Arch Hand Microsurg.
2020 Dec;25(4):320-325. 10.12790/ahm.20.0058.
Successful Microsurgical Replantation of Scalp Amputation Using Medicinal and Chemical Leech Therapy: A Case Report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2508948
- DOI: http://doi.org/10.12790/ahm.20.0058
Abstract
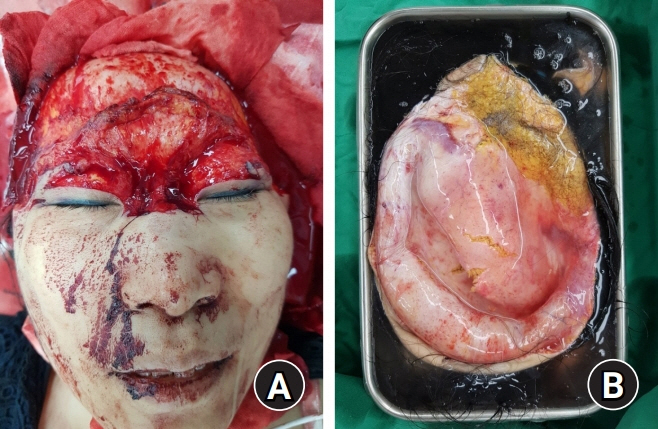
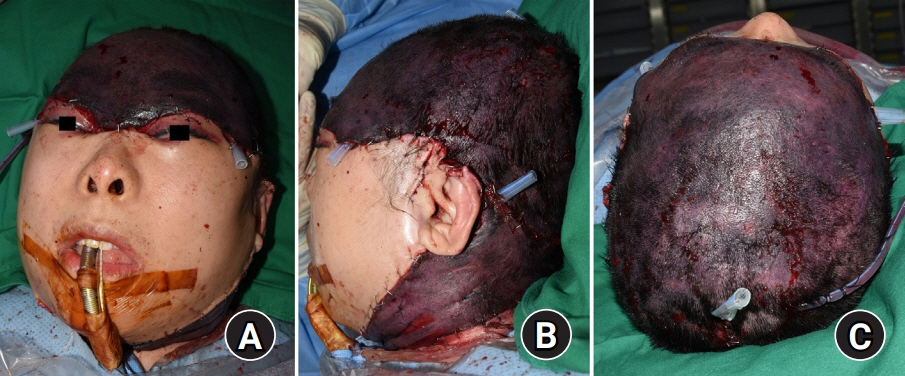
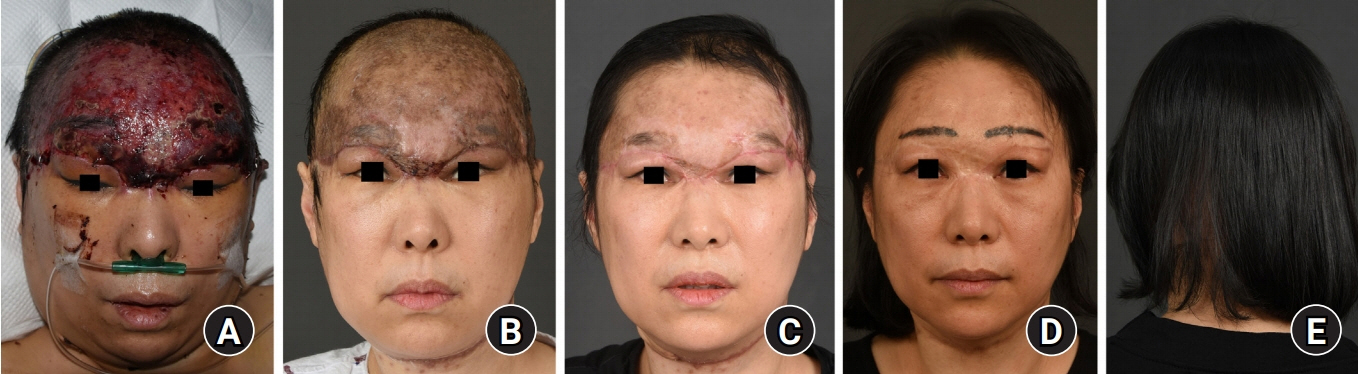
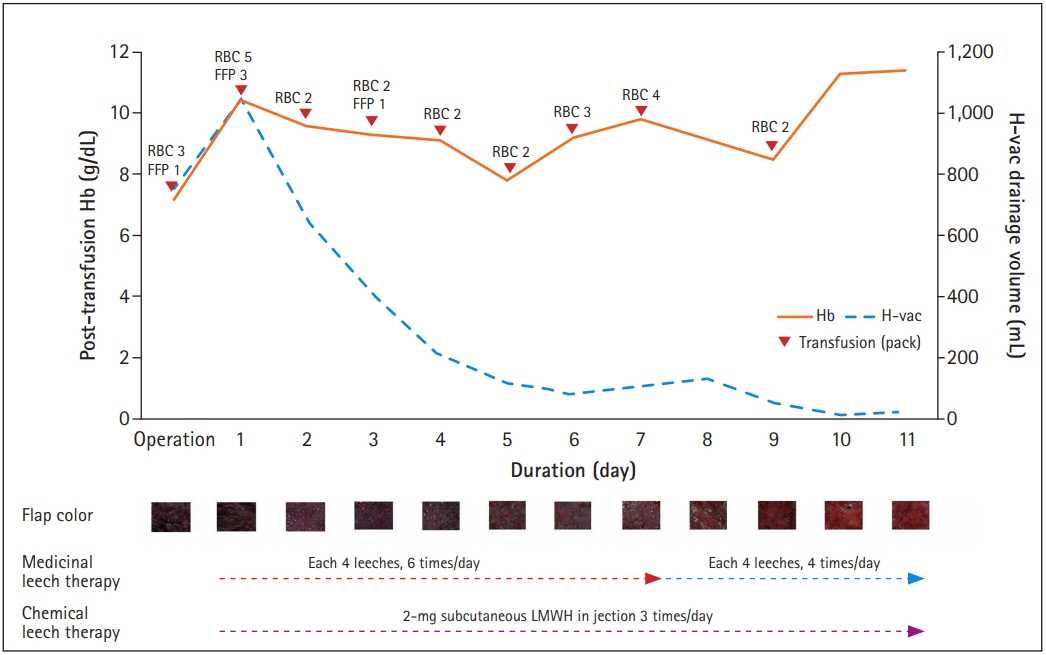
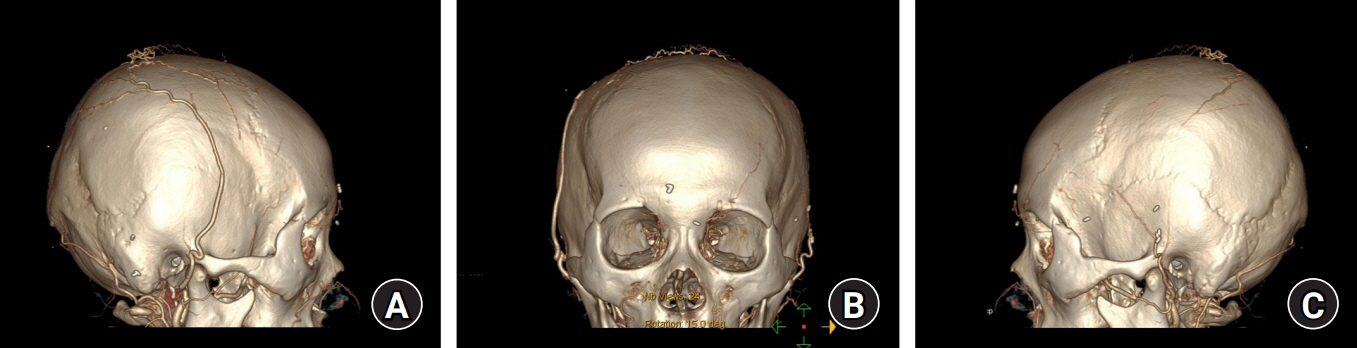
- Scalp amputation is a very rare occurrence worldwide. In particular, replantation failure may occur from venous congestion, which represents a major complication of replantation. Accordingly, this study reports on a scalp amputation case with successful replantation treatment using medicinal and chemical leech therapy. On November 11, 2017, a 47-year-old female patient experienced a complete amputation injury starting from the top of the nose involving the total scalp by rolling machine that packs laundry. Severe venous congestion was controlled by medicinal leech therapy performed six times a day and chemical leech therapy (subcutaneous low-molecular-weight heparin injection) three times a day for 10 days. Approximately 85% of the scalp was replanted, and hair growth was confirmed. The basic concept of replantation surgery, “replace tissue with like tissue,” makes replacement impossible with tissues other than the hair-bearing scalp. Accordingly, the authors present a case of successful replantation with both medicinal and chemical leech therapy.
Keyword
Figure
Reference
-
1. Miller GD, Anstee EJ, Snell JA. Successful replantation of an avulsed scalp by microvascular anastomoses. Plast Reconstr Surg. 1976; 58:133–6.
Article2. Cheng K, Zhou S, Jiang K, et al. Microsurgical replantation of the avulsed scalp: report of 20 cases. Plast Reconstr Surg. 1996; 97:1099–106.3. Barisoni D, Lorenzini M, Governa M. Two cases of scalp reimplantation based on one artery and one vein with interposed vein grafts. Eur J Plast Surg. 1997; 20:51–3.
Article4. Herrera F, Buntic R, Brooks D, Buncke G, Antony AK. Microvascular approach to scalp replantation and reconstruction: a thirty-six year experience. Microsurgery. 2012; 32:591–7.
Article5. Ding W, Liu M, Chen L, Xu L, Rui Y, Gu Y. Treatment of total scalp avulsion by an advanced microsurgical method involving the subcutaneous tissue suspension by the tight suture of scalp tissue around anastomotic stoma. J Craniofac Surg. 2015; 26:579–81.
Article6. Jin Y, Hua C, Hu X, et al. Microsurgical replantation of total avulsed scalp: extending the limits. J Craniofac Surg. 2017; 28:670–4.7. Nguyen HH. The microsurgical replantation of seven complete scalp avulsions: is one artery sufficient? J Plast Reconstr Aesthet Surg. 2012; 65:1639–44.
Article8. Nguyen MQ, Crosby MA, Skoracki RJ, Hanasono MM. Outcomes of flap salvage with medicinal leech therapy. Microsurgery. 2012; 32:351–7.
Article9. Barnett GR, Taylor GI, Mutimer KL. The “chemical leech”: intra-replant subcutaneous heparin as an alternative to venous anastomosis: report of three cases. Br J Plast Surg. 1989; 42:556–8.
Article10. Pérez M, Sancho J, Ferrer C, García O, Barret JP. Management of flap venous congestion: the role of heparin local subcutaneous injection. J Plast Reconstr Aesthet Surg. 2014; 67:48–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microsurgical Replantation of the Amputated Ear without Venous Repair: Clinical Experience with Leech
- Replantation of a Completely Amputated Penis, which Occurred in a Child during Circumcision
- Replantation of Nose Amputation by Use of Medical Leech
- Treatment of Complete Scalp Avulsion with the Conditions of Unstable Vital Signs: A Case Report
- A Case of Successful Penile Replantation