Factors Associated with Awareness, Treatment, and Control Rate of Hypertension among Korean Young Adults Aged 30–49 Years
- Affiliations
-
- 1Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Cardiovascular and Metabolic Diseases Etiology Research Center, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2509027
- DOI: http://doi.org/10.4070/kcj.2020.0208
Abstract
- Background and Objectives
Hypertension awareness, treatment, and control have been substantially improved in the last decades worldwide, but hypertension management in younger adults is still challenged. We analyzed a nationally representative sample of Korea to investigate factors affecting hypertension management among the young Korean population.
Methods
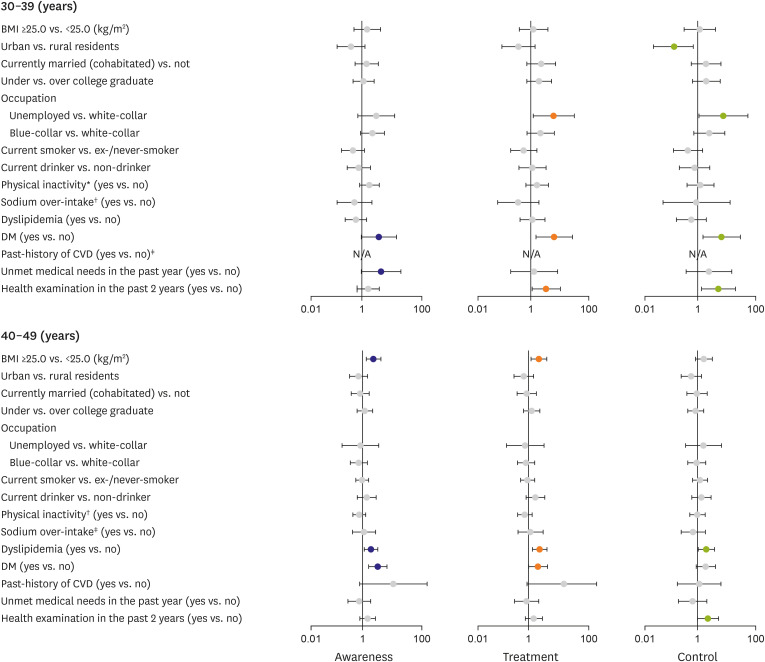
Among 8,024 young adults aged 30–49 years from the 2014–2018 Korea National Health and Nutrition Examination Survey, 1,103 participants with hypertension were analyzed to identify factors associated with hypertension management status. Multiple logistic regression models were conducted separately by sex.
Results
Young adults with hypertension showed a low rate of awareness (35.8%), treatment (30.9%), and control (23.0%). The older age (40–49 years), obese (body mass index ≥25.0 kg/ m 2 ), having diabetes mellitus (DM), and having past-history of cardiovascular disease were positively associated with awareness, and taking health examination in the past 2 years were positively associated with both treatment and control of hypertension among male. Young females who were older (40–49 years), rural residents, unemployed, not taking sodium over the recommended amount, having dyslipidemia, and having DM showed a higher likelihood of awareness. Young females who have not experienced unmet medical needs in the past year were more likely to be treated or controlled with hypertension.
Conclusions
The factors associated with hypertension awareness, treatment, and control were different by sex and age group. Enhancing attention on hypertension among young hypertension and encouraging them to visit clinics would be key strategies to improve hypertension management among the young hypertensive population.
Figure
Cited by 6 articles
-
Hypertension Control in Young Population: the Earlier, the Better
Wook Bum Pyun
Korean Circ J. 2020;50(12):1092-1094. doi: 10.4070/kcj.2020.0427.Suboptimal Management Status of Younger Hypertensive Population in Korea
Hae-Young Lee, Gyu Chul Oh, Il Suk Sohn, Sungha Park, Jinho Shin, Wook Bum Pyun, Myeong-Chan Cho
Korean Circ J. 2021;51(7):598-606. doi: 10.4070/kcj.2020.0542.Solvitur Ambulando: Importance of Exercise in Middle-Age for Cardiovascular Health
Hae-Young Lee
Korean Circ J. 2021;51(11):936-938. doi: 10.4070/kcj.2021.0308.The Advent of Cuffless Mobile Device Blood Pressure Measurement: Remaining Challenges and Pitfalls
Hae-Young Lee, Thilo Burkard
Korean Circ J. 2022;52(3):198-204. doi: 10.4070/kcj.2021.0405.Reimbursement of Digital Therapeutics: Future Perspectives in Korea
Jin Han Ju, Boram Sim, Jeongeun Lee, Jin Yong Lee
Korean Circ J. 2022;52(4):265-279. doi: 10.4070/kcj.2022.0014.Development of a Zebrafish Larvae Model for Diabetic Heart Failure With Reduced Ejection Fraction
Inho Kim, Seung Hyeok Seok, Hae-Young Lee
Korean Circ J. 2022;53(1):34-46. doi: 10.4070/kcj.2022.0210.
Reference
-
1. NCD Risk Factor Collaboration (NCD-RisC). Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019; 394:639–651. PMID: 31327564.2. Cho SM, Lee H, Kim HC. Comparison and implication of the contemporary blood pressure guidelines on Korean population. Korean Circ J. 2020; 50:485–498. PMID: 32212423.
Article3. Kim HC, Ihm SH, Kim GH, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology of hypertension. Clin Hypertens. 2019; 25:16. PMID: 31388451.
Article4. Korean Society Hypertension (KSH). Hypertension Epidemiology Research Working Group. Kim HC, Cho MC. Korea hypertension fact sheet 2018. Clin Hypertens. 2018; 24:13. PMID: 30288297.
Article5. Kjeldsen S, Feldman RD, Lisheng L, et al. Updated national and international hypertension guidelines: a review of current recommendations. Drugs. 2014; 74:2033–2051. PMID: 25315030.
Article6. Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77. PMID: 24585853.
Article7. Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012; 60:599–606. PMID: 22796254.
Article8. Li D, Lv J, Liu F, et al. Hypertension burden and control in mainland China: analysis of nationwide data 2003-2012. Int J Cardiol. 2015; 184:637–644. PMID: 25771229.
Article9. Ueshima H, Zhang XH, Choudhury SR. Epidemiology of hypertension in China and Japan. J Hum Hypertens. 2000; 14:765–769. PMID: 11095166.
Article10. Moon JY, Park KJ, Hwangbo Y, et al. A trend analysis of the prevalence, awareness, treatment, and control of hypertension by age group. J Prev Med Public Health. 2013; 46:353–359. PMID: 24349657.
Article11. Kang SH, Kim SH, Cho JH, et al. Prevalence, awareness, treatment, and control of hypertension in Korea. Sci Rep. 2019; 9:10970. PMID: 31358791.
Article12. De Venecia T, Lu M, Figueredo VM. Hypertension in young adults. Postgrad Med. 2016; 128:201–207. PMID: 26821528.
Article13. Ostchega Y, Zhang G, Hughes JP, Nwankwo T. Factors associated with hypertension control in US adults using 2017 ACC/AHA guidelines: National Health and Nutrition Examination Survey 1999-2016. Am J Hypertens. 2018; 31:886–894. PMID: 29617894.
Article14. Park JE, Park JH, Chang SJ, Lee JH, Kim SY. The determinants of and barriers to awareness and treatment of hypertension in the Korean population. Asia Pac J Public Health. 2019; 31:121–135. PMID: 30678483.
Article15. Satoh A, Arima H, Ohkubo T, et al. Associations of socioeconomic status with prevalence, awareness, treatment, and control of hypertension in a general Japanese population: NIPPON DATA2010. J Hypertens. 2017; 35:401–408. PMID: 28005709.16. Hanyang University College of Medicine. Report: Quality Control and Assurance of Blood Pressure Measurement: KNHANES 6 (2014). Cheongju: KCDC;2014.17. Hanyang University College of Medicine. Report: Quality Control and Assurance of Blood Pressure Measurement: KNHANES 7 (2018). Cheongju: KCDC;2018.18. World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications Australia;2000.19. World Health Organization. Global Recommendations on Physical Activity for Health. Geneva: WHO;2010.20. World Health Organization. Prevention of Cardiovascular Disease. Geneva: WHO;2007.21. Lee MH, Kim HC, Ahn SV, et al. Prevalence of dyslipidemia among Korean adults: Korea National Health and Nutrition Survey 1998-2005. Diabetes Metab J. 2012; 36:43–55. PMID: 22363921.22. Choi HM, Kim HC, Kang DR. Sex differences in hypertension prevalence and control: analysis of the 2010-2014 Korea National Health and Nutrition Examination Survey. PLoS One. 2017; 12:e0178334. PMID: 28542557.
Article23. Everett B, Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemogr Soc Biol. 2015; 61:1–17.
Article24. Johnson HM, Warner RC, LaMantia JN, Bowers BJ. “I have to live like I'm old.” Young adults' perspectives on managing hypertension: a multi-center qualitative study. BMC Fam Pract. 2016; 17:31. PMID: 26969619.
Article25. Wu Y, Tai ES, Heng D, Tan CE, Low LP, Lee J. Risk factors associated with hypertension awareness, treatment, and control in a multi-ethnic Asian population. J Hypertens. 2009; 27:190–197. PMID: 19145784.
Article26. Ostchega Y, Hughes JP, Wright JD, McDowell MA, Louis T. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens. 2008; 21:159–165. PMID: 18188162.
Article27. Johnson HM, Warner RC, Bartels CM, LaMantia JN. “They're younger… it's harder.” Primary providers' perspectives on hypertension management in young adults: a multicenter qualitative study. BMC Res Notes. 2017; 10:9. PMID: 28057065.
Article28. Li T, Song X, Wu J, et al. Awareness of hypertension and related factors in northeastern China: a cross-sectional study. J Hum Hypertens. 2020; 34:43–50. PMID: 31548618.
Article29. Cho E, Lee CY, Kim I, et al. Factors influencing medication adherence in patients with hypertension: based on the 2008 Korean National Health and Nutrition Examination Survey. J Korean Acad Community Health Nurs. 2013; 24:419–426.
Article30. Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016; 388:2665–2712. PMID: 27671667.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and management of hypertension in Korean adults
- Suboptimal control status of young hypertensive population
- Management Status of Cardiovascular Disease Risk Factors for Dyslipidemia among Korean Adults
- Awareness, Treatment, and Control Rates of Hypertension and Related Factors of Awareness among Middle Aged Adult and Elderly in Chuncheon: Hallym Aging Study(HAS)
- Awareness, Treatment and Control of Hypertension and Related Factors in the Jurisdictional Areas of Primary Health Care Posts in a Rural Community of Korea