Korean J Gastroenterol.
2021 Jan;77(1):30-34. 10.4166/kjg.2020.130.
Case of Crohn’s Disease Initially Misdiagnosed as Intestinal Tuberculosis Due to Active Pulmonary Tuberculosis
- Affiliations
-
- 1Department of Internal Medicine, Comprehensive Medical Examination Center, Busan, Korea
- 2Good Samsun Hospital, Busan, Korea
- KMID: 2510773
- DOI: http://doi.org/10.4166/kjg.2020.130
Abstract
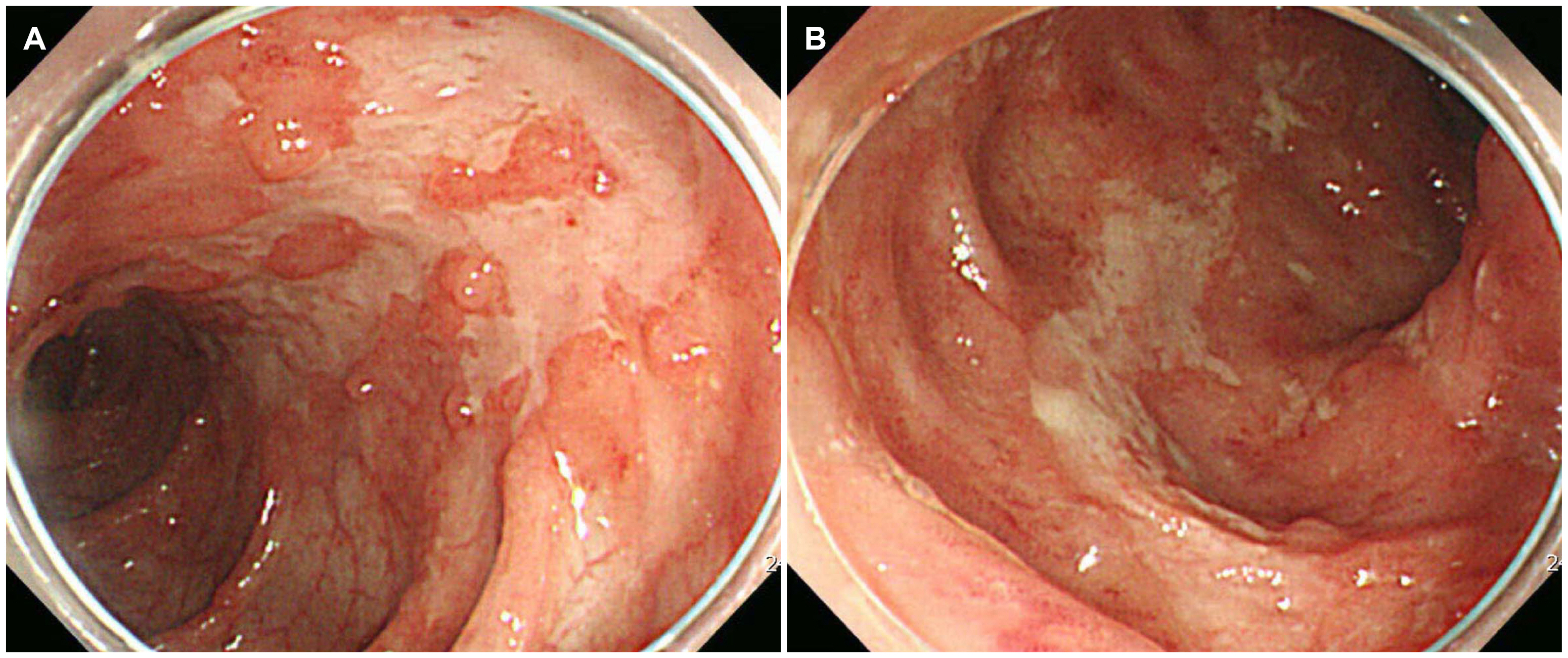
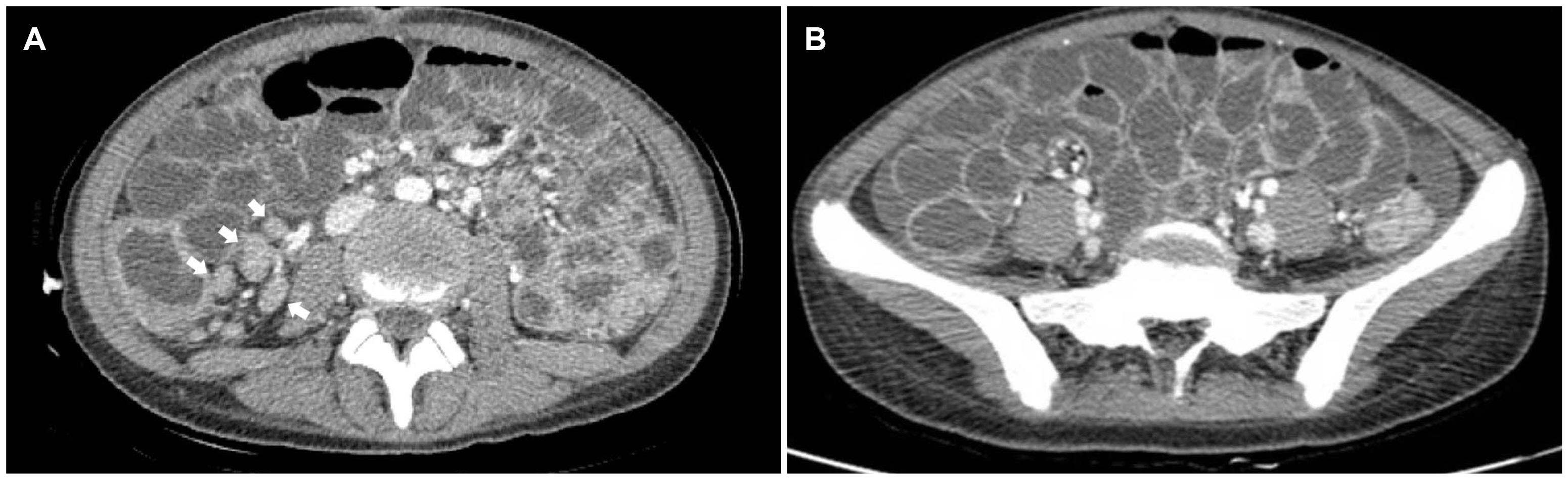
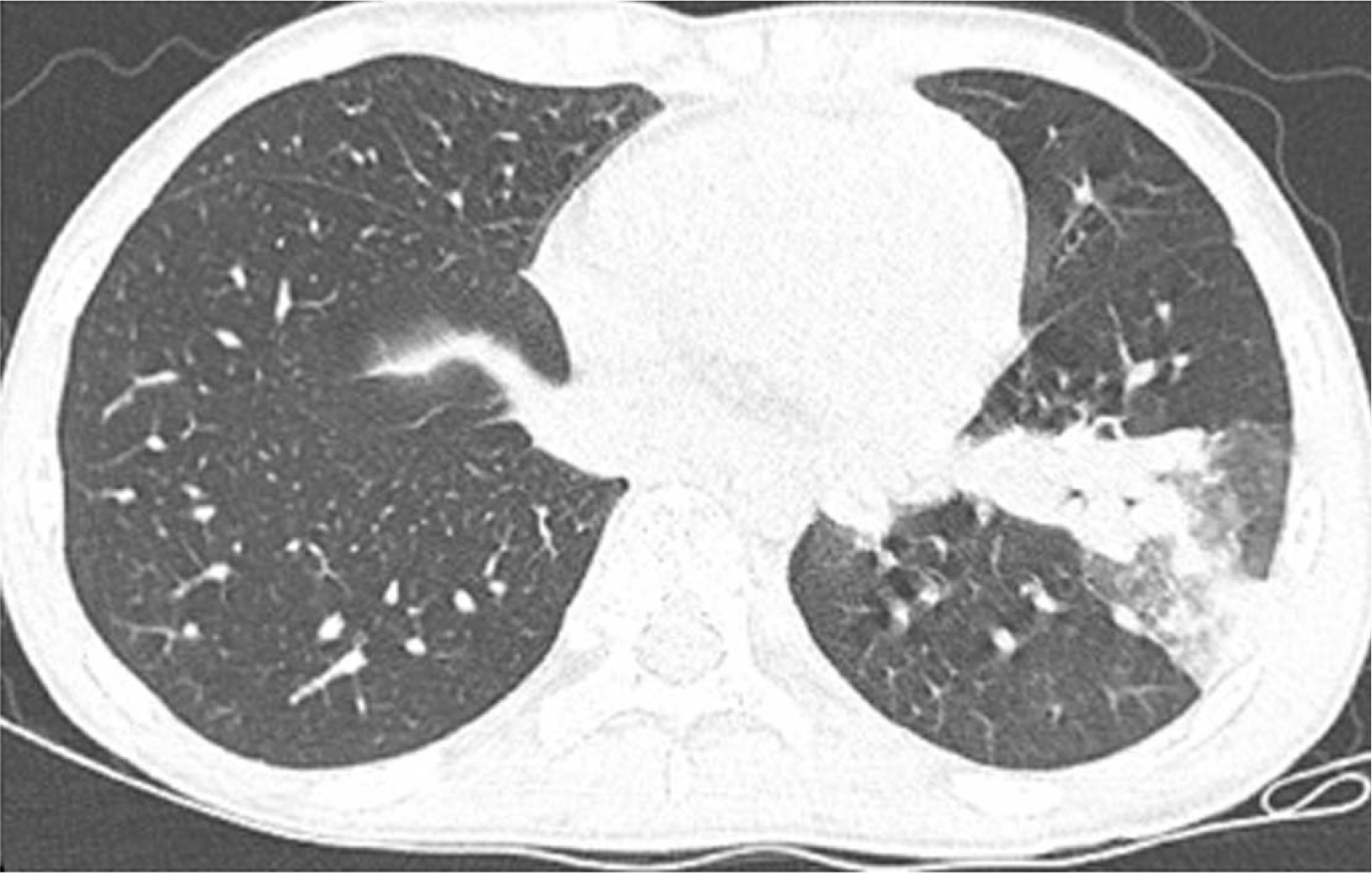
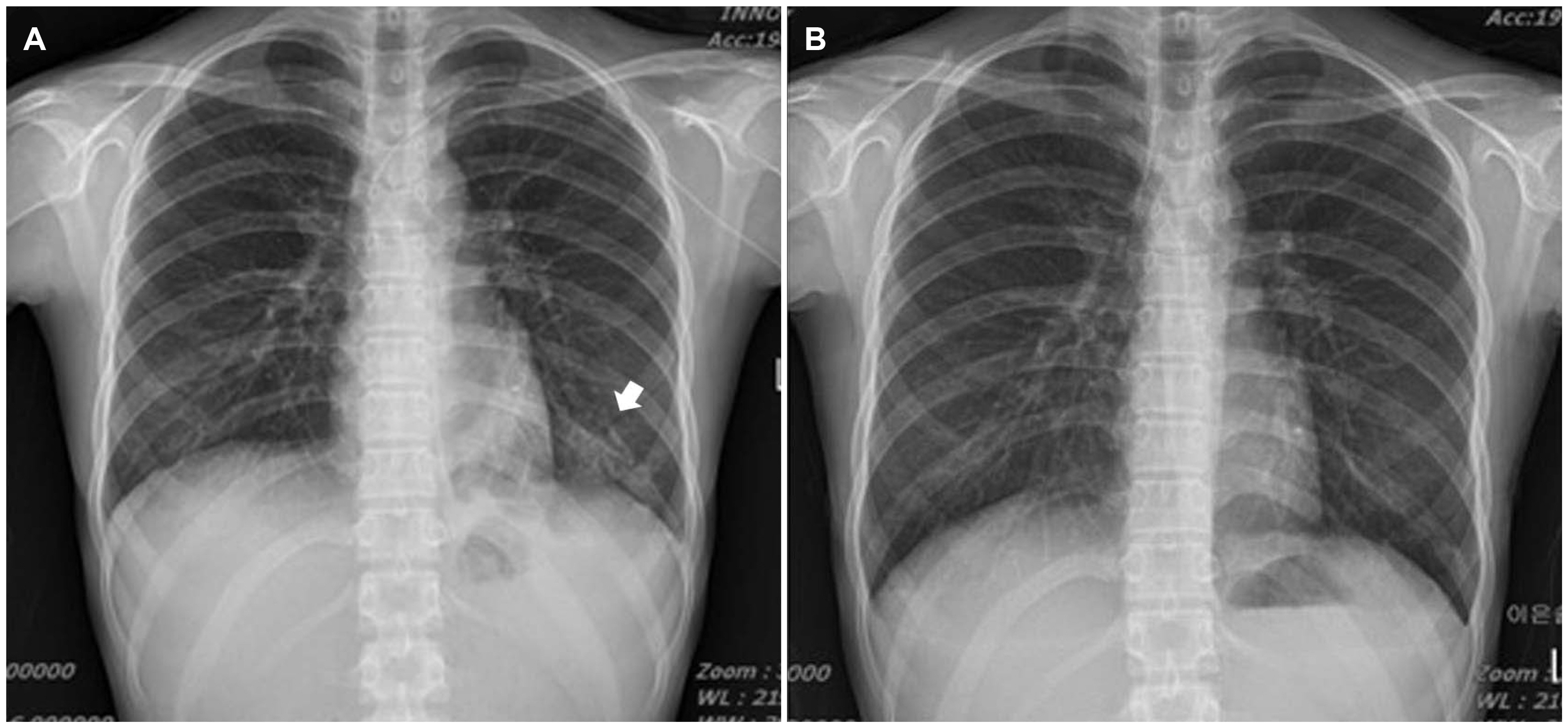
- Differentiating Crohn’s disease (CD) from intestinal tuberculosis (TB) is a challenge. In patients suspected of having CD or intestinal TB compounded with active pulmonary TB in its early stages, clinicians often lean towards a diagnosis of intestinal TB. A 14-year-old female patient was admitted with symptoms of abdominal pain and diarrhea with hematochezia. Colonoscopy revealed a stricture of the ileocecal valve and scattered longitudinal ulcers. Initial chest radiography showed consolidation in the left lower lobe of the lung. Chest CT revealed branching nodular opacities and consolidation. The TB PCR of the bronchial washing fluid was positive. The patient was diagnosed with pulmonary and intestinal TB. The colonoscopy findings favored CD. Despite this, anti-tubercular therapy was initiated based on the radiology findings and PCR test. After treatment with anti-tubercular therapy, the patient’s diarrhea and abdominal pain worsened despite the improvement observed on her chest radiography. Follow-up colonoscopy revealed aggravation of her ulcers. The patient was diagnosed with CD and treated with prednisolone and mesalazine. Her clinical condition improved, and follow-up colonoscopy showed significant improvement of the ulcers. This case highlights the need for caution in diagnosis and suggests that clinicians consider reevaluation in similar cases.
Keyword
Figure
Reference
-
1. Gomollón F, Dignass A, Annese V, et al. 2017; 3rd European evidence-based consensus on the diagnosis and management of crohn's disease 2016: part 1: diagnosis and medical management. J Crohns Colitis. 11:3–25. DOI: 10.1093/ecco-jcc/jjw168. PMID: 27660341.
Article2. Kirsch R, Pentecost M, Hall Pde M, Epstein DP, Watermeyer G, Friederich PW. 2006; Role of colonoscopic biopsy in distinguishing between Crohn's disease and intestinal tuberculosis. J Clin Pathol. 59:840–844. DOI: 10.1136/jcp.2005.032383. PMID: 16873564. PMCID: PMC1860439.
Article3. Ma JY, Tong JL, Ran ZH. 2016; Intestinal tuberculosis and Crohn's disease: challenging differential diagnosis. J Dig Dis. 17:155–161. DOI: 10.1111/1751-2980.12324. PMID: 26854750.
Article4. Sharma MP, Ahuja V. Schaaf HS, Zumla A, Grange JM, editors. 2009. Abdominal tuberculosis in adult. Tuberculosis: a comprehensive clinical reference. Saunders/Elsevier;Edinburgh: p. 424–431. DOI: 10.1016/B978-1-4160-3988-4.00039-1. PMCID: PMC2696123.5. 2017. Global Tuberculosis Report. [Internet]. World Health Organization;Geneva: Available from https://www.who.int/tb/publications/global_report/gtbr2017_ main_text.pdf?u%20a=1. cited 2017 Nov 13.6. Zhao XS, Wang ZT, Wu ZY, et al. 2014; Differentiation of Crohn's disease from intestinal tuberculosis by clinical and CT enterographic models. Inflamm Bowel Dis. 20:916–925. DOI: 10.1097/MIB.0000000000000025. PMID: 24694791.
Article7. Amarapurkar DN, Patel ND, Rane PS. 2008; Diagnosis of Crohn's disease in India where tuberculosis is widely prevalent. World J Gastroenterol. 14:741–746. DOI: 10.3748/wjg.14.741. PMID: 18205265. PMCID: PMC2684002.
Article8. Shepherd NA. 2002; Granulomas in the diagnosis of intestinal Crohn's disease: a myth exploded? Histopathology. 41:166–168. DOI: 10.1046/j.1365-2559.2002.01441.x. PMID: 12147095.9. Kedia S, Das P, Madhusudhan KS, et al. 2019; Differentiating Crohn's disease from intestinal tuberculosis. World J Gastroenterol. 25:418–432. DOI: 10.3748/wjg.v25.i4.418. PMID: 30700939. PMCID: PMC6350172.
Article10. Almadi MA, Ghosh S, Aljebreen AM. 2009; Differentiating intestinal tuberculosis from Crohn's disease: a diagnostic challenge. Am J Gastroenterol. 104:1003–1012. DOI: 10.1038/ajg.2008.162. PMID: 19240705.
Article11. Boudiaf M, Zidi SH, Soyer P, et al. 1998; Tuberculous colitis mimicking Crohn's disease: utility of computed tomography in the differentiation. Eur Radiol. 8:1221–1223. DOI: 10.1007/s003300050539. PMID: 9724443.
Article12. Franco-Paredes C, Díaz-Borjon A, Senger MA, Barragan L, Leonard M. 2006; The ever-expanding association between rheumatologic diseases and tuberculosis. Am J Med. 119:470–477. DOI: 10.1016/j.amjmed.2005.10.063. PMID: 16750957.
Article13. de Visser V, Sotgiu G, Lange C, et al. 2015; False-negative interferon-γ release assay results in active tuberculosis: a TBNET study. Eur Respir J. 45:279–283. DOI: 10.1183/09031936.00120214. PMID: 25359336.
Article14. Ghoshal UC, Ghoshal U, Singh H, Tiwari S. 2007; Anti-Saccharomyces cerevisiae antibody is not useful to differentiate between Crohn's disease and intestinal tuberculosis in India. J Postgrad Med. 53:166–170. DOI: 10.4103/0022-3859.33857. PMID: 17699989.15. Ooi CJ, Makharia GK, Hilmi I, et al. 2016; Asia Pacific Consensus Statements on Crohn's disease. J Gastroenterol Hepatol. 31:45–55. DOI: 10.1111/jgh.12956. PMID: 25819140.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Crohns Disease Misdiagnosed as Intestinal Tuberculosis
- Differentiating between Intestinal Tuberculosis and Crohn’s Disease May Be Complicated by Multidrug-resistant Mycobacterium tuberculosis
- The Diagnostic Value of Polymerase Chain Reaction in Intestinal Tuberculosis
- A Case of Tuberculous Enteritis with Active Pulmonary Tuberculosis in a 12-Year-Old Girl
- A case of intestinal tuberculosis complicated by miliary tuberculosis