeed N, Stark J, et al. Abnormal cortical development after premature birth shown by altered allometric scaling of brain growth. PLoS Med. 2006; 3:e265.26. Hintz SR, Kendrick DE, Vohr BR, Kenneth Poole W, Higgins RD; Nichd Neonatal Research Network. Gender differences in neurodevelopmental outcomes among extremely preterm, extremely-low-birthweight infants. Acta Paediatr. 2006; 95:1239–48.27. Reiss AL, Kesler SR, Vohr B, Duncan CC, Katz KH, Pajot S, et al. Sex differences in cerebral volumes of 8-year-olds born preterm. J Pediatr. 2004; 145:242–9.28. Anderson PJ, Doyle LW. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin Perinatol. 2006; 30:227–32.29. Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005; 116:1353–60.30. Hintz SR, Kendrick DE, Vohr BR, Poole WK, Higgins RD; National Institute of Child Health and Human Development Neonatal Research Network. Changes in neurodevelopmental outcomes at 18 to 22 months’ corrected age among infants of less than 25 weeks' gestational age born in 1993-1999. Pediatrics. 2005; 115:1645–51.31. Natarajan G, Pappas A, Shankaran S, Kendrick DE, Das A, Higgins RD, et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum Dev. 2012; 88:509–15.32. Trittmann JK, Nelin LD, Klebanoff MA. Bronchopulmonary dysplasia and neurodevelopmental outcome in extremely preterm neonates. Eur J Pediatr. 2013; 172:1173–80.33. Vohr BR, Tyson JE, Wright LL, Perritt RL, Li L, Poole WK, et al. Maternal age, multiple birth, and extremely low birth weight infants. J Pediatr. 2009; 154:498–503.34. DiLabio J, Zwicker JG, Sherlock R, Daspal S, Shah PS, Shah V, et al. Maternal age and long-term neurodevelopmental outcomes of preterm infants < 29 weeks gestational age. J Perinatol. 2020; Jul. 21. [Epub]. https://doi.org/10.1038/s41372-020-0735-9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurodevelopmental outcomes of preterm infants
- Neurodevelopmental Outcomes and Brain Volumetric Analysis of Low-Grade Intraventricular Hemorrhage
- Comparisons of Clinical Characteristics Affecting Readmission between Late Preterm Infants and Moderate Preterm Infants or Full-Term Infants
- Growth patterns of preterm infants in Korea
- Neurodevelopmental Outcomes of Extremely Preterm Infants