Ann Surg Treat Res.
2020 Dec;99(6):329-336. 10.4174/astr.2020.99.6.329.
What is the better surgical treatment option for recurrent common bile duct stones?
- Affiliations
-
- 1Digestive Disease Center, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 2Department of General Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 3Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 4Department of Internal Medicine, Gachon Gil Hospital, Gachon University College of Medicine, Incheon, Korea
- 5Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 6Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea
- 7Department of Internal Medicine, Inha University School of Medicine, Incheon, Korea
- KMID: 2508932
- DOI: http://doi.org/10.4174/astr.2020.99.6.329
Abstract
- Purpose
Repeating endoscopic retrograde cholangiopancreatography (ERCP) in patients with recurrent common bile duct (CBD) stones is problematic in many ways. Choledochoduodenostomy (CDS) and choledochojejunostomy (CJS) are 2 surgical treatment options for recurrent CBD stones, and each has different advantages and disadvantages. The aim of this study was to compare the 2 surgical options in terms of the recurrence rate of CBD stones after surgical treatment.
Methods
This retrospective multicenter study included all patients who underwent surgical treatment due to recurrent CBD stones that were not effectively controlled by medical treatment and repeated ERCP between January 2006 and March 2015. We collected data from chart reviews and medical records. A recurrent CBD stone was defined as a stone found 6 months after the complete removal of a CBD stone by ERCP. Patients who underwent surgery for other reasons were excluded.
Results
A total of 27 patients were enrolled in this study. Six patients underwent CDS, and 21 patients underwent CJS for the rescue treatment of recurrent CBD stones. The median follow-up duration was 290 (180–1,975) days in the CDS group and 1,474 (180–6,560) days in the CJS group (P = 0.065). The postoperative complications were similar and tolerable in both groups (intestinal obstruction; 2 of 27, 7.4%; 1 in each group). CBD stones recurred in 4 patients after CDS (4 of 6, 66.7%), and 3 patients after CJS (3 of 21, 14.3%) (P = 0.010).
Conclusion
CJS may be a better surgical option than CDS for preventing further stone recurrence in patients with recurrent CBD stones.
Keyword
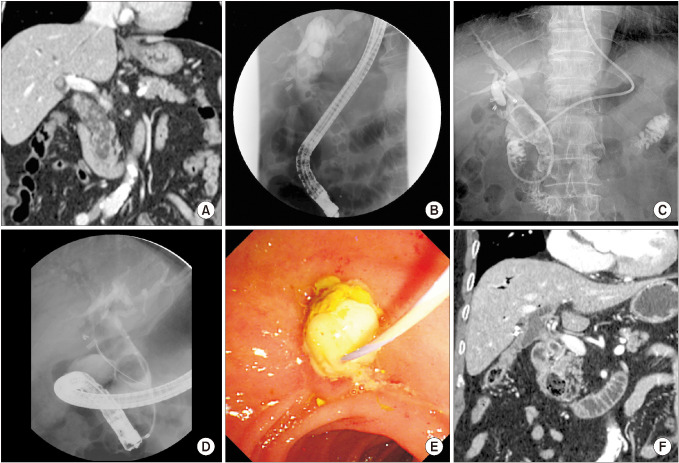
Figure
Reference
-
1. Keizman D, Shalom MI, Konikoff FM. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg Endosc. 2006; 20:1594–1599. PMID: 16858527.2. Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918. PMID: 8782497.3. Hawes RH, Cotton PB, Vallon AG. Follow-up 6 to 11 years after duodenoscopic sphincterotomy for stones in patients with prior cholecystectomy. Gastroenterology. 1990; 98:1008–1012. PMID: 2311858.4. Prat F, Malak NA, Pelletier G, Buffet C, Fritsch J, Choury AD, et al. Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology. 1996; 110:894–899. PMID: 8608900.5. Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, et al. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003; 52:116–121. PMID: 12477771.6. Pereira-Lima JC, Jakobs R, Winter UH, Benz C, Martin WR, Adamek HE, et al. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998; 48:457–464. PMID: 9831832.7. Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccalà G, Perri V. Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy. 2002; 34:273–279. PMID: 11932781.8. Lai KH, Peng NJ, Lo GH, Cheng JS, Huang RL, Lin CK, et al. Prediction of recurrent choledocholithiasis by quantitative cholescintigraphy in patients after endoscopic sphincterotomy. Gut. 1997; 41:399–403. PMID: 9378399.9. Cetta F. The role of bacteria in pigment gallstone disease. Ann Surg. 1991; 213:315–326. PMID: 2009013.10. Bowser L, Schutz SM. The role of surveillance endoscopic retrograde cholangiopancreatography in preventing episodic cholangitis in patients with recurrent common bile duct stones. Gastrointest Endosc. 2000; 51:247–248. PMID: 10702020.11. Sugiyama M, Suzuki Y, Abe N, Masaki T, Mori T, Atomi Y. Endoscopic retreatment of recurrent choledocholithiasis after sphincterotomy. Gut. 2004; 53:1856–1859. PMID: 15542528.12. Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M, et al. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008; 57:1004–1021. PMID: 18321943.13. Geenen DJ, Geenen JE, Jafri FM, Hogan WJ, Catalano MF, Johnson GK, et al. The role of surveillance endoscopic retrograde cholangiopancreatography in preventing episodic cholangitis in patients with recurrent common bile duct stones. Endoscopy. 1998; 30:18–20. PMID: 9548038.14. Kummerow KL, Shelton J, Phillips S, Holzman MD, Nealon W, Beck W, et al. Predicting complicated choledocholithiasis. J Surg Res. 2012; 177:70–74. PMID: 22682715.15. Uchiyama K, Onishi H, Tani M, Kinoshita H, Kawai M, Ueno M, et al. Long-term prognosis after treatment of patients with choledocholithiasis. Ann Surg. 2003; 238:97–102. PMID: 12832971.16. Matsushima K, Soybel DI. Operative management of recurrent choledocholithiasis. J Gastrointest Surg. 2012; 16:2312–2317. PMID: 22907776.17. Blankensteijn JD, Terpstra OT. Early and late results following choledochoduodenostomy and choledochojejunostomy. HPB Surg. 1990; 2:151–158. PMID: 2278911.18. Yoon H, Kwon CI, Jeong S, Lee TH, Han JH, Song TJ, et al. Clinical significance of biliary dilatation and cholelithiasis after subtotal gastrectomy. Korean J Gastroenterol. 2015; 66:33–40. PMID: 26194127.19. Panis Y, Fagniez PL, Brisset D, Lacaine F, Levard H, Hay JM. Long term results of choledochoduodenostomy versus choledochojejunostomy for choledocholithiasis. The French Association for Surgical Research. Surg Gynecol Obstet. 1993; 177:33–37. PMID: 8322146.20. Li ZF, Chen XP. Recurrent lithiasis after surgical treatment of elderly patients with choledocholithiasis. Hepatobiliary Pancreat Dis Int. 2007; 6:67–71. PMID: 17287170.21. Groen AK, Out T, Huibregtse K, Delzenne B, Hoek FJ, Tytgat GN. Characterization of the content of occluded biliary endoprostheses. Endoscopy. 1987; 19:57–59. PMID: 3106022.22. Weickert U, Venzke T, König J, Janssen J, Remberger K, Greiner L. Why do bilioduodenal plastic stents become occluded? A clinical and pathological investigation on 100 consecutive patients. Endoscopy. 2001; 33:786–790. PMID: 11558033.23. Kwon CI, Gromski MA, Sherman S, Easler JJ, El Hajj II, Watkins J, et al. Time sequence evaluation of biliary stent occlusion by dissection analysis of retrieved stents. Dig Dis Sci. 2016; 61:2426–2435. PMID: 27154511.24. Narayanan SK, Chen Y, Narasimhan KL, Cohen RC. Hepaticoduodenostomy versus hepaticojejunostomy after resection of choledochal cyst: a systematic review and meta-analysis. J Pediatr Surg. 2013; 48:2336–2342. PMID: 24210209.25. Patil V, Kanetkar V, Talpallikar MC. Hepaticoduodenostomy for biliary reconstruction after surgical resection of choledochal cyst: a 25-year experience. Indian J Surg. 2015; 77:240–244. PMID: 26730001.26. Takada K, Hamada Y, Watanabe K, Tanano A, Tokuhara K, Kamiyama Y. Duodenogastric reflux following biliary reconstruction after excision of choledochal cyst. Pediatr Surg Int. 2005; 21:1–4. PMID: 15480709.27. Santore MT, Behar BJ, Blinman TA, Doolin EJ, Hedrick HL, Mattei P, et al. Hepaticoduodenostomy vs hepaticojejunostomy for reconstruction after resection of choledochal cyst. J Pediatr Surg. 2011; 46:209–213. PMID: 21238669.28. Mukhopadhyay B, Shukla RM, Mukhopadhyay M, Mandal KC, Mukherjee PP, Roy D, et al. Choledochal cyst: a review of 79 cases and the role of hepaticodochoduodenostomy. J Indian Assoc Pediatr Surg. 2011; 16:54–57. PMID: 21731232.29. Shimotakahara A, Yamataka A, Yanai T, Kobayashi H, Okazaki T, Lane GJ, et al. Roux-en-Y hepaticojejunostomy or hepaticoduodenostomy for biliary reconstruction during the surgical treatment of choledochal cyst: which is better? Pediatr Surg Int. 2005; 21:5–7. PMID: 15372285.30. Hamada Y, Hamada H, Shirai T, Nakamura Y, Sakaguchi T, Yanagimoto H, et al. Duodenogastric regurgitation in hepaticoduodenostomy after excision of congenital biliary dilatation (choledochal cyst). J Pediatr Surg. 2017; 52:1621–1624. PMID: 28410789.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Surgery for Common Bile Duct Stone
- Recent Advances in the Management of Recurrent Bile Duct Stones
- Need to identify the risk factor for stone recurrence after common bile duct exploration
- Clinical Significance of Periampullary Diverticulum (Pad) on Recurrent Common Bile Duct Stones
- Application of Electrohydraulic Lithotripsy for Bile Duct Stones Difficult to Remove