J Korean Neurosurg Soc.
2021 Jan;64(1):69-77. 10.3340/jkns.2020.0080.
A New Classification for Cervical Ossification of the Posterior Longitudinal Ligament Based on the Coexistence of Segmental Disc Degeneration
- Affiliations
-
- 1Department of Neurosurgery, Korea University Guro Hospital, Seoul, Korea
- KMID: 2510761
- DOI: http://doi.org/10.3340/jkns.2020.0080
Abstract
Objective
: Classification systems for cervical ossification of the posterior longitudinal ligament (OPLL) have traditionally focused on the morphological characteristics of ossification. Although the classification describes many clinical features associated with the shape of the ossification, including the concept of spondylosis seems necessary because of the similarity in age distribution.
Methods
: Patients diagnosed with OPLL who presented with increase signal intensity (ISI) on magnetic resonance imaging were surgically treated in our department. The patients were divided into two groups (pure versus degenerative) according to the presence of disc degeneration.
Results
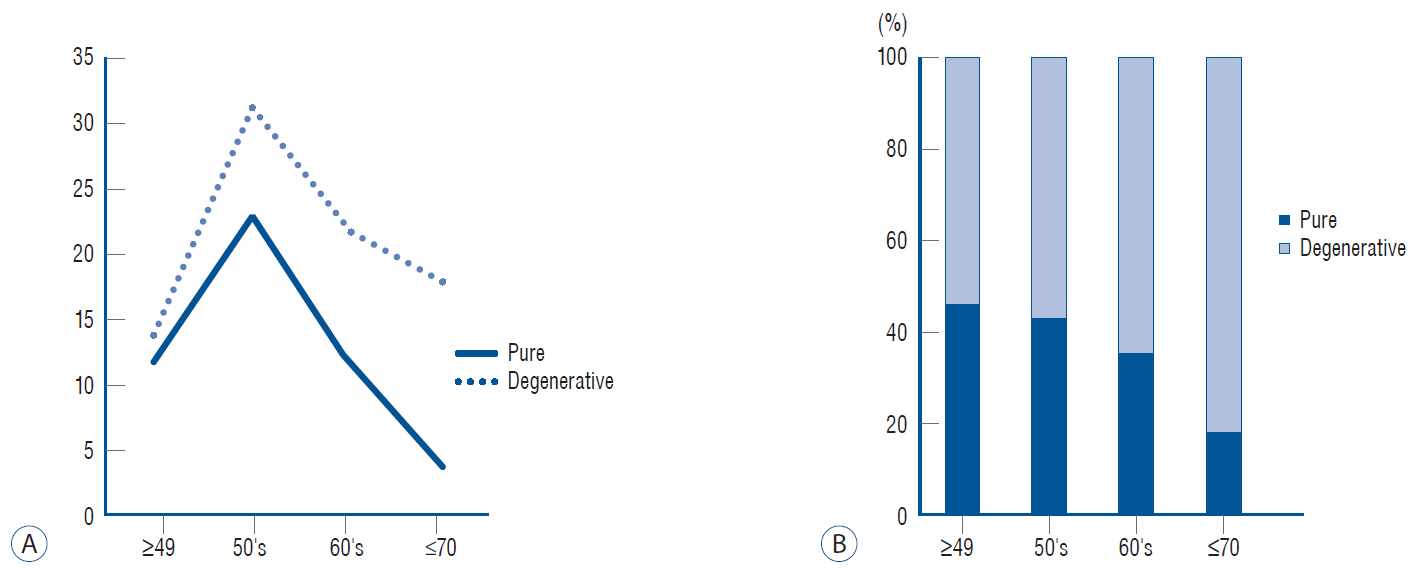
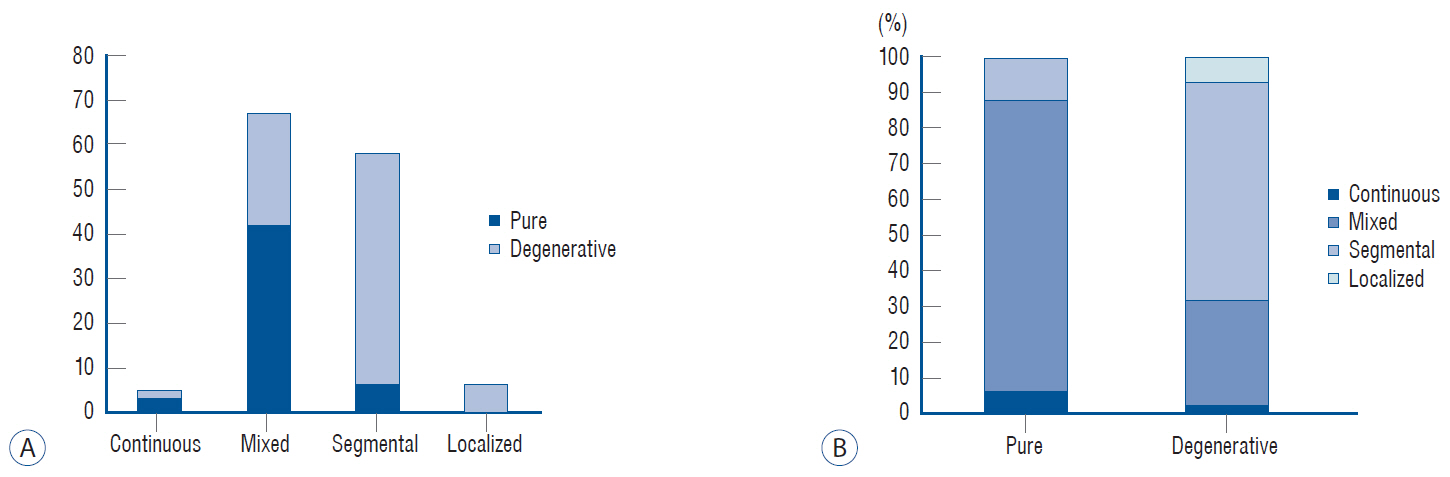
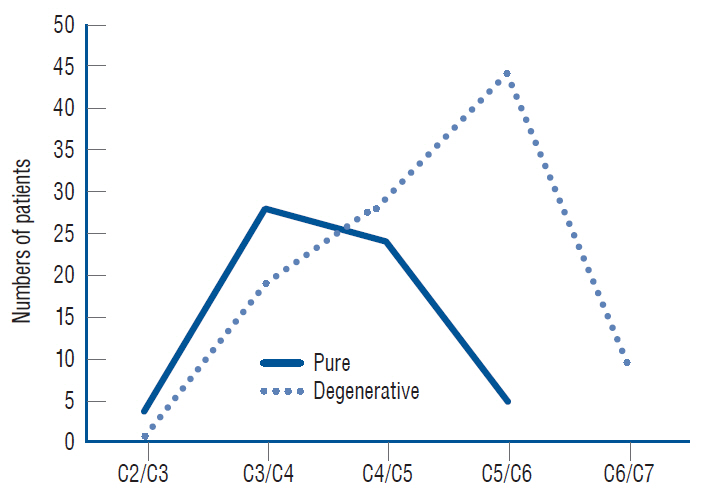
: Of 141 patients enrolled in this study, more than half (61%) were classified into the degenerative group. The pure group showed a profound male predominance, early presentation of myelopathy, and a different predilection for ISI compared to the degenerative group. The mean canal compromise ratio (CC) of the ISI was 47% in the degenerative group versus 61% in the pure group (p<0.0000). On the contrary, the global and segment motions were significantly larger in the degenerative group (p<0.0000 and p=0.003, respectively). The canal diameters and global angles did not differ between groups.
Conclusion
: Classifying cervical OPLL based on the presence of combined disc degeneration is beneficial for understanding the disorder’s behavior. CC appears to be the main factor in the development of myelopathy in the pure group, whereas additional dynamic factors appear to affect its development in the degenerative group.
Keyword
Figure
Reference
-
References
1. Bednarik J, Kadanka Z, Dusek L, Kerkovsky M, Vohanka S, Novotny O, et al. Presymptomatic spondylotic cervical myelopathy: an updated predictive model. Eur Spine J. 17:421–431. 2008.
Article2. Chang H, Song KJ, Kim HY, Choi BW. Factors related to the development of myelopathy in patients with cervical ossification of the posterior longitudinal ligament. J Bone Joint Surg Br. 94:946–949. 2012.
Article3. Chazono M, Tanaka T, Kumagae Y, Sai T, Marumo K. Ethnic differences in pedicle and bony spinal canal dimensions calculated from computed tomography of the cervical spine: a review of the English-language literature. Eur Spine J. 21:1451–1458. 2012.
Article4. Du YQ, Duan WR, Chen Z, Wu H, Jian FZ. Risk factors and management of dural defects in anterior surgery for cervical ossification of the posterior longitudinal ligament. World Neurosurg. 111:e527–e538. 2018.
Article5. Fujiyoshi T, Yamazaki M, Okawa A, Kawabe J, Hayashi K, Endo T, et al. Static versus dynamic factors for the development of myelopathy in patients with cervical ossification of the posterior longitudinal ligament. J Clin Neurosci. 17:320–324. 2010.
Article6. Inamasu J, Guiot BH, Sachs DC. Ossification of the posterior longitudinal ligament: an update on its biology, epidemiology, and natural history. Neurosurgery. 58:1027–1039. discussion 1027-1039. 2006.
Article7. Ito K, Yukawa Y, Machino M, Kobayakawa A, Kato F. Range of motion determined by multidetector-row computed tomography in patients with cervical ossification of the posterior longitudinal ligament. Nagoya J Med Sci. 77:221–228. 2015.8. Kelly JC, Groarke PJ, Butler JS, Poynton AR, O'Byrne JM. The natural history and clinical syndromes of degenerative cervical spondylosis. Adv Orthop. 2012:393642. 2012.
Article9. Matsunaga S, Kukita M, Hayashi K, Shinkura R, Koriyama C, Sakou T, et al. Pathogenesis of myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg. 96(2 Suppl):168–172. 2002.
Article10. Matsunaga S, Nakamura K, Seichi A, Yokoyama T, Toh S, Ichimura S, et al. Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament: a multicenter cohort study. Spine (Phila Pa 1976). 33:2648–2650. 2008.
Article11. Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine (Phila Pa 1976). 37:E309–E314. 2012.12. Matsunaga S, Sakou T, Taketomi E, Komiya S. Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg. 100(3 Suppl Spine):245–248. 2004.
Article13. Morio Y, Nagashima H, Teshima R, Nawata K. Radiological pathogenesis of cervical myelopathy in 60 consecutive patients with cervical ossification of the posterior longitudinal ligament. Spinal Cord. 37:853–857. 1999.
Article14. Onishi E, Sakamoto A, Murata S, Matsushita M. Risk factors for acute cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976). 37:660–666. 2012.
Article15. Park HJ, Jeon JS, Lee PE. Range of motion of cervical spine in normal Korean people. J Korean Soc Spine Surg. 11:83–89. 2004.
Article16. Park YK, Moon HJ, Kwon TH, Kim JH. Long-term outcomes following anterior foraminotomy for one- or two-level cervical radiculopathy. Eur Spine J. 22:1489–1496. 2013.
Article17. Saetia K, Cho D, Lee S, Kim DH, Kim SD. Ossification of the posterior longitudinal ligament: a review. Neurosurg Focus. 30:E1. 2011.
Article18. Sakou T, Matsunaga S, Koga H. Recent progress in the study of pathogenesis of ossification of the posterior longitudinal ligament. J Orthop Sci. 5:310–315. 2000.
Article19. Sugawara T, Itoh Y, Hirano Y, Higashiyama N, Mizoi K. Long term outcome and adjacent disc degeneration after anterior cervical discectomy and fusion with titanium cylindrical cages. Acta Neurochir (Wien). 151:303–309. discussion 309. 2009.
Article20. Tetreault L, Nakashima H, Kato S, Kryshtalskyj M, Nagoshi N, Nouri A, et al. A systematic review of classification systems for cervical ossification of the posterior longitudinal ligament. Global Spine J. 9:85–103. 2019.
Article21. Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 184:71–84. 1984.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ossification of the Posterior Longitudinal Ligament: 2 cases report
- Dysphagia Caused by Ossification of the Cervical Anterior Longitudinal Ligament
- A Case Quadriplegia due to Minor Head Trauma Associated with Ossification of the Posterior Longitudinal Ligament of the Cervical Spine
- Does Ossification of the Posterior Longitudinal Ligament Progress after Fusion?
- Anterior Decompression and Interbody Fusion for Ossification of the Posterior Longitudinal Ligament of the Cervical Spine: Case Report