Arch Hand Microsurg.
2020 Dec;25(4):292-296. 10.12790/ahm.20.0061.
Case of Treatment of Snakebite on Finger with Topical Oxygen Therapy
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- KMID: 2508943
- DOI: http://doi.org/10.12790/ahm.20.0061
Abstract
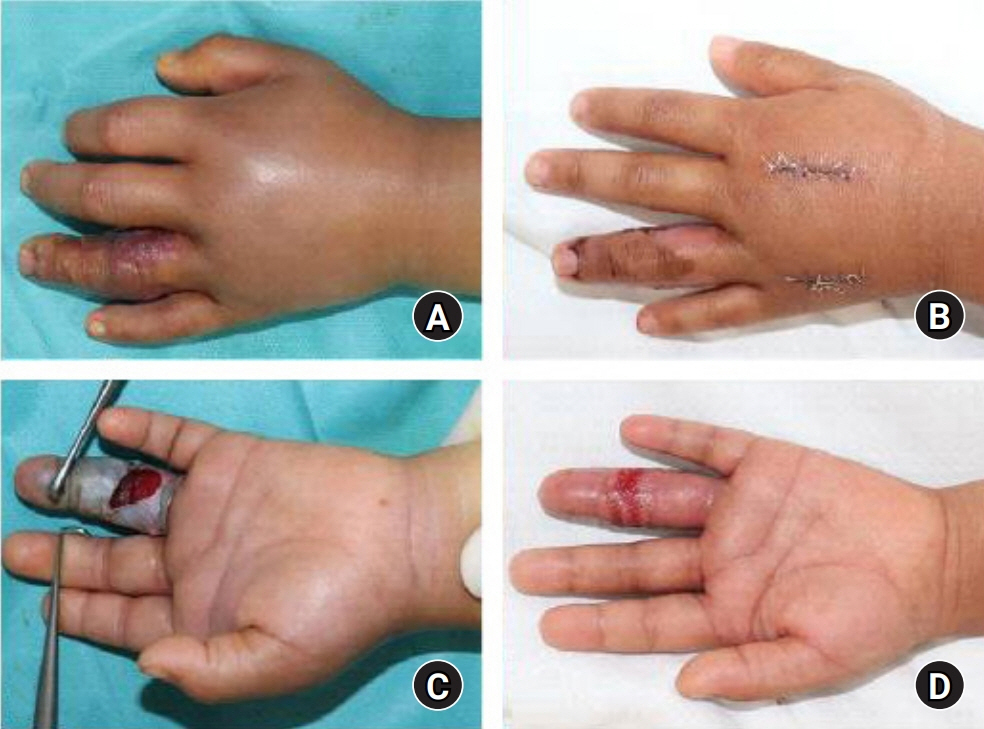
- Snakebites, though uncommon, are a potentially serious cause of disability or death. Local symptoms may include pain, edema, or ecchymosis that may progress to skin necrosis or compartment syndrome. This study explores the case of a 4-year-old male patient bitten by a snake on the distal volar aspect of his left ring finger. On physical examination, there were moderate swelling, hemobullae formation, and the skin necrosis was progressing on middle phalanx of ring finger. Fasciotomy and topical oxygen therapy was performed. The topical oxygen therapy (TOT) was started once a day for 90 minutes with 4 L/minute of oxygen flow. TOT is a method of delivering humidified oxygen directly to the wound bed to support the healing of chronic and hypoxic wounds. There is no report on TOT for snakebite injury. In this report, we would like to report on the clinical experience of early surgery and adjuvant TOT with literary consideration.
Keyword
Figure
Cited by 1 articles
-
Treatment of a rattlesnake bite on the finger using alternative antivenom management and reconstructive surgery: a case report
Kyong Chan Park, Chang Yong Choi, Seung Min Nam, Eun Soo Park
Arch Hand Microsurg. 2022;27(2):161-165. doi: 10.12790/ahm.22.0008.
Reference
-
1. Russell FE. Snake venom poisoning in the United States. Annu Rev Med. 1980; 31:247–59.
Article2. Kasturiratne A, Wickremasinghe AR, de Silva N, et al. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008; 5:e218.
Article3. Shin CS, Bae JS, Sohn KS. Clinical analysis on venomous snake bite in Korea. J Korean Surg Soc. 1984; 27:245–54.4. Lee BJ, Hong SI, Kim HS, et al. Hematological features of coagulopathy and the efficacy of antivenin therapy for a Korean snakebite. J Korean Surg Soc. 2007; 72:18–26.5. Orsted HL, Poulson R; Advisory Group, et al. Evidence-based practice standards for the use of topical pressurised oxygen therapy. Int Wound J. 2012; 9:271–84.
Article6. Rha JH, Kwon SM, Oh JR, Han BK, Lee KH, Kim JH. Snakebite in Korea: a guideline to primary surgical management. Yonsei Med J. 2015; 56:1443–48.
Article7. Pang HN, Teoh LC, Yam AK, Lee JY, Puhaindran ME, Tan AB. Factors affecting the prognosis of pyogenic flexor tenosynovitis. J Bone Joint Surg Am. 2007; 89:1742–8.
Article8. Fries R, Wallace W, Roy S, et al. Dermal excsional wound healing in pigs following treatment with topically applied pure oxygen. Mutat Res. 2005; 579:172–81.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Condyloma Acuminata Treated with Topical Photodynamic Therapy
- A Case of Actinic Keratosis Treated by Topical Photodynamic Therapy with Low Intensity Dye Laser
- Topical Hyperbaric Oxygen Therapy on Composite Graft & Local Flap on Facial Area
- Oxygen therapy for sepsis and prevention of complications
- Clinical Significance of Delayed re-evaluation in Initial Symptoms Following Snakebite Injury